Low back pain (LBP) is one of the highest prevalence problems of public health. LBP affects up to 85% people worldwide. Somebody will be affected at less in one point of his life. LBP represent an enormous economic burden on society; its total cost includes: Direct medical costs, work absenteeism, insurance, lost production and disability benefits. Current treatments range from bed rest, physiotherapy, oral analgesic, muscle relaxants, injection of corticosteroids, local anesthetic, surgery, cell based therapies aiming repair a herniated intervertebral disc and an emerging technique which use injectable hydrogels to restore disc height and function.
It was to show treatment methodology, its accuracy and health satisfaction in patients who developed LBP.
1,000 patients were subject to a treatment which consists of a combination of three therapies: Physic therapy, ozone and intravenous injections.
This method achieves decreases 4 points in a visual analogic scale (VAS) over 12 weeks without medication. It has a rate success of 73%. This methodology may be an applicable and useful tool to avoid the surgery in those patients who present an episode of LBP.
Randomized comparative trials are needed to further evaluate if our treatment is superior to lumbar disc surgery.
Lumbalgia, Bulging disc, Disc hernia, Homeopathy, Homotoxicology, Extrusion
Low back pain (LBP) is one of the highest prevalence problems of public health. LBP affects up to 85% people worldwide. Somebody will be affected at less in one point of his life, approximately 15% of them turn on chronic [1]. LBP is considered as chronic if persists more than 12 weeks [2]. Development of chronic LBP is normally caused by somatic and physiological factors [3]. Somatic causes are considered: Psychosocial environment at work, psychological demand and control over the own work. As physiological factor, there is a strong association with disc degeneration, and in less frequency, are inflammatory, tumoral, metabolic and infectious factors [4]. The most common disc disorder is herniated or prolapsed intervertebral disc. In this case, the disc bulge o rupture (rather partially or totally) posteriorly or posterolateral and press on the nerve roots in the spinal canal. Disc herniation is almost always a result of mechanical induced rupture [5]. Other studies have been demonstrated the presence of genetic factors as triggers to development of LBP [6]. Independently of its origin, LBP represent an enormous economic burden on society; its total cost includes: Direct medical costs, work absenteeism, insurance, lost production and disability benefits. Current treatments range from bed rest, physiotherapy, oral analgesic, muscle relaxants, injection of corticosteroids, local anesthetic, surgery [7], cell based therapies aiming repair a herniated intervertebral disc [8] and an emerging technique which use injectable hydrogels to restore disc height and function [9]. Without mention empirical treatments based only in anecdotal statements, which lack of scientific methodology. However, these techniques are tested in a pre-selected population with a high prior probability of treatment success. Nonetheless, these trials use a limited number of patients, leading to controversy and uncertainty about their effectivity. Thus, there is a need to test all treatment in a largest cohort [10].
The Spine Center, at Guadalajara Mexico has developed a method which combines conventional medicine, complementary medicine, physiotherapy and homotoxicology to treat patients with LBP. The aim of this study was show treatment methodology, its accuracy and health satisfaction in patients who developed LBP.
This is a retrospective observational study. All the interventions are standard procedures applied in typical physiotherapy sessions; thus, no institutional or ethical review board approval is required in Mexico. Patients with LBP who attended consultation at the Spine Center in Guadalajara, Mexico, from July 25, 2007 to September 1, 2016 were included in the study. Personal data, age, size, weight and clinical story were recovered. Patients with spine surgery, disc prosthesis, diabetes, neoplasia, or any other reported sickness were not included.
Pain intensity was measured by visual analogic scale (VAS) from 0 (no pain) to 10 (worst pain) [11]. Two VAS were registered for statistical analysis propose; first at the beginning without any treatment (VAS input) and the second after treatment (VAS output). Treatment was considered successful if VAS input - VAS output ≥ 4 (ΔVAS ≥ 4), was constant over 12 weeks [12].
Body mass index (BMI) was estimated with the formula BMI = weight/height2 then patients were classified as follow: Severe thinness (< 16.00); moderate thinness (16.00-16.99); light thinness (17.00-18.48); normal (18.50-24.99); pre-obesus (25.00-29.99); mild obesity (30.00-34.99); average obesity (35.00-39.99) and morbid obesity (> 40.00) [13].
Nuclear magnetic resonance (NMR) was performed to see: 1) Injury type (extrusion, protrusion or bulge) and 2) Affected discs' position [cervical (C), thoracic (T) or lumbar (L)]. Considering extrusion as the worst lesion and defined as nucleus pulposus has been left out; protrusion in case annulus fibrosus ripped internally but not externally; and bulge when the disc is deformed but not ripped [14].
Treatment consists of a combination of three therapies: Physic therapy, ozone and intravenous injections.
All patients undergo physical therapy as complement to ozone and intravenous injections. It consists of different local interventions to reduce pain, inflammatory and movement limitation. This therapy includes a session per day during 30 days. Physic therapy modalities were: Electrotherapy, local ultrasound, massage, thermotherapy, hydrotherapy, traction bed, Williams exercises and neuromuscular bandage.
Electrotherapy: An inferential current from 80 to 150 Hertz (Hz), was applied in the muscle which surrounds the affected area using bipolar and tetrapolar electrodes by 20 minutes per session.
Local ultrasound: A sonic stimulus of 1 W/cm2 at 1 Mega Hertz (MHz) potency by three minutes per session were applied.
Massage: Therapeutic-relaxing massage was applied approximately five minutes around the injury area.
Thermotherapy: Warm compresses were applied directly in the affected area by 20 minutes.
Hydrotherapy: Consists in performing soft exercises inside the water taking advantage of anti-gravity affects.
Traction bed: Patients were stretched manually during 10 minutes using pelvic and thoracic harnesses.
Williams exercises: They are basic exercises that go from supine to sitting position, considering the stretching of the lumbar muscles and strengthening of abdominal muscles.
Neuromuscular bandage: Also, known as kinesio taping it consists in the application of elastic bands 5 m × 5 cm in size over the affected area.
This therapy includes 30 applications of a mix composed by medicinal ozone and a local anesthetic procaine (0.5 mg at 2% concentration), administered by intramuscular and rectal routes (15 applications for each via). Intramuscular applications were in the pain trigger points, as follow: 1-5 sessions ozone at 15 µg/ml into a 5-ml bolus; 6-10 sessions ozone at 20 µg/ml into a 10-ml bolus and finally, 11-15 sessions ozone 30 µg/ml into a 10-ml bolus. Rectal applications were as follow: 1-5 sessions ozone at 15 µg/ml into a 90-ml bolus; 6-10 sessions ozone at 20 µg/ml into a 120-ml bolus and finally, 11-15 sessions ozone 30 µg/ml into a 150-ml bolus.
Intravenous treatment consists of allopathic, homeopathic and homotoxicology combination drugs. Application periodicity and sessions were personalized depending of symptoms and pain intensity reported by VAS. Allopathic treatment was composed by two mixes. First mix included dexamethasone 4 mg, tramadol hydrochloride 50 mg, metamizole sodium 500 mg and dexketoprofen 50 mg. Second mix included calcium gluconate 2 g, parenteral multivitamin (MVI-12, Grossman, Mexico) 2 ml, magnesium sulphate 2 ml (150 mg/ml). Both mixes were diluted in physiological saline solution 0.9% administrated a 50 ml/hour speed. Application was as follow: 1-5 sessions both mixes, session 6 onwards only the second mix was used. Homeopathic treatment was cocarboxylase 2 ml (carzilasa, Manuell, Mexico). Finally, homotoxicological treatment included a solution of the following drugs: Zeel-T, Discus Intervertebralis, rose-bay (Nerium oleander), Colt Homaccord, Disheel and Cochicom mite.
Statistical differences between sex, age, BMI, injury type and affected disc were analyzed using chi-squared tests (X2). The significance level was set at p < 0.05. H0 was rejected if X2 calculated > X2 of table. Data analysis was performed using Graph Pad Prism 7 software (GraphPad Inc., La Jolla, CA).
A total of 1,000 patients were attended in 9 years and 2 months. Treatment was success (ΔVAS ≥ 4) in 731 and failed (ΔVAS < 4) in 269 patients, being 73.1% and 26.9% respectively (Table 1), which represents approximately a success of ¾ (Figure 1). They were 496 men and 504 women, who treatment success was in 364 and 367 patients respectively. This treatment acts as men as well as women (Table 2). Proportionally there was not different by sex (Figure 2). Their ages were ranging from 11 to 90-years-old. Patients were classified by decades. Decade which has more patients is 61-70 (27.2%), while 11-20 (1.3%), decades has the lowest ones. At each decade were registered patients whose treatment was success. There is not difference in treatment success by age (Table 3), at each decade the proportion of relieved patients was similar (Figure 3). Injuries in young people are principally due to mechanical impact as result of sport practice or automobilist accident, while in old people they are due to a degenerative process own of the age; but interestingly old people recover faster than the youngest. Treatment success also was analyzed by BMI. The majority are ranked in normal, preobese and mild obesity (90.7%). Severity thinness, moderate thinness and mild thinness are the classes with lower reports (9.3%). There is difference in treatment success by BMI (Table 4), since each denomination shows different proportion of relieved patients (Figure 4). BMI is the only parameter which treatment fails when we analyzed each one of the categories; it is obvious because obesity is a risk factor to develop LBP.
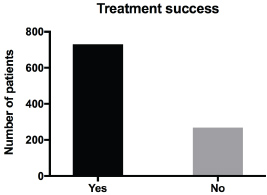 Figure 1: Schematic view of all patients. A total of 1,000 patients were attended. Treatment was success in 731 patients (black bar) and failed in 269 (gray bar) patients.
View Figure 1
Figure 1: Schematic view of all patients. A total of 1,000 patients were attended. Treatment was success in 731 patients (black bar) and failed in 269 (gray bar) patients.
View Figure 1
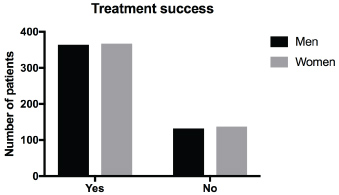 Figure 2: Classification by sex. There were 496 men and 504 women, who showed improvement 365 and 367 respectively, while 132 and 137 did not show improvement.
View Figure 2
Figure 2: Classification by sex. There were 496 men and 504 women, who showed improvement 365 and 367 respectively, while 132 and 137 did not show improvement.
View Figure 2
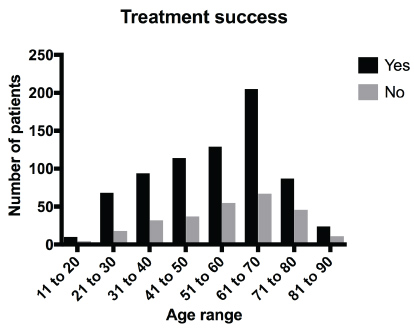 Figure 3: Classification by age. Patients were classified in decades, showing the highest population at the middle of the graphic.
View Figure 3
Figure 3: Classification by age. Patients were classified in decades, showing the highest population at the middle of the graphic.
View Figure 3
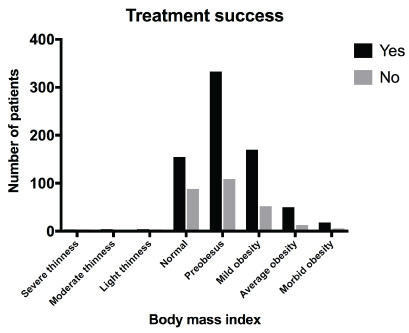 Figure 4: Classification by BMI. Patients were classified in eight groups. Normal, pre-obesus and mild obesity concentrate the highest population.
View Figure 4
Figure 4: Classification by BMI. Patients were classified in eight groups. Normal, pre-obesus and mild obesity concentrate the highest population.
View Figure 4
Table 1: Total patients who participated in the study. Treatment was considered as success if ΔVAS ≥ 4. View Table 1
Table 2: Patients who participated in the study classified by sex. X2 analysis to test H0: There is not statistically significant difference between men and women who received treatment (physical therapy, ozone and intravenous injections) to reduce the low back pain at a significance level of P < 0.05 using 1 as degrees of freedom (v). View Table 2
Table 3: Patients who participated in the study classified by age. X2 analysis to test H0: There is not statistically significant difference between age range of patients who received treatment (physical therapy, ozone and intravenous injections) to reduce the low back pain at a significance level of P < 0.05 using 7 as degrees of freedom (v). View Table 3
Table 4: Patients who participated in the study classified by body mass index (BMI). X2 analysis to test H0: There is not statistically significant difference between BMI of patients who received treatment (physical therapy, ozone and intravenous injections) to reduce the low back pain at a significance level of P < 0.05 using 7 as degrees of freedom (v). View Table 4
Results analysis also was done according: injury type and affected discs' position. We found 1,541 lesions distributed heterogeneously over the 1,000 patients. Thus, each patient has in average 1.5 injury. The most common lesion is the protrusion (50.4%), then bulge (36.4%) and finally the worst injury, the extrusion (13.2%). There is not difference in treatment success when we analyzed lesion type (Table 5), proportion of relieved patients is approximately of ¾ (Figure 5). As expected, lumbar discs have the highest cases (79%), followed by cervical (13.5%) and finally thoracic discs (7.5%) due to protective effect of the ribs. Treatment has the same effect in all the damaged discs (Table 6), since each disc shows similar proportion of relieved patients (Figure 6). Finally, we analyzed the injuries quantity per patient and found 62 patients without defined lesion but they were still presenting pain probably due to an inflammatory process. 490 (49%) patients presented only one injury, while in the most extreme cases there were four patients who had 6 lesions (0.4%). Even so our treatment works as well in 0 injuries as in 6 ones. When we multiply injury quantity per injury numbers and then add together, the result is 1,541 injuries (Table 7). Also relieve proportion in treatment success was of a 75% approximately (Figure 7).
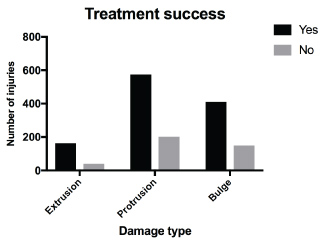 Figure 5: Classification by injuries. Three damages types were studied. Protrusion was the more frequent followed by bulge and extrusion.
View Figure 5
Figure 5: Classification by injuries. Three damages types were studied. Protrusion was the more frequent followed by bulge and extrusion.
View Figure 5
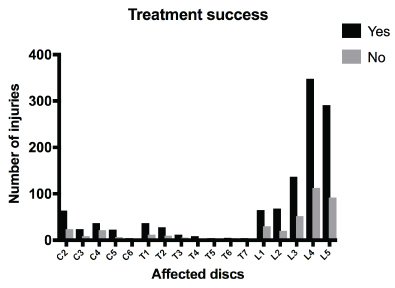 Figure 6: Classification by affected discs. Cervical (C), thoracic (T) and lumbar (L) discs were analyzed. L4 and L5 lesions correspond to 54.8% of cases.
View Figure 6
Figure 6: Classification by affected discs. Cervical (C), thoracic (T) and lumbar (L) discs were analyzed. L4 and L5 lesions correspond to 54.8% of cases.
View Figure 6
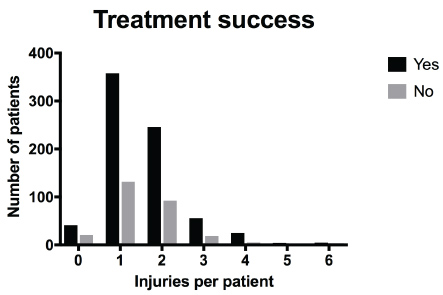 Figure 7: Number of injuries per patient. Most of the patients has one or two injuries, while others have cero and the most extreme 6 lesions. There was treatment success in all cases independently of injuries' number.
View Figure 7
Figure 7: Number of injuries per patient. Most of the patients has one or two injuries, while others have cero and the most extreme 6 lesions. There was treatment success in all cases independently of injuries' number.
View Figure 7
Table 5: Injuries observed in the study. X2 analysis to test H0: There is not statistically significant difference between extrusion, protrusion or bulge in those patients who received treatment (physical therapy, ozone and intravenous injections) to reduce the low back pain at a significance level of P < 0.05 using 2 as degrees of freedom (v). View Table 5
Table 6: Damaged discs observed in the study. X2 analysis to test H0: There is not statistically significant difference between cervical (C), thoracic (T) or lumbar (L) discs in those patients who received treatment (physical therapy, ozone and intravenous injections) to reduce the low back pain at a significance level of P < 0.05 using 16 as degrees of freedom (v). View Table 6
Table 7: Number of injuries per patient. X2 analysis to test H0: There is not statistically significant difference between the number of injuries per patient in those patients who received treatment (physical therapy, ozone and intravenous injections) to reduce the low back pain at a significance level of P < 0.05 using 6 as degrees of freedom (v). View Table 7
The purpose of this report was to teach a treatment to reduce LBP, improve quotidian activities and as possible avoids surgery. This is the first work which reports an effectiveness of 73% using a mixed strategy which combines physiotherapy, allopathic and homeopathic as complementary approaches. Other strengths of this method are excellent recruitment, high treatment compliance, acceptable levels of retention rates, high participant satisfaction, and the most important no associated serious or adverse events.
The total group of patients with LBP (1,000) is heterogeneous and was classified by sex, age and BMI; while injuries (1,541) were classified into damage type (extrusion, protrusion and bulge) in each of one of discs (cervical, thoracic and lumbar), and finally, injuries' number per patient. As said before, treatment's aim is reducing pain and as possible avoid surgery, we did not propose improve any injury; hence in several cases NMR studies showed no injury's improvement after treatment, but these patients reported a pain reduction. However, all participants were attended when they had a new episode of LBP.
The areas of LBP treatment, ranging from conservative methods (oral and intramuscular medication and physical therapy), minimally invasive (percutaneous and disc puncture) to surgery (discectomy, disc arthroplasty, spinal fusion, etc.). In these same order complication rate and possible adverse effect are increasing. By definition, the treatment presented here is conservative. Thus, looking for a treatment of minimal invasion, the best cost/benefit ratio and lowest complication rate; we compare our treatment whit those previously reported on the light their corresponding findings.
There are reports of conservative methods which share some techniques with us. Petit A & Ronzi Y and colleagues reported a protocol based in a set of physiotherapies, which consisted in: 1) Intensive and multidisciplinary program conducted in a rehabilitation center; 2) Less intensive outpatient program conducted by a trained private physiotherapist; and 3) Mixed strategy combining the same outpatient program associated with a weekly multidisciplinary intervention. They did not find significant difference for the evolution of participants' quality of life, social ability, and personal beliefs between the three groups [15,16]. Liu L and coworkers presented a classic no invasive method based on acupuncture. They reported a compliance of 86.7%, unfortunately their study group was done only with 45 participants [17]. There are also reported methods which share radiofrequency and ozone techniques; such as Stagni S and colleagues reported the application of a DiscoGel® chemonucleolysis in patients unresponsive to ozone therapy. This study gave a pain improvement in 24/32 patients [18]. Zhang D and collaborators treated 236 patients by radiofrequency thermocoagulation combined with collagenase chemonucleolysis (it consists of an injection of proteolytic enzymes into the intervertebral disc for dissolving the herniated nucleolus pulposus. The main enzyme used for this purpose was chymopapain, which is a nonspecific proteoglycanase derived from the papaya plant). They found a success of 66.5% (157/236) at 2 weeks' post-operation, and 88.1% (208/236) at 3 months' post-operation. A disadvantage of this method is that it works in post-surgery conditions [19]. Also, there are minimal invasive methods which do not share any techniques, but they have promising results. All of them consist in percutaneous or disc puncture using either radiopaque, methylene blue (MB) and hydrogel. Radiopaque (a viscous solution containing ethyl alcohol and cellulose derivative products associated with tungsten as contrast agent). Radiopaque treatment was a trial only with 80 patients and reported a treatment success of 75%. A success very similar of us [20]. MB injection into the nucleus pulposus to spread into radial fissures where it can destroy the nerve endings or nociceptors that have grown into the painful disc. MB protocol is an ongoing trial which was not completed at the time of submission [21]. Hydrogel is an emerging technique to restore damage disc, by the moment only used in pigs, which requires further work to be evaluated in human [22]. Also, there are the most novel techniques which use umbilical stem cells and platelet-rich plasma. Pang X and colleagues, treated two patients using human umbilical cord tissue-derived mesenchymal stem cells to regenerate degenerative discs. Patients improved immediately their VAS scores during a 2-year follow-up period [23]. In the other hand; Levi D and collaborators reported success rates as follows: 1 month: 3/22 = 14%, 2 months: 7/22 = 32% and 6 months: 9/19 = 47%; a low success compared with our method. They used a single treatment of intradiscal injection of platelet-rich plasma [24]. Finally, we must compare our method with surgery. Surgical treatment provides faster relief, but its benefit is lost in mid-term and long-term. Benefit is no longer than 10 years [25]; while our treatment shows a permanent relief if patients follow our recommendations.
The method proposed here has many advantages. Firstly, it is conventional or non-invasive, uses standard techniques without undesirable effects. As other methods, it uses combination of different fields as complement of each other. It was tested in a large population allowing analyzed its effectivity in the following categories: sex, age, BMI, injuries, affected disc and injuries per patient. This method is effective in all analyzed categories, except BMI due to obesity is a high-risk factor to develop LBP.
We the authors want to express our gratitude to Jorge Octavio Ortiz-Salazar, Oswaldo Beraun-López and Jorge Gaytán-Castillo for their guidance in improving this manuscript.
The authors declare that they have no conflict of interest. This work did not receive public or governmental funding.