Primary testicular lymphoma is a rare extranodal lymphoma accounting for only 1-2% of all Non-Hodgkin's lymphomas. It is the most common neoplasm in patients above 60 years of age. Diffuse large B-cell lymphoma is the most common lymphoma worldwide. It accounts for approximately 30% of all lymphoid malignancies.
We report the case of a 64-year-old male with bilateral diffuse large cell, non germinal centre like B-cell lymphoma of the testes. MRI showed bilateral epididymitis with right sided orchitis and minimal left sided hydrocoele. Right high inguinal orchidectomy was done to confirm the diagnosis. 6 cycles of RCHOP adjuvant chemotherapy was given. He was, however, unable to tolerate the intensive treatment and chemotherapy regimen and succumbed to its adverse effects, 2 months after completion of the 6th cycle.
Primary Testicular Lymphoma is extremely rare with unilateral presentation, making a bilateral testicular lymphoma even rarer. Orchidectomy is the primary choice of intervention to come to a diagnosis. Aggressive systemic therapy offers the only chance there is of remission, but rate of relapse are still quite high.
As primary testicular lymphoma is a rare condition, there is a lack of clinical data to guide the treatment. However, with the aid of retrospective data evaluation, better prognosis may be obtained.
Testicular, Lymphoma, Primary, Chemotherapy, Bilateral
MRI: Magnetic Resonance Imaging; IHC: Immunohistochemistry; PET-CT: Positron Emission Tomography-Computed Tomography; R-CHOP: Rituximab-Cyclophosphamide Hydroxydaunomycin Oncovin Prednisolone; CECT: Contrast Enhanced Computed Tomography; IV: Intravenous; ACLS: Advanced Cardiac Life Support; CNS: Central Nervous System
Primary testicular lymphoma is an extranodal lymphoma in which the primary origin is the testis. It accounts for only 1-2% of all Non-Hodgkin's lymphomas and less than 5% of all testicular tumours [1]. Most of the patients are above 60 years. Primary testicular lymphoma is the most common neoplasm in this age group [2].
Diffuse large B-cell lymphoma is the most common lymphoma worldwide. It accounts for approximately 30% of all lymphoid malignancies. It is heterogeneous in morphologic appearance, immunophenotype, and biological behaviour, including response to chemotherapy and ultimate outcome [3].
A 64-year-old male came with the chief complaints of enlargement of both his testes since 6 months. It began with the right testis and then went on to include the left testis as well. Both testes gradually increased in size, insidiously, over 6 months, and were painless. There were no associated symptoms and no decrease in size. He was a known hypertensive with ischemic heart disease.
On examination he had none of the general signs of systemic disease such as pallor, icterus, clubbing, cyanosis, generalized lymphadenopathy or pedal oedema and his vitals were stable.
The right testis was larger than the left measuring 10 × 8 cm. It was hard in consistency and non-tender. The left testis measured 8 × 7 cm and had a variable consistency with intervening cystic areas in a solid mass. The spermatic cord on the right was impalpable whereas on the left it was thickened and hard. The scrotal skin was free from the swellings and there were no palpable inguinal nodes.
Systemic examination revealed no findings.
He was admitted under the department of general surgery in Justice K.S. Hegde Charitable Hospital, Mangalore in April 2019. He underwent an MRI pelvis which showed bilateral epididymitis with right sided orchitis and minimal left sided hydrocoele. As this report was not convincing, he underwent a right high inguinal orchidectomy on 10th May 2019 (Figure 1).
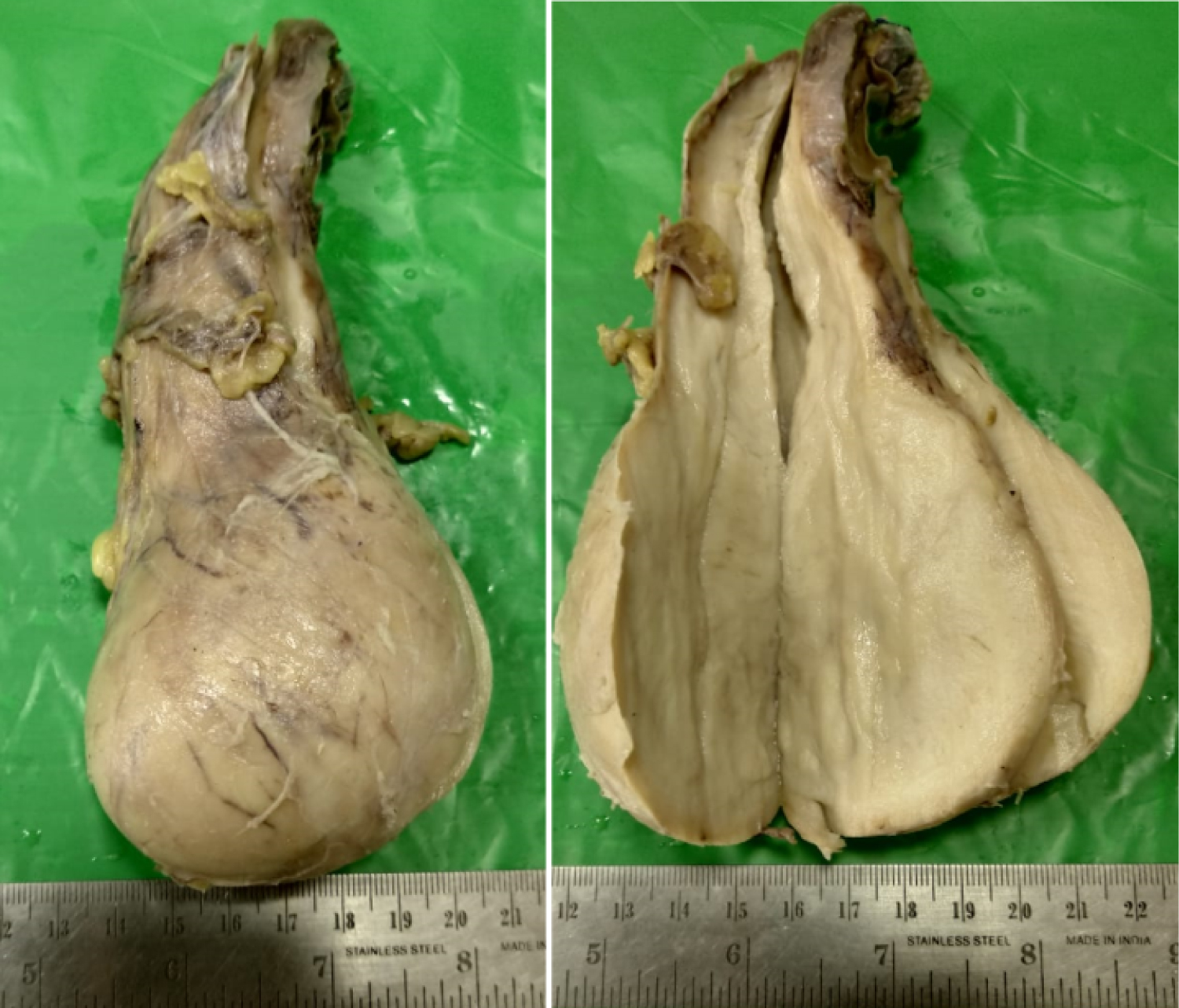 Figure 1: Gross appearance of the specimen.
View Figure 1
Figure 1: Gross appearance of the specimen.
View Figure 1
Histopathology showed it to be Non-Hodgkin's lymphoma of the right testis. Subsequent IHC marker study was suggestive of diffuse large cell, non germinal centre like B-cell lymphoma testis (Figure 2).
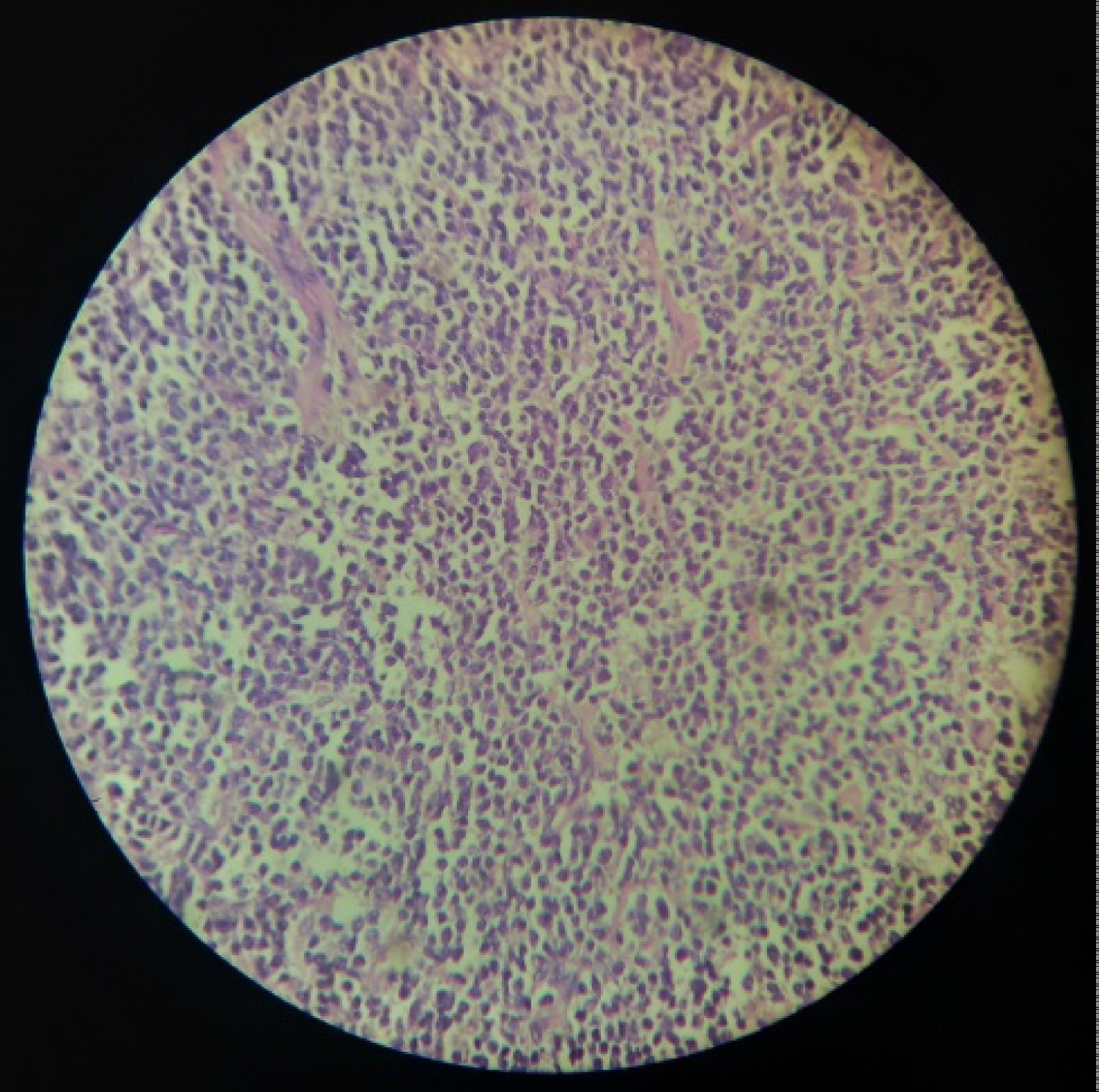 Figure 2: Histology of the testicular specimen.
View Figure 2
Figure 2: Histology of the testicular specimen.
View Figure 2
A PET-CT was done on 8th June 2019 which showed the following (Figure 3):
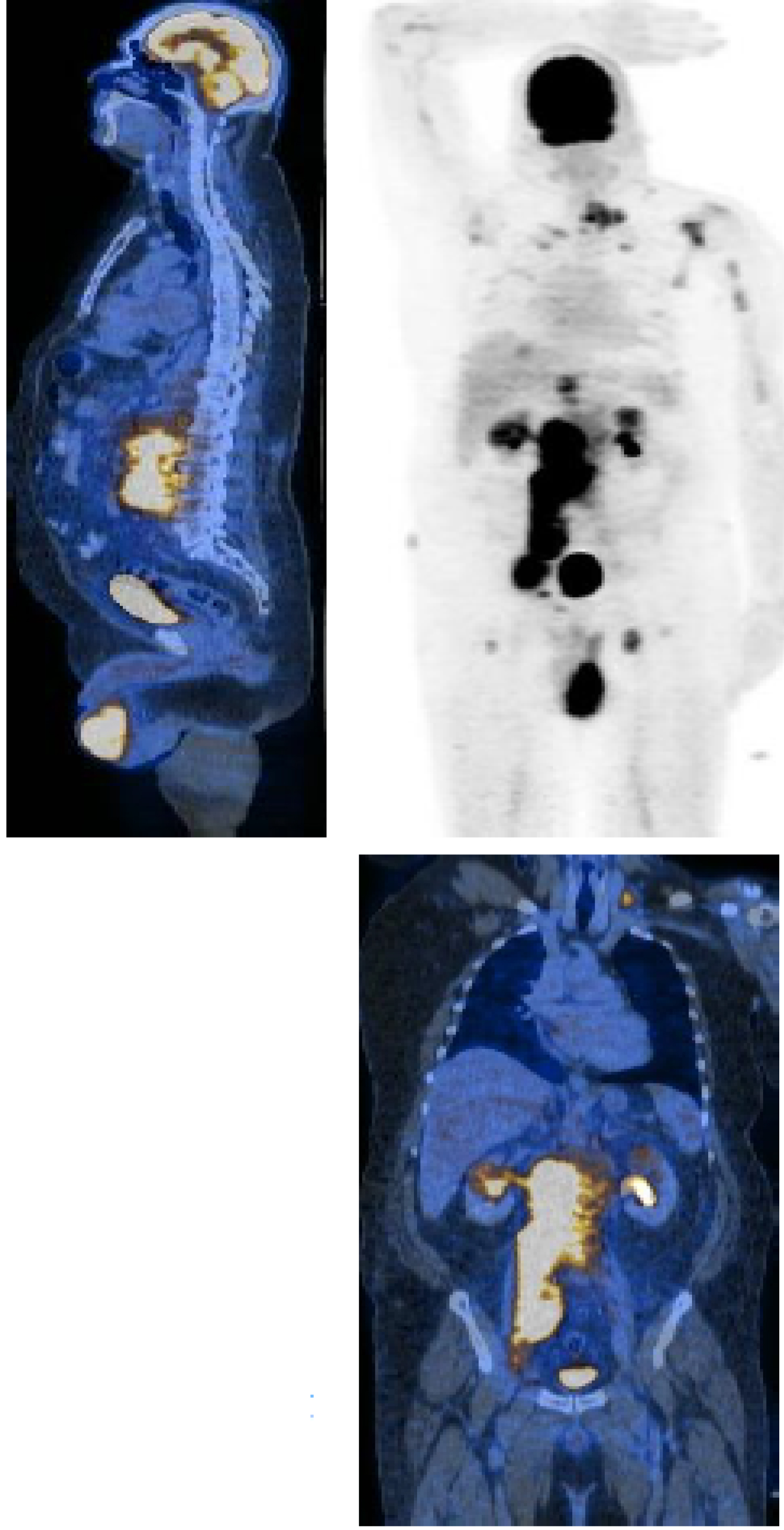 Figure 3: PET-CT images.
View Figure 3
Figure 3: PET-CT images.
View Figure 3
• Confluent/discrete retroperitoneal, retrocrural, bilateral iliac, inguinal, left cervical and supraclavicular lymphadenopathy.
• Prominent mediastinal, mesenteric, supradiaphragmatic, periportal, portocaval and left axillary lymph nodes.
• Metabolically active deposits in bilateral renal cortex.
• Bulky metabolically active left testis.
• Metabolically active marrow deposits.
• Metabolically active soft tissue in the left C6-C7 neural foramen extending to the adjacent epidural and paravertebral space.
• Patchy ground glass and consolidative opacities in both lungs.
• Trace bilateral pleural effusion.
• Mild bilateral hydronephrosis.
A medical oncology reference was given and a multidisciplinary team meeting was held. The patient was subsequently started on R-CHOP regimen as adjuvant chemotherapy. He received 6 cycles of chemotherapy that ended on 16th October 2019.
2 weeks after the 6th cycle, he was readmitted with complaints of low backache and inability to bear weight with pain in both his thighs. Physiotherapy was started to improve his symptoms as per Orthopaedic and Neurology advice. Medical oncology advised to start high dose methotrexate with rituximab to prevent a CNS relapse. He received 3 cycles of the same along with high dose of steroids (Prednisolone 20 mg thrice daily) for the bone pain.
In December 2019, he developed cardiopulmonary symptoms for which he was evaluated and managed appropriately. He was found to have acute necrotizing pancreatitis with peripancreatic fluid collection with a grossly elevated serum amylase (4036.6 IU/L) and serum lipase (33386 IU/L).
Eventually, he developed multi-organ dysfunction requiring haemodialysis, ionotropic and ventilatory support. On 28th December 2019, he had a cardiopulmonary arrest in the late evening and passed away the same night.
Primary testicular lymphoma is an extremely rare tumour when it presents unilaterally making our case of a bilateral diffuse large B-cell lymphoma even rarer. This case fits the description of the presenting features as described in previous case reports [1]. However, the fact remains that it is very difficult to differentiate a primary testicular lymphoma from a manifestation of a generalized lymphomatous disease.
Testicular lymphomas have a characteristic pattern of dissemination with frequent involvement of contralateral testis, bones, and lungs as was seen in this case as well. Skin, CNS, Waldeyer's ring and adjacent structures are also frequently involved, but were not seen in this case [4]. Based on this pattern of spread, the presenting symptoms and the course of the disease, we can suspect a primary testicular pathology rather than the involvement of the testes in a generalized disease.
Suboptimal treatment usually occurs in these cases because of poor clinical performance or intolerance to the intervention [5]. Orchidectomy is the primary intervention to come to a diagnosis in most cases, as was seen with our case.
As previously described in a case report by Cakiroglu, et al. 6 cycles of RCHOP were given for this patient in view of stage 4 disease on PET-CT [6].
CNS relapse is a fairly common occurrence in primary testicular lymphoma. High dose methotrexate given orally or intrathecally has been shown to lower the risk of CNS relapse significantly [7].
Adjuvant radiotherapy has been shown to improve survival, but this has more value in limited stage disease. Data is limited regarding the benefit of regional nodal irradiation in advanced disease and hence, it is not routinely recommended. Acute cutaneous toxicity, lethargy, nausea, hypogonadism and infertility are some of the complications associated with locoregional radiotherapy to the scrotum [7].
Thus, for patients with advanced stage disease, a combination of systemic chemotherapy, CNS prophylaxis and radiotherapy is required [8]. Following 6 cycles of RCHOP as systemic chemotherapy, our case received high dose methotrexate for CNS prophylaxis. However, he was unable to receive radiotherapy as his condition deteriorated soon after the completion of chemotherapy.
According to a study done by Jiang H, et al. higher Ann Arbor stage, B symptoms and extranodal involvement other than testes were poor prognostic indicators. A high stage and extranodal involvement were both present in our case. The study also showed preliminary evidence that bilateral intervention, either by radiotherapy or orchidectomy, had the potential to improve survival [9]. In our case, however, the patient was not willing for surgery and was unable to undergo radiotherapy.
Aggressive systemic treatment is the preferred approach to achieve clinical remission. However, even with extensive systemic chemotherapy, relapse rates are high in patients with testicular lymphoma [8]. In this case, however, we were unable to get documented remission as a repeat PET-CT was not done. He probably succumbed to the intensive chemotherapy regimen which points to the fact that treatment for testicular lymphoma requires further clinical research and understanding.
Primary testicular lymphoma is a rare disease. Hence, there is a lack of data that can guide the treatment. However, with the aid of retrospective data evaluation, better prognosis may be obtained. Despite the improvements in local and systemic disease, CNS relapse remains the worst complication. Strategies that may decrease the risk of primary testicular lymphoma in patients, will end up with better prognosis.
This case report has been made by Dr. Rishabh Agarwalla under the guidance of Dr. Rajashekar Mohan in K. S. Hegde Medical Academy, a unit of Nitte (Deemed to be) University in consultancy with Dr. Vijith Shetty.