Anterior dislocation of the shoulder may go undiagnosed and may thus left untreated for a variable length of time. Chronic locked anterior dislocations of the glenohumeral joint is a rare condition. Its diagnosis and management can be challenging. Reverse shoulder arthroplasty has yelded satisfactory outcomes in patients with cuff tear arthropaty and other degenerative changes of the shoulder joint. The concept of this implant theoretically allows stabilization of the dislocated shoulder independently of soft tissues defects.
The aim of this study was to evaluate the short term clinical outcomes of patients with the diagnosis of chronic anterior locked glenohumeral dislocation surgically treated with a reverse shoulder arthroplasty. 6 patients were included and treated in our institution with a reversed shoulder arthroplasty for chronic anterior glenohumeral dislocations. They were clinically evaluated at latest follow-up with the Constant-Murley Score. All patients had pre-operative shoulder trauma series X-rays and CT-scan.
The average age was 69.5 years and time from dislocation to surgical treatment was 7 weeks. The average time of the latest follow-up and clinical evaluation was 8 months. One of the patient had severe anterior glenoid bone loss and was treated with humeral head autograft. Median Constant-Murley (CM) score at the latest follow-up was 65. Postoperative radiographs at latest follow-up showed no sign of scapular notching, humeral or glenoid loosening or heterotopic ossification. No other complications that required surgical or medical treatment were registered.
Some few recent studies have shown promising results for patients who undergo reverse shoulder arthroplasty for chronic anterior dislocation. Besides that, few are the follow-up studies described. With this clinical cases series, it can be concluded that, facing with a rare condition as a chronic anterior locked glenohumeral dislocation, a reversed shoulder replacement can be a reliable method of treatment and good and predictable functional results can be expected.
Under certain circumstances, anterior dislocation of the shoulder may go undiagnosed and may thus left untreated for a variable length of time [1]. A chronic dislocation of the shoulder is defined when the diagnosis is delayed by more than 3 weeks [2,3]. Chronic locked anterior dislocations of the glenohumeral joint is a rare condition and is usually related to trauma of the affected shoulder [4,5]. The common mechanism is an abduction and external rotation force applied to the shoulder [6]. Its diagnosis and management is challenging since these dislocations usually occur in debilitated and elderly patients [7]. Concomitant pathologies such as bone defects on the humeral and/or glenoid side are very frequent, besides the poor bone quality and a decreased rehabilitation potential [7-11]. Over time, anterior soft tissues structures are stretched, and the posterior capsule and cuff may develop contractures; additionally, the cartilage damage also occurs [12].
When severe bone loss and/or advanced arthritis occurs, shoulder arthroplasty can be necessary [13,14]. Reverse shoulder arthroplasty has yielded satisfactory outcomes in patients with cuff tear arthropathy and other degenerative changes of the shoulder joint [15,16]. The concept of this implant theoretically allows stabilization of the dislocated shoulder independently of soft tissues defects [17].
The aim of this study is to evaluate the short term clinical outcomes of patients with the diagnosis of chronic anterior locked glenohumeral dislocation surgically treated with a reverse shoulder arthroplasty.
All patients between January 2017 and December 2017 that were treated in our institution with a reversed shoulder arthroplasty for chronic anterior glenohumeral dislocations were retrospectively evaluated. They were clinically evaluated at latest follow-up with the Constant-Murley Score. Range of motion was recorded using a goniometer for elevation and external rotation and the most cephalad spinal level reached by the thumb for internal rotation. All patients had pre-operative shoulder trauma series X-rays and CT-scan, post-operatively were evaluated with X-ray.
All patients were installed in the beach-chair position under general anesthesia. The deltopectoral approach was utilized for all the surgeries performed. The rotator cuff interval was opened and a tenodesis of the long head of the bíceps was performed at the pectoralis major tendon. A tenotomy of the subscapularis at the tendino-osseus transition was established and the arm progressively brought in external rotation. Once the humeral head was freed, the endomedullary canal was reamed starting from the top. Osteotomy of the humeral head was performed in 20 degrees of retroversion. Exposure of the posterior capsule was performed and it was completely released. The glenoid was exposed and then reamed until a "subchondral smile" of cancellous bone was reached. A bone graft harvested from the resected humeral head was performed. If an anterior glenoid defect was present. Once the glenoid plane was smoothly reamed, the central hole of the baseplate is drilled guided by the K-wire, and metal-back is introduced and tapered into the glenoid. The fixation was optimized with one superior and one inferior screws. The glenosphere was assembled (36 mm) to the baseplate and secured with a screw. Reaming of the humeral side was performed and the thickness of the polyethylene determined after a trial reduction. The definitive humeral components were introduced, reduction performed, and the subscapularis reinserted. Finally, a suction drain introduced and the wound was closed.
6 patients (5 females and 1 male) were diagnosed in our hospital's emergency department with chronic shoulder dislocation. The average age was 69.5 years (range between 64 and 80). The average time from dislocation to surgical treatment was 7 weeks (between 5 and 10) and the time between diagnosis and treatment was in average 2 weeks. The average time of the latest follow-up and clinical evaluation was 8 months (between 6 and 16 months). One of the patient had severe anterior glenoid bone loss and was treated with humeral head autograft. Median Constant-Murley (CM) score at the latest follow-up was 65 (between 35 and 80). The patient with 35 was 80-years-old and suffers from Parkinson and Scleroderma, which limited rehabilitation and consequently the score. Excluding this patient, the median CM score was 71 (between 61 and 80). Mean shoulder flexion was 105° (range 55° - 170°), external rotation 18° (range -0.5° - 26°); internal rotation median was waist (L3) (buttock - T12 vertebra). The previous mentioned patient also had the most limited ROM. Postoperative radiographs at latest follow-up showed no sign of scapular notching, humeral or glenoid loosening or heterotopic ossification. No other complications that required surgical or medical treatment were registered (See Figure 1 and Figure 2).
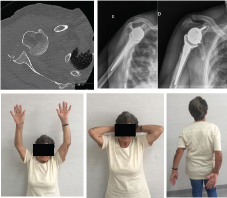 Figure 1: Pre-op axial CT-scan axial view; Post-op X-Ray; Latest follow-up mobilities. View Figure 1
Figure 1: Pre-op axial CT-scan axial view; Post-op X-Ray; Latest follow-up mobilities. View Figure 1
 Figure 2: Pre-op X-ray AP views; Latest follow-up mobilities. View Figure 2
Figure 2: Pre-op X-ray AP views; Latest follow-up mobilities. View Figure 2
Reverse shoulder arthroplasty used to be reserved for older, low-demand patients in whom rotator cuff arthropathy was diagnosed, sequelae of previously treated proximal humerus fractures, and others. However, research has led to an improved understanding of the biomechanics behind reverse shoulder prostheses, which has improved implant design and surgical techniques. Consequently, orthopaedic surgeons have slowly begun to expand the indications for reverse shoulder arthroplasty to include a wider spectrum of shoulder pathologies and some few recent studies have shown promising results for patients who undergo reverse shoulder arthroplasty for chronic anterior dislocation [18]. Besides that, few are the follow-up studies described.
Verhaegen, et al. in a small case series of three patients diagnosed with a chronic unreduced anterior dislocations of the shoulder, one of them was surgically treated with a reverse shoulder replacement achieving a good function without pain but with weakness in rotational movements [1].
Hyun, et al. in 5 patients with chronic locked anterior dislocation treated with a reverse TSA, although they were not formally studied, their motion and pain have shown improvement and all but 1 were satisfied with the result [19].
Van Togel, et al. in a more recent retrospective study of 6 patients with anterior glenohumeral dislocation that were treated with a reversed shoulder arthroplasty, evaluated the postoperative Constant-Murley (CM) score. Average age was 73 years, average time of dislocation was 18 weeks and average time of follow-up was 39 months. CM improved from 33 pre-operatively to 76 postop (between 55 and 89). No postoperative complications were observed. The authors concluded that Reversed shoulder arthroplasty gives good results in cases of chronic glenohumeral dislocation and realized that Predictable results can be obtained similar to the literature of the reverse prosthesis in trauma of the proximal humerus [20].
In our series, besides the smallest average time of follow-up and younger average ages, Constant-Murley score at the latest follow-up was a little bellow comparing with Van Togel, et al. case series. Still, if excluded the patient with Scleroderma and Parkinson diseases, the CM score approaches the results of the Van Togel, et al. study. This is a short follow-up clinical case series, and with time we should expect a higher CM average score, taking into account the short period of rehabilitation and proprioceptive training.
With this clinical cases series, it can be concluded that, facing with a rare condition as a chronic anterior locked glenohumeral dislocation, a reversed shoulder replacement can be a reliable method of treatment and good and predictable functional results can be expected.