The study aimed to determine the efficacy of single dose of glucocorticoid (125 mg of Solumedrol intravenous) in terms of seroma formation after mastectomy in patient with carcinoma of breast.
Randomized controlled trial.
Study was conducted in the Department of General Surgery, Liaquat National Hospital Karachi, Pakistan from July 1 to Dec 31, 2010.
Patients were randomly divided in two groups (study and control) each group consisting of 30 patients. Randomization was done by opening of a sealed envelope which had a slip bearing the name of study medication (solu-medrol or saline as placebo) to be administered. The study group received a single dose of inj 125 mg solu-medrol IV half an hour prior to surgery by resident scrub in surgery. A similar procedure was applied to the control group and patients in controlled group were administered an equal volume of saline intravenously. After drain removal patients in both groups were observed for duration of 2 weeks for sermoa formation. Detection of seroma formation was based on clinical grounds by absence of any fluid collection at mastectomy bed as detected by manual palpation. SPSS 10 was used for analysis.
Seroma formation was observed in 66.7% (40/60) women 2 weeks post drain removal. Rate of seroma formation was significantly low in study groups than control groups (33.3% vs. 100%; p = 0.0001).
Single dose of steroid is efficacious in reducing the post mastectomy seroma formation.
Post mastectomy seroma formation, Steroid and seroma, Factors for seroma formation, How to reduce seroma formation post mastectomy, Mastectomy, Seroma
Seroma is a post operative fluid collection requiring one or more aspirations or subsequent drain placement following surgery. It is a common occurrence following surgery. The incidence rate of seroma formation following breast surgery is up to 30% to 92% [1]. It is often an ongoing problem after removal of the suction drain, and repeated skin puncture is necessary to remove the seroma. Seroma formation is most likely the result of the inflammatory response due to wound healing. Comparison of drain fluid to plasma ratios with known lymph to plasma values for biochemical parameters showed that this fluid is compositionally different from lymph, but is similar to inflammatory exudates [2]. In the seroma fluid several factors have been detected that support this assumption. These factors are: High levels of IgG, leucocytes, granulocytes, proteinases, proteinases inhibitors, different kinds of cytokines (tPA, uPA, uPAR, PAI-1, PAI-2, IL-6, IL-1). The modulation of acute phase response may have important implications for patients with cancer undergoing surgery [3]. On the basis of this understanding, an inhibition of the inflammatory response might result in a decrease in seroma formation, and perhaps improve quality of life after mastectomy. Steroids inhibit the inflammatory response for example by inhibition of the cytokine function. It has been shown that a high single dose of steroid infusion (30 mg/kg solu-medrol) inhibits the normal IL 6 response after colon resection. While there are no studies on the use of solu-medrol in breast cancer, the use of triamcinolone in breast reconstruction surgery demonstrated than 55% did not have seroma formation whereas 95% developed seroma in those administered saline [4].
The exact etiology of seroma formation remains controversial. Several interventions have been reported with the aim of reducing seroma formation including the use of ultrasound scissors in performing quilting [5], buttress suture [6], lymphadenectomy [7], fibrin glue [8], fibrin sealant [9], bovine thrombin application [10], and altering surgical technique to close dead space [11].
The seroma formation after breast cancer surgery is independent of duration of drainage, compression dressing and other known prognostic factors in breast cancer patients except the type of surgery, i.e there is a 2.5 times higher risk of seroma formation in patients undergoing MRM compared to BP [12].
It is the possibility of decreased seroma formation with the use of steroids that we propose to undertake this study. It is proposed to use a single dose of 125 mg solu-medrol intravenously in this study.
Seroma: Presences of clear fluid filled pockets in the body post operatively; Efficacy: Efficacy will be deemed posture as when no seroma formation at the end of 4 weeks; Carcinoma Breast: Biopsy proven breast cancer lobular or infiltrative ductal.
Study design: Randomized controlled trial; Setting: Study was conducted in the Department of General Surgery, Liaquat National Hospital Karachi, Pakistan from July 1 to Dec 31, 2010; Duration of study: 6 months, patients in each group were observed for seroma formation for 2 weeks after drain removal; Sample technique: Non probability purposive; Sample Size: Assuming the efficacy of solu-medrol 55% and saline 15% [12], level of significance 5% and power of test 90%, simple size required was 46 but we took 60 patient (considering lost to follow up) 30 patient in each group [4].
Sample Selection: Inclusion criteria:
• Women with primary breast cancer up to stage III, planned for a mastectomy with axillary dissection.
• Age over 25 years.
• Age over 25 years.
Exclusion criteria:
• Men
• Treatment with glucocorticoids within the last month before surgery, including inhalation products
• Pregnant.
• Severe heart disease
• Treatment with carbamazepine, phenytoin, Phenobarbital, rifampicin, salicylates and cyclosporine
• Uremia
• Diabetes
• Post neo-adjuvant and adjuvant chemotherapy.
Patients found eligible as per inclusion criteria were offered to participate in the study. Those giving informed consent were included. A proforma was filled for each patient to record. Mastectomy with axillary clearance was performed by consultant (with 15 years of experience) in breast surgery. Each patient enrolled in the study was eligible to be enrolled into either arm of the study following the opening of a sealed envelope which had a slip bearing the name of study medication (solu-medrol or saline as placebo) to be administered. Most senior resident scrubbed in case was choosing the envelope and afterwards it was handed over to anesthetist who used to administer the randomized drug pre operatively to the patient during induction. The study group received a single dose of inj 125 mg solu-medrol IV half an hour prior to surgery by resident scrub in surgery. A similar procedure was applied to the control group and patients in controlled group were administered an equal volume of saline intravenously. Patients in both groups were followed postoperatively until 2 weeks after drain removal. An absence of clear fluid filled pocket in the mastectomy bed was documented in the proforma by a resident attending the OPD.
Data was entered and analyzed by using statistical package for social sciences (SPSS) version 11.0 software. Frequencies and percentages were computed for categorical variables like age groups, stages of breast cancer, seroma formation and efficacy. Mean, standard deviations, 95% confidence interval, median with IQR were calculated for quantitative variables like age of patient. Chi-square test and fisher's exact test was applied to compare proportion difference between groups for efficacy. Independent sample t test was applied to compare mean difference between groups for age. P ≤ 0.05 was considered significant. Confounding variables like age and stages of carcinoma were controlled by stratification to observed effect on outcome.
A total of 60 women with primary breast cancer planned for a mastectomy with axillary dissection were included in this study. Patients were equally divided into two groups. The study group received a single dose of inj 125 mg solu-medrol IV half an hour prior to surgery and similar procedure was applied to the control group who were administered an equal volume of saline. Overall age distribution of the patients is presented in Figure 1. The average age of the patients was 52.32 ± 9.86 years (95% CI: 49.77 to 54.86) as shown in Table 1. Significant difference was not observed between group in average age (52.62 ± 8.42 vs. 52 ± 11.25; p > 0.05) as presented in Figure 2.
Table 1: Descriptive statistics of age of the patients; n = 60. View Table 1
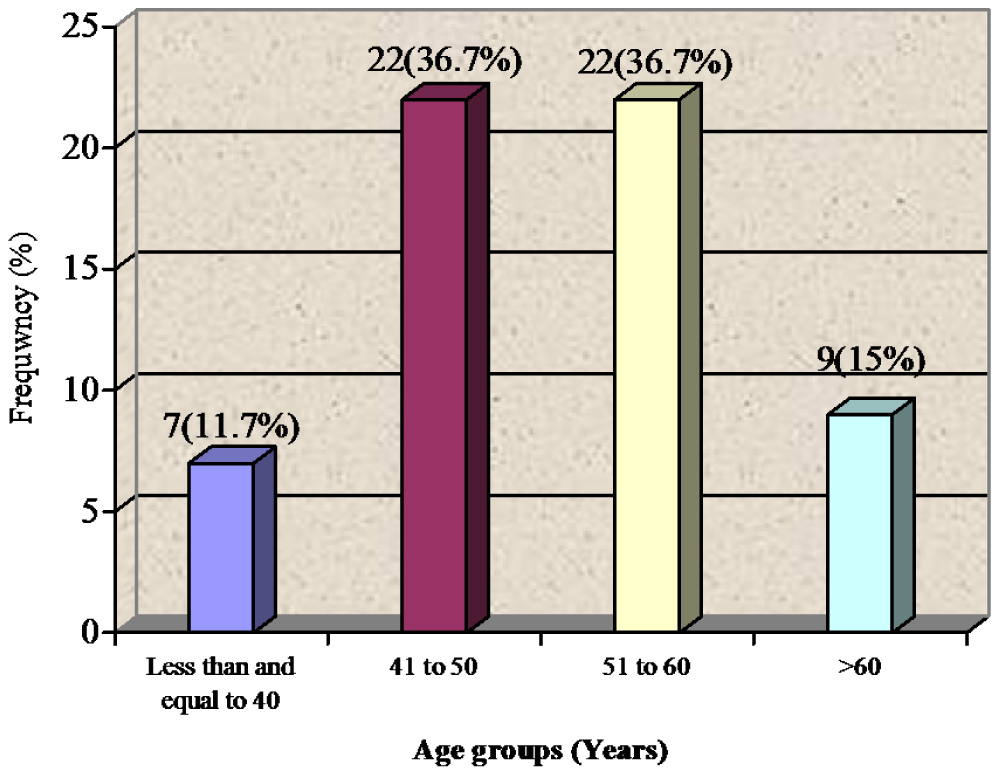 Figure 1: Age distribution of the patients; n = 60.
View Figure 1
Figure 1: Age distribution of the patients; n = 60.
View Figure 1
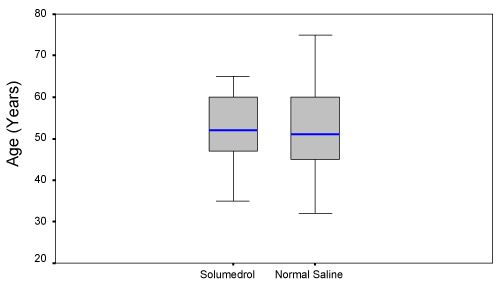 Figure 2: Comparison of age between groups.
View Figure 2
Figure 2: Comparison of age between groups.
View Figure 2
Regarding stages of carcinoma, 4 (7%) women were in stage 1A, 14 (23%) were in stage 2A 22(37%) were in stage 3A and 20 (33%) women were observed with stage 2B carcinoma as presented in Figure 3.
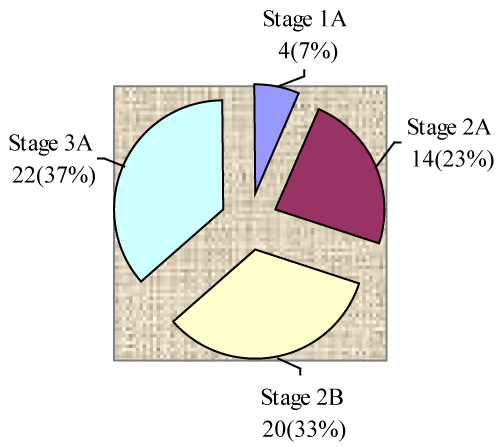 Figure 3: Stages of breast cancer; n = 60.
View Figure 3
Figure 3: Stages of breast cancer; n = 60.
View Figure 3
Seroma formation was observed in 66.7% (40/60) women 2 weeks post drain removal. Rate of seroma formation was significantly low in study groups than control groups (33.3% vs. 100%; p = 0.0001) as shown in Table 2. Comparisons of efficacy in term of seroma formation in women with primary breast cancer after mastectomy with axillary dissection are presented in Table 3. Efficacy of the treatments was significantly high in study group (Solumedrol) than control (66.7% vs. 0%; p = 0.0001). Similarly effectiveness of solu-medrol was significantly high with respect to age as presented in Table 4, Table 5 and Table 6 and it was also significantly effective in stage 2A, stage 3A and stage 2B as presented in Table 7, Table 8 and Table 9.
Table 2: Comparison of seroma formation between groups. View Table 2
Table 3: Comparison of efficacy between groups. View Table 3
Table 4: Comparison of efficacy between groups for below and equal to 50 years of age. View Table 4
Table 5: Comparison of efficacy between groups for above 50 years of age. View Table 5
Table 6: Comparison of efficacy between groups for stage 1A of breast cancer. View Table 6
Table 7: Comparison of efficacy between groups for stage 2A of breast cancer. View Table 7
Table 8: Comparison of efficacy between groups for stage 2B of breast cancer. View Table 8
Table 9: Comparison of efficacy between groups for stage 3A of breast cancer. View Table 9
The documented effect of triamcinolone as a potent anti-inflammatory agent could perhaps be suggestive of its mechanism in seroma management. It is a synthetic glucocorticoid frequently used to treat autoimmune and allergic conditions. It suppresses the inflammatory process by formation of phospholipase inhibitor lipocortin, which diminishes the supply of arachidonic acid available for synthesis of prostaglandin and leukotrienes. As a result capillary permeability, oedema, migration of leucocytes, and later signs of capillary proliferation, and fibroblast and collagen deposition are inhibited. This study has demonstrated the effect of solu-medrol in reducing seroma re-accumulation, which would perhaps suggest the inflammatory mechanism to be significant in seroma formation. The use of solu-medrol is therefore an inexpensive and simple means of seroma management. Moreover we found no added significant complications with this technique, in particular infective complications given the potential immune compromising effect of steroid.
In this study a total of 60 women with primary breast cancer planned for a mastectomy with axillary dissection were included. Patients were equally divided into two groups. The study group received a single dose of inj 125 mg solu-medrol IV half an hour prior to surgery and similar procedure was applied to the control group who were administered an equal volume of saline. The average age of the patients was 52.32 ± 9.86 years (95% CI: 49.77 to 54.86). Significant difference was not observed between group in average age (52.62 ± 8.42 vs. 52 ± 11.25; p > 0.05).
Regarding stages of carcinoma, 4 (7%) women were in stage 1A, 14 (23%) were in stage 2A 22 (37%) were in stage 3A and 20 (33%) women were observed with stage 2B carcinoma.
Seroma formation was observed in 66.7% (40/60) women. Rate of seroma formation was significantly low in study groups than control groups (33.3% vs. 100%; p = 0.0001). Efficacy of the treatments was significantly high in study group (Solumedrol) than control (66.7% vs. 0%; p = 0.0001). Similarly effectiveness of solu-medrol was significantly high with respect to age and it was also significantly effective in stage 2A, stage 3A and stage 2B.
While there are no studies on the use of solu-medrol (but easily available in our setup) in breast cancer, the use of triamcinolone (which has same mode of action and duration like solu-medrol) in breast reconstruction surgery demonstrated than 55% did not have seroma formation whereas 95% developed seroma in those administered saline [12]. It is the possibility of decreased seroma formation with the use of steroids that we propose to undertake this study.
The small sample size of present study is a limitation and hence the power of the study is low. A number of questions remain unanswered and more research is needed to answer these.
Single dose of steroid is efficacious in reducing the post mastectomy seroma formation which helps in timely administration of chemotherapy and reduce the risk of infection, necrosis and sepsis and improve quality of life. Steroids may have applications in managing other seromas of similar etiology, such as those after abdominoplasty and hernia mesh repair.