CLBP is the leading cause of years lived with disability worldwide and patients with yellow flags have the worst outcomes and contribute significantly to the societal cost. Clinicians are aware of the importance of yellow flags but feel undertrained to deal with them. Furthermore there is a lack of clarity for clinicians looking at how to specifically manage these patients from guidelines and an incredibly varied set of approaches available to clinicians. The objective of this review was to review the effectiveness of the physiotherapy interventions for chronic low back pain patients with yellow flags that have been studied. Three approaches were used for retrieving literature. Searches were conducted initially using the terms "physiotherapy", "chronic low back pain", psychosocial and "management or treatment", using the databases PubMed, Embase, PEDro and CINHAL from January 1987 up to February 2017. In addition content experts were consulted to ensure no additional papers were missed and citation tracking was implemented. 39 studies were identified with 20 meeting the selection criteria. Interestingly the term yellow flags is not used in the treatment literature and instead specific psychosocial terms are used. This review tentatively suggests specific exercise and passive interventions are more beneficial for reducing measures of pain, whilst psychological input and general exercise appears more targeted towards psychosocial measures.
Low back pain (LBP) is usually defined as pain localised below the costal margin (ribs) and above the inferior gluteal folds (buttock crease). It is the leading cause of years lived with disability worldwide and is becoming increasingly prevalent [1-5]. Chronic low back pain (CLBP) is variously defined as lasting longer than 7-12 weeks, to 3 months [6,7]. LBP is typically classified as "specific" or "non-specific". Specific LBP refers to symptoms caused by specific pathophysiologic causes, such as hernia nucleus, infection, inflammatory disease, osteoporosis, rheumatoid arthritis, fracture or tumour [8]. There is no effective cure for non-specific low back pain (NSCLBP) and this represents the 90% of the LBP population that cannot be classified as specific LBP [9]. Most guidelines are based on the assumption that symptoms resolve spontaneously and that return to work equals recovery [6,10]. However, when pain is assessed it appears patients may be returning to work despite their pain [11], and whilst spontaneous recovery occurs in approximately a third of patients after 3 months, 71% still have pain after 1 year [12].
CLBP patients with psychosocial, psychological and social, risk factors are known to have poorer outcomes and increased management costs [13,14]. The term "yellow flags" was originally used to describe psychosocial risk factors that predict disability in LBP patients [15]. These risk factors are predictors of return to work and disability in CLBP patients [16]. The risk factors can be identified using a questionnaire or a clinical diagnosis [17]. Questions cover beliefs that are associated with delayed return to work and disability. These include fears about pain, injury, recovery and being despondent or anxious. It is suggested that having a few strongly held negative beliefs or several weaker ones could be used to identify at risk patients [14]. These beliefs increase a patient's perception of threat and modern neuroscience suggests that pain is the conscious interpretation that tissue is in danger [18]. These beliefs can be viewed as "thought viruses" [19].
Yellow flags are now included in most LBP guidelines although there is wide variation in suggestions in how to manage these patients [8]. All guidelines consider the assessment of yellow flags but treatment is not specifically addressed. All guidelines at least briefly state the need for re-assurance and return to normal activities, which may aid yellow flag management. The European guidelines suggest the inclusion of a cognitive behavioural approach and the German guidelines propose psychotherapy may be an education option and suggest referral for multi-disciplinary treatment. Thus within the guidelines the importance of yellow flags is appreciated in assessment and for triage but there is ambiguity in the specifics of management.
The differences seen across the full range of physiotherapy approaches is far greater than within the guidelines. The Maitland and McKenzie approaches are the most utilised in the UK [20]. These approaches and the traditional orthopaedic medicine approach [21] are perhaps the most bio-medical focused, placing emphasis on finding and treating the tissues that is the cause. Other approaches such as that derived by O'Sullivan [22] and, Lee and Vleeming [23] attempt to classify patients that need more psychosocial input. With the new clinical model 4, the Society of Musculoskeletal Medicine is moving in the same direction [24]. The Neuro Orthopaedic Institute and Mind in Body groups place the most emphasis on a hands-off approach to psychosocial aspects [19]. This approach is based on an understanding of the importance a patient's perception has on their symptoms and thus the benefits of education and a graded return to normal activities. In contrast Dorko [25] is a proponent of a hands-on approach to addressing the psychosocial aspects. Clinicians are aware of the importance of psychosocial factors in these patients [26] but feel underprepared and may sometimes stigmatise these patients [27]. Furthermore as Stewart, et al. [28] states that yellow flag identification questionnaires are not contextually situated, have poor content validity and clinical specificity. In particular they highlight concerns over the constraining nature of the STarT tool with regard to question 7 [29], "worrying thoughts have been going through my head in the last 2 weeks", agree or disagree. Similar, concerns are valid for the Örebro tool over anxiety [30]. Thus whilst yellow flags are clearly important there remains a lack of clarity for clinicians looking at how to specifically manage these patients from guidelines and clinicians are using an incredibly varied set of approaches. This systematic reviews aims to investigate the physiotherapy management of CLBP patients with psychosocial symptoms.
Three approaches were used for retrieving literature. Searches were conducted initially using the terms "physiotherapy", "chronic low back pain", "yellow flags" and "management or treatment", using the databases PubMed, Embase, PEDro and CINHAL from January 1987 up to February 2017. Due to the paucity of papers returned the term "yellow flag" was replaced with "psychosocial". In addition content experts were consulted to ensure no additional papers were missed and citation tracking was implemented. Foreign language papers that were identified using the English terms were included. Refworks was used to store and remove duplicates from the searches.
The researcher initially screened the title and abstract of the identified studies. The full text was then analysed. Studies were selected on the basis of the following selection criteria;
1. Primary experimental design study of human participants with chronic (> 12 weeks) or recurrent (repeated episodes over 12 months) low back pain.
2. Participants must have yellow flags or measured psychosocial status commensurate with yellow flags.
3. Studies must cover the management of patients.
Studies were excluded if;
1. The intervention group did not have yellow flags or measurable psychosocial factors.
2. Looked at post surgical patients.
3. Mixed groups of sub-acute and chronic patients.
4. Mixed groups of neck and CLBP patients.
5. The intervention was purely psychological (CBT) and outside the scope of traditional physiotherapy practice.
Risk of bias was assessed as suggested by the Cochrane Back Review Group [31]. Studies with a score above 6 were considered low risk of bias. Studies with a score below 6 were considered high risk. Where any doubt remained an author of the study was contacted via email.
In total 39 studies were identified, after screening titles and abstracts 27 remained. Three papers were excluded on reading the full text as there were no measures of psychosocial factors (three studies), one as the intervention was chiropractic and outside traditional physiotherapy practice, another paper [32] was excluded as it included both neck and back patients in one homogenous group with no separate analysis of back pain patients, and another had a definition which allowed for sub acute low back pain patients to be included [33]. The remaining 20 papers met the inclusion criteria. One foreign language paper met the inclusion and included [34], this paper was translated using google translate so that it could be included in the analysis. A clear limitation is that these studies look at groups of CLBP patients that show yellow flags on average, but within each cohort there will have likely been patients with very few yellow flags and possibly some with very significant yellow flags. Using the guidelines of the Cochrane Back Review Group [31] the studies were classified as high or low risk.
Three papers were high risk [34-36] and 17 were classified as low risk. The oldest trial that met the selection criteria was Alaranta, et al. [37] as despite it's age it met all quality criteria for selection. The 20 studies all looked at patients of 18 years or older with CLBP, using at least 6 months follow up. All but four were randomised controlled trials, with four being cohort studies [34-36,38,39] and another with no randomisation [40] (Figure 1).
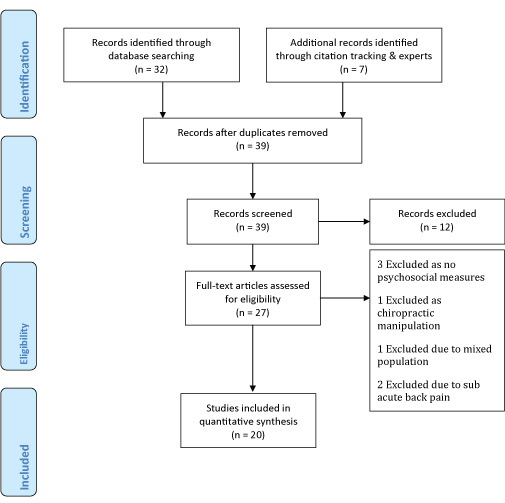 Figure 1: PRISMA flow diagram. View Figure 1
Figure 1: PRISMA flow diagram. View Figure 1
The studies identified cover a broad spectrum of biopsychosocial interventions, with some focusing on more biomedical interventions, psychosocial interventions or a combination. Six studies looked at a predominantly biomedical approach.
Two studies with a low risk of bias from the same group have examined a passive biomedical intervention. Weiner, et al. [41,42] conducted randomised controlled trials of percutaneous electrical nerve stimulation (PENS). This involves delivering a low voltage electrical current through a specially designed needle to the adipose layer close to the nerves near the site of pain. Patients were aged 65 or older, experienced moderate CLBP. In their earlier study [41] the Geriatric Depression Scale mean score was 6.81, which equates to mild depression. In their later study [42] psychosocial function measures showed mild to moderate levels of psychosocial stress across the Geriatric Depression Scale, the Chronic Pain Self-Efficacy Scale, the Catastrophizing Scale of the Cognitive Strategies Questionnaire and the Fear-Avoidance Beliefs Questionnaire. The combination of the scores across these measures shows these patients had yellow flags in both studies.
In their earlier study subjects were randomised to receive 6-weeks of twice weekly PENS and physical therapy or sham PENS stimulation and physical therapy. The PENS and physical therapy group had significant reductions in pain intensity and pain related disability, the control group did not. These improvements remained at 3-month follow up. Furthermore, significant improvements in physical and psychosocial function were also seen in the PENS and physical therapy group. In their later study [42] they had 200 participants, randomised to receive either PENS, brief PENS to control for treatment expectancy, PENS with general conditioning or brief PENS and general conditioning. All interventions were done twice a week for 6 weeks. After the 6-week intervention all four groups produced statistically significant improvements in present, average and greatest pain intensity measured on the short form McGill Pain Questionnaire. Interestingly the brief PENS of 5-minutes produced an equal improvement to that of the 30-minute PENS. Furthermore, the general conditioning protocol had no additional benefit on pain measures above that of the PENS interventions, however it did significantly improve fear avoidance in comparison to PENS. These studies suggest that whilst sham PENS is ineffective, 5-minutes is sufficient to have treatment effect, casting significant doubt over the authors proposed mechanism of effect and suggesting the effects may be more centrally driven. Furthermore they indicate the potential benefits of active interventions, in particular general conditioning, on fear avoidance beliefs.
Geisser, et al. [43] conducted a randomised controlled trial of specific exercise and manual therapy for CLBP. Patients received either specific exercises tailored for their back pain by a physiotherapist or a non-specific programme of general stretching and aerobic exercise. In addition patients received either manual therapy or sham manual therapy. Patients were seen once per week for 6-weeks and asked to do their exercises twice daily. Only 72 out of 100 patients completed the study. They found that specific exercise and manual therapy significantly reduced pain but not disability. It is interesting to hypothesise that addressing pain may not address the psychosocial symptoms. Indeed those prescribed general exercise showed a trend towards reduced disability.
Five of the studies examined exercise-based interventions. Murtezani, et al. [44] found high intensity aerobic exercise outperformed a passive electrotherapy group not dissimilar to the approach of Weiner and colleagues. They randomised 101 patients to either a high intensity aerobic exercise group or a passive modalities group. The active group produced a 3.9 decrease in visual analogue scores and significant improvements in pain intensity, toe touch and psychosocial measures in contrast to the electrotherapy. This passive intervention was far less effective than the results seen in Weiner and colleague's studies [41,42].
In contrast the other two low risk of bias studies looking at low intensity aerobic interventions found no significant difference between their intervention and control groups. Hurley, et al. [45] conducted a 3-arm assessor blind RCT of an individualised walking programme, an exercise group intervention and usual care physiotherapy, in 246 patients aged 18-62 with CLBP. Patients also received education on functional restoration and addressing fears around movement and the patient's understanding of their problem. The walking programme was in line with the recommendations of the American College of Sports Medicine and previous studies [46-48]. The exercise group attended a class based on the back to fitness programme [49] endorsed by the UK National Institute of Clinical Excellence guidelines. The physiotherapists providing the usual physiotherapy were free to prescribe education, advice, manipulation and exercise as usual but could not refer patients to an exercise group or a walking programme. Similarly, Mannion, et al. [50] compared modern active physiotherapy, muscle reconditioning on training devices, and low-impact aerobics, each done twice a week over 3-months. As is quite typical in many studies the specifics of what was actually done in terms of exercises and all acute variables remains a mystery. Muscle reconditioning involved 12-weeks on the David Back Clinic programme. 148 participants met the inclusion criteria and 16, 10.8%, dropped out during the study. The three groups did not differ significantly in terms of compliance with 84.1% completing all 24 sessions. Interestingly in both studies all interventions were equally efficacious, despite all three interventions targeting different aspects of physical conditioning.
Mannion, et al. [50] suggest this shows that the mechanism of benefit may be more central and possibly due to challenging beliefs around physical activity and chronic low back pain. This is further supported by the correlation between improvement in fear avoidance beliefs and self rated disability. Furthermore these correlations were also present in the devices and aerobics group where these effects were still seen at 6-months, but not in the active physiotherapy group where they were not seen. There were also improvements in spinal flexion and these improvements were correlated with improvements in pain and intensity and self-rated disability. Hurley, et al. [45] highlight that whilst there was no difference in outcomes, the walking programme had the greatest adherence and the lowest costs.
Two studies with low risk of bias looked at lumbar extensor training. Risch, et al. [51] investigated the effects of 10-weeks of lumbar extension exercise on 52 patients with CLBP. Initially 31 received treatment and 21 were placed on a waiting list. Pain and isometric strength significantly increased in the treatment group. Furthermore psychosocial and physical dysfunction also significantly decreased. Building on this Vincent, et al. [52] compared total body resistance training with lumbar extensor training and a control group in obese individuals. Resistance training sessions were carried out three times a week for 4-months. The lumbar extension group did just the lumbar extension exercise from the total body resistance-training group. As is typical in these studies no information on the tempo of the exercises was provided. The control group received advice on healthy nutrition via a leaflet from the American Heart Association, information about back pain and information on bodyweight back strengthening exercises. The total body training group had greater reductions in self-reported disability as measured on the Oswestry Disability Index and Roland Morris Disability Questionnaire. Pain Catastrophizing Scale scores decreased in the total body training group more than in the control group at 4-months. Lumbar extensor training and total body training both decreased walking and chair rise pain severity significantly more than the control. From this it is tempting to imply that the lumbar extensor training was sufficient to improve physical function whilst the total body training provided additional benefits to perceived disability and psychosocial factors.
Eight studies looked at more directly addressing the psychosocial component of patient's pain experiences, two of which looked specifically at the effects of pain education and were considered low risk of bias. Moseley and colleagues [53] conducted a randomised controlled trial comparing pain neurophysiology education with traditional back school education. 15-week days after the initial assessment participants receiving pain neurophysiology education had significant improvements in pain attitudes, pain catastrophizing scale, straight leg raise and forward bend compared with the back education group. Roland Morris Disability Questionnaire was statistically significantly improved although the authors suggest this probably was not a clinically significant improvement.
Vowles, et al. [40] looked at the effect of pain acceptance, pain control and continued practice instruction strategies on physical impairment index scores, in 74 unemployed individuals on workers compensation with LBP for greater than 3 months. The instructions for the first test were the same for all participants. For the second test participants were randomised in to three different groups, focusing pain control, pain acceptance or suggesting continued practice would improve performance. After the intervention the pain acceptance group reduced their scores by 16.3%, whilst there was a worsening of 8.3% in the pain control group and 2.5% reduction in the continued practice group. Interestingly there was no significant difference across groups in terms of pain during the tasks. This suggests that the pain acceptance strategy allowed the patients to improve their physical performance without any increase in pain. Conversely it suggests the pain control group had increased physical impairment with no improvement in pain. The authors note that 124 people in total were asked to start the trial and only 91 started. They state that authors experience suggested that the patients that refused to take part were afraid of exacerbating their symptoms. This skews the population of the study towards those who were more likely to do well with this intervention. Nonetheless it provides what appears to be an immediately useful approach for clinicians to use in explaining how to approach pain during exercise and activities of daily living. The combination of pain acceptance with pain neurophysiology education may prove even more advantageous but this remains to be seen.
Six studies looked at what could be considered intensive rehabilitation programmes, with functional restoration and cognitive behavioural therapy (CBT) components. Three of these studies had a high risk of bias [34-36].
Borys, et al. [36] examined the effectiveness of a three-week intensive inpatient multimodal programme on chronic low back pain patients in 155 patients. 66 patients went on a waiting list to start and then received the programme after the original 89 had received treatment. Pain intensity, well-being, anxiety and depression were all significantly improved compared to the waiting list control. Multimodal therapy was an individually tailored programme decided on by a multidisciplinary team involving physicians, physiotherapists, a clinical psychologist and a pain nurse. Treatment was for 8-hours a day 6 days a week and included medication modification, once a week one on one CBT, daily group CBT, work hardening, Nordic walking, pain and psychological education, and tailored exercise. The greater the number of treatments tried before the study the worse the patients responded to treatment.
Pfingsten and Hilderbrandt [34] reported on the results of the functional restoration programme which they trialled over 10 years with 762 CLBP patients, from 1990 to 2000. This was the lowest quality study of those identified, with no randomisation, blinding and no explanation of drop outs. Nonetheless, it had an excellent follow up length and a large number of participants in comparison to other studies. As expected patients who were off work had increased psychosocial and pain symptoms compared with working patients. Their programme consisted of a 3 week pre-programme of education, stretching and bodyweight exercises followed by an intensive 7 hours a day outpatient programme for 5 weeks. This involved aerobic, functional strength and endurance exercises, back school education, cognitive behavioural group therapy, relaxation training and vocational counselling. The programme reduced Numerical Rating Scale, Pain Disability Index, Allgemiene Depressionsskala (amount of depression), psychological distress (Fear Avoidance Beliefs Questionnaire) and healthcare utilisation. Furthermore work capability significantly improved. However, when they modified it to remove the work hardening component there were no such improvements. These results remained stable at 12-month follow up.
Kainz, et al. [35] compared the effectiveness of Enhanced Outpatient Therapy, Outpatient Rehabilitation Therapy and Medical Training Therapy across 1274 chronic low back pain patients. There was no difference between treatments in terms of effectiveness or satisfaction. As Medical Training Therapy can be done whilst working and costs the least it was the most cost effective of approach for this patient group.
Three studies with a low risk of bias using intensive psychosocial based physiotherapy interventions were identified [37,39,54]. Alaranta, et al. [37] looked at a combined psychosocial activation and physical intervention in CLBP compared with an inpatient rehabilitation programme in 152 patients, with a control group of 141. All patients had been referred to receive inpatient rehabilitation in Finland. Subjects were stratified according to sex and age and randomised to either group. Both interventions started 3-weeks after assessment and lasted 3-weeks. The intervention group received 37-hours of guided self-controlled physical exercises, without passive physical therapy and 5 hours of discussion groups a week, and individual consultations for work problems. The programme included a range of cardiovascular activities and games, strength and endurance training based off the patients 1 repetition maximum, stretching, relaxation and cognitive-behavioural disability management groups. This group did not receive any passive physiotherapy. The inpatient therapy involved a large amount of passive therapy as well as back education, pool exercises, indoor and outdoor activities. The authors considered this programme to be 40-50% of the intensity of the intervention group. The other study [54] directly assessed psychosocial treatment in CLBP patients aged 18-55, with Orebro Musculoskeletal Pain Questionnaire scores of 106-145 indicating moderate psychosocial risk factors. Patients were randomised to either an integrated work rehabilitation group or the conventional treatment group. Physiotherapists in this study had postgraduate qualifications and had received training in the cognitive behavioural approach. Patients received individual treatment for up to 3 months. Conventional treatment typically involved a combination of electrophysical agents, lumbar traction, manual therapy, and exercise therapy. Dictated by the patients' symptoms at presentation and on their response to treatment. The cognitive behavioural approach group received an individualised graded activity programme, pacing techniques, work conditioning, return-to-work goal setting, self-management strategies, job analysis, and ergonomic advice. The aim was to improve their physical and functional capabilities with thorough attention to return to work. The researchers took the step of calling patients who missed an appointment to remind of them of their next appointment. Patients were discharged when they were able to return to work, had a subjective improvement of 70% or greater or they reached a plateau.
In both studies the authors suggest the results for the primary intervention group are clinically significant. Alaranta, et al. [37] found that at 3-months lateral trunk flexion, trunk rotation and hamstring flexibility was 11-12% increased in the combined group compared with 2-9% in the inpatient group. Abdominal, back and squatting strength improved significantly more in the intervention group in comparison to the inpatient group. These trends remained at 1-year follow up. The intervention group had greater decreases in pain at 3-month (17.1 vs. 9.1) and 12-month (15.9 vs. 8.9) follow up as measured using the Million index. Usage of physiotherapy and medical services was significantly decreased in both groups with the intervention group performing best. Mean days of sick leave per year decreased by 14 days in the intervention group, although this was not statistically superior to the inpatient group. At baseline to 3-months and at 12-month follow-up there were significant improvements in depression, subjective symptoms, and aspects of personality, beliefs in disease and control and psychosocial adjustment in both groups. Similarly, Lee, et al. [54] found that at discharge, the patients in the cognitive behavioural approach group made significant improvements in work recovery expectation, pain self-efficacy, and were more satisfied than the conventional treatment group.
Similarly, Tutzschke, et al. [39] investigated the effects of the German new back school. After the initial 3-month programme there were no statistically significant improvements across pain, disability or multifidus tests. However at 12-month follow up they found significant improvements across all measures. Interestingly, CLBP patients had decreased multifidus surface EMG compared to healthy controls, this did not initially change after the 3-month programme. However, after 12-months significant improvement in multifidus firing had occurred.
Four trials with low risk of bias using a classification-based approach were identified. Two approaches used the Cognitive Functional Therapy (CFT) approach developed by O'Sullivan [55], whilst the others looked at classifying patients for motor control [56] and Sahrmann's movement impairment syndromes [57].
Macedo, et al. [56] examined whether patients could be sub-classified to identify those more suitable for motor control exercises. They analysed the results of an earlier trial of 172 patients with CLBP. Patients received 12 treatment sessions over 8 weeks, with follow up sessions at 4 and 10 months. Psychosocial, features, physical activity, walking tolerance and self reported signs of clinical instability were measured at baseline, additionally, pain and function were measured by a blinded assessor at baseline, 2,6 and 12 months. Self reported clinical instability was a significant predictor of treatment effect at 12 months. Those with scores above 9 did 0.76 points better with motor control, whereas those with scores below 9 did 1.93 points better with graded activity. The researchers concluded by suggesting that the 15-point questionnaire can identify patients who will respond better to motor control or graded exposure exercises.
Henry, et al. [57] assessed the effects of providing matched treatments based on patient's clinical features improved outcomes compared to providing unmatched treatments. The matched treatments were based on Sahrmann's [58] movement impairment syndrome. 124 subjects with chronic recurrent back pain of greater than one-year duration were initially classified as suitable for stabilisation training or not and then sub-classified in to one of five movement impairment categories. Patients were randomised on a 3:1 ratio to either receive treatment as suggested by their classification, matched 76, or stabilisation exercises, unmatched 25. 23 were deemed unsuitable for stabilisation exercise. They then had a one-hour treatment session per week for six weeks. Both groups improved significantly in all measures, with the only difference between matched and unmatched treatment being disability as measured on the graded chronic pain scale.
The multidimensional pain inventory classifies patients as either adaptive copers, inter-personally stressed or dysfunctional. Dysfunctional profile patients have previously shown most improvement with multidisciplinary treatment, which has been attributed to the psychosocial input in such programmes. Riipinen, et al. [59] looked to assess how patients in this group would do without specific psychosocial input. They randomised CLBP patients to receive manipulation, exercise and physician consultation or physician consultation alone, with 102 patients in each group. Although all patients improved, the dysfunction profile patients in the combined group improved most. This has implications both for treating these patients and future research. This suggests this group of patients are especially sensitive to treatment as their decreased acceptance of pain and increased pain related anxiety exaggerates symptoms and but also increases their response to treatment.
O'Sullivan, et al. [38] recruited 47 patients with at least a 1-year history of NSCLBP to a waiting list. 26 met all the selection criteria and underwent an initial 3-months on waiting list where they repeated the baseline assessments at 6-weekly intervals. The study did not have a control group, but went to extensive lengths to establish that participants had a stable condition and establish a clear baseline for the group. Based on the STarT Back screening tool scores, 14 patients were high risk, eight were moderate, and four were considered low risk. These scores indicate that these patients had yellow flags. They were then put through a cognitive functional therapy programme, which, focused on improving functional movements and postures, and tackling pain behaviours. In addition they took patients through cognitive reconceptualisation of their NSCLBP experience. Questioning of beliefs around pain, their relationship to pain, pain coping, and the relationship of stress with their pain were assessed. The primary outcomes were the Oswestry Disability Index and the Brief Pain Inventory, the average of four pain scores, maximum, minimum, average and current pain in the last 24 hours. An average of 7.7 treatments was conducted over 12 weeks. Oswestry Disability Index scores were 22 points lower after treatment, 23 points lower after 3 and 6 months and 24 points lower after 12 months. The initial reduction equates to a 54% reduction from baseline. Pain scores were 1.6 points lower after treatment, 1.5 and 1.6 points lower after 3 and 6 months and 1.7 points lower 12 months. All these results represented statistically significant reductions.
Vibe Fersum, et al. [60] unusually specified that participant's pain was provoked and relieved by specific activities, movements or postures. The numerical rating scale needed to average at least 2/10 over the proceeding 14 days and the Oswestry Disability Index needed to be greater than 14%. The authors state the selection criteria designed this way to select patients whose movement behaviour had a clear association with their pain disorder. Patients with greater than 4 months sick leave were excluded on the grounds that they would require a specific return to work programme. 121 participants met the inclusion criteria and were randomised to receive either a cognitive behavioural functional therapy or manual therapy and exercise. The three physiotherapists delivering the approach were experienced exponents of using a multidimensional classification system. Based on the classification system each patient received a tailored intervention targeted at improving the cognitive, movement or lifestyle component the classification system suggested was maladaptive or provocative. The Orebro Musculoskeletal Pain Questionnaire was also used to target psychosocial interventions. The intervention had four main components. For each patient their vicious cycle of pain was explained in a personalised diagram based on their assessment findings. Specific movement exercises designed to normalise their maladaptive movement behaviours were given based on their movement classification diagnosis. Functional restoration based on the movements they reported avoiding or provocative, and a physical activity programme tailored to the movement classification. The initial session was 1-hour and follow-ups were 30-45 minutes. Patients were initially seen once a week for 2-3 weeks and then progressed to follow-ups every 2-3 weeks over the course of the 12-week intervention. The comparison group received joint mobilisation or manipulation techniques to the spine or pelvis as delivered by specialists in orthopaedic manual therapy with an average of 25.7 years experience. These physiotherapists had no prior experience of the classification system or cognitive behavioural functional therapy. 82.5% of the patients received exercises based on the physiotherapists' findings. Initial appointments in this group were 1 hour and follow-ups lasted 30 minutes. Both sets of therapists underwent a half-day of training with a clinical psychologist on the concepts of a best practice cognitive approach to managing back pain. Both groups received 8 sessions on average. Their primary outcome measures were pain was measured using the pain intensity rating scale and the Oswestry Disability Index. A validated 15-item scale to self-evaluate back specific function. There is some confusion over the pain scale used as the test suggests it was average pain over the proceeding two weeks, whilst the table reporting the data suggests it was one week. There was no difference in medication usage between groups before or after treatment. A lack of compliance withdrawal was set at 50%, leading to 27.1% of the manual therapy and exercise group, and 17.7% from the cognitive functional therapy group failing to complete treatment, which precluded an intention to treat analysis. After the intervention average pain over the last week decreased from 5.3 to 3.8 and stayed 3.8 at 12-month follow up, in the manual therapy group. In cognitive functional therapy group it went from 4.9 to 1.7, and crept back to 2.3 at 12-month follow up. The Oswestry Disability Index decreased from 24.0 to 18.5 after intervention and was 19.7 at 12-month follow up in the manual therapy and exercise group. In the cognitive functional therapy group it decreased from 21.3 to 7.6 and was 9.9 at 12-month follow up. These results were all statistically significant in favour of cognitive functional therapy over manual therapy and exercise. It is clear which intervention they were hoping to prove effective and it is possible that increased effort consciously or unconsciously may have gone in to the treatment group. Further the clinicians treating the control may well have been less invested in the outcome of the subjects they treated. This may account for the treatment group receiving 30-45 minutes for follow-ups compared to 30 minutes in the control group. Nonetheless the results are in keeping with those of O'Sullivan, et al. [38] highlighting the benefit of a classification-based approach.
Given the significant nature of the problem of chronic low back pain it is surprising only 20 studies met the inclusion criteria. These studies show a consistent pattern that a variety of interventions are able to decrease psychosocial symptoms, improve function and decrease perceived pain. Disappointingly none of the research on the popular Maitland and McKenzie approaches met the inclusion criteria. Of the studies included the reporting of how interventions were carried out is often not sufficient to allow reproducibility or use in practice, with limited details on sets, repetitions, tempo and progressive overload of exercises across all studies.
Of all the studies those using the CFT approach had the most positive effects as measured by disability and pain. The other particularly effective approach was the walking programme of Hurley and colleagues [45] which had the same effect as their exercise group and usual physiotherapy interventions for pain, disability and psychosocial measures but the walking programme had greater adherence and lower costs. This fits with some of the emerging research in whiplash pain which suggests a low cost telephone based intervention was equal to a more expensive and time intensive motor control intervention [61].
A general theme emerging across the studies was the benefits to pain of more specific exercise programmes and the benefits to psychosocial factors through general exercise and psychological input. The admittedly very limited selection of two studies [41,42] suggests that whilst passive interventions could positively affect pain, the addition of general conditioning was required to reduce fear avoidance. Similarly, Vincent, et al. [52] found that the lumbar extensor strengthening was sufficient to increase physical function but the total body programme was required to improve perceived disability and psychosocial measures. Supporting this Geisser, et al. [43] found specific exercise and manual therapy reduce pain whilst their general exercise group had reduced disability.
Improvements in fear avoidance beliefs are often associated with improved function [62] nonetheless in these studies it appears that active treatment such as walking or whole body exercise is required to improve psychosocial measures. There were only two education-based studies but the positive results suggest pain acceptance and neurophysiology education in combination should be useful. The results from intensive functional restoration and CBT programmes suggests these kind of multidisciplinary programmes are effective across all measures, with Pfingsten and Hilderbrandt [34] noting the importance of work hardening in promoting return to work.
The classification based approaches such as Macedo, et al. [56] suggest that there could be future developments allowing clinicians to classify which patients respond best to general exercise and to more general exercise based approaches. In particular patients classified as dysfunctional on the multidimensional pain inventory have been shown to respond best to combined psychosocial and physical input [59].
This systematic review has several limitations. Most obviously, broadening search terms to look for specific psychosocial factors, and specific techniques would allow the inclusion of more papers. This is an inherent issue with study such a broad area as physiotherapy, as compared with specific techniques within the profession. Nonetheless the aim of the review was to see which approaches had been studied and how effective they had been. Furthermore some physical therapy based studies may be missed giving this paper an English bias. Another key limitation is only one researcher being involved in the paper, thus any biases will impact selection, analysis and the writing up of the paper.
Furthermore inferences have been made comparing different interventions and this study design cannot be used to directly compare interventions. However, it would academically dishonest not to point out the trends and to leave the interested reader to use these assertions to inform their clinical judgement as they will.
Considering that CLBP is the leading cause of disability worldwide and those with yellow flags are known to suffer the worst and contribute most to societal cost it is surprising how few studies met the selection criteria. This review has shown that whilst the term yellow flags are used in the assessment literature and guidelines, the term psychosocial and the factors that make it up are used in the treatment literature. The studies selected highlight that passive, active; more comprehensive and simple education interventions can all positively impact the pain experience of this patient group. While the study design does not allow for a direct comparison of treatment approaches, some general trends did emerge. Passive interventions can improve pain, but more whole body active approaches such as whole body weight training or walking may be necessary to positively impact psychosocial symptoms. Comprehensive CBT and functional restoration programmes are effective but the inclusion of work hardening may significantly aid in return to work. Pain education approaches involving pain neurophysiology education and pain acceptance were both effective compared with more traditional back school and pain avoidance approaches respectively. A combination of these may be useful clinically. The CFT approach was the most effective in terms of disability and self reported pain. This review tentatively suggests specific exercise and passive interventions are more beneficial for reducing measures of pain, whilst psychological input and general exercise are more targeted towards psychosocial measures.