Introduction: The etiology of hernias involves changes in the expression of different components of the extracellular matrix, which especially affect the fascia transversalis (FT), such as collagen, the elastic component and metalloproteinases (MMP). On the other hand, there is an overexpression of MMP-2 in the FT of young patients with direct inguinal hernia, correlated with an increase in TGF-beta1 that shows an attempt to counteract an increased process of degradation of the extracellular matrix in these patients.
Clinical case: A 63-year-old female with a family history of maternal grandmother with bilateral and umbilical inguinal hernia, father with retinal detachment and inguinal hernia, pathological personal history of essential arterial hypertension, dyslipidemia, and multiple hemangiomas distributed throughout the body. She comes to consult due to increased volume in the right inguinal region for 3 years, in the left inguinal region for two years, both without treatment, which increased with the Valsalva maneuver and currently one in the umbilical region, denying nausea, vomiting, fever, pain or constipation. Physical examination, skin color unchanged, reducible, not incarcerated, not strangled. The diagnostic protocol was started where the presence of bilateral inguinal and umbilical hernia was evidenced, for which a surgical programming was decided to perform abdominal wall plasty. Right and left inguinal plasty with mesh and umbilical plasty without mesh were performed.
Discussion: In the last 30 years, research on the etiopathogenesis of abdominal wall hernias has revealed that one of the causes is due to multifactorial systemic tissue disease, currently known as herniosis.
Hernia, Abdominal wall, Metalloproteins, Collagen, Elastin
The etiology of hernias involves changes in the expression of different components of the extracellular matrix, which especially affect the fascia transversalis (FT), such as collagen, the elastic component and metalloproteinases (MMP). On the other hand, there is an overexpression of MMP-2 in the FT of young patients with direct inguinal hernia, correlated with an increase in TGF-beta1 that shows an attempt to counteract an increased process of degradation of the extracellular matrix in these patients. At the level of the elastic tissue of the FT, patients with hernia show lower levels of tropoelastin (TE), monomers that make up elastin, and lysyloxidase like-1 (LOXL-1), an enzyme involved in elastin crosslinking. All this is accompanied by a significantly higher expression of elastase, the main enzyme involved in the process of elastin degradation. In cell cultures from FT, the levels of mRNA encoding LOXL-1 were also found to be significantly lower in patients with direct inguinal hernia.
All these alterations highlight a disorder at the level of the extracellular matrix of the connective tissue in patients with inguinal hernias, which together with other exogenous factors (smoking, mechanical stress, tissue aging, etc.) would partly explain the genesis of this pathology [1,2].
A 63-year-old female with a family history of maternal grandmother with bilateral and umbilical inguinal hernia, father with retinal detachment and inguinal hernia, pathological personal history of essential arterial hypertension, dyslipidemia, and multiple hemangiomas distributed throughout the body. She comes to consult due to increased volume in the right inguinal region for 3 years, in the left inguinal region for two years, both without treatment, which increased with the Valsalva maneuver and currently one in the umbilical region, denying nausea, vomiting, fever, pain or constipation. Physical examination, skin color unchanged, reducible, not incarcerated, not strangled. The diagnostic protocol was started where the presence of bilateral inguinal and umbilical hernia was evidenced, for which a surgical programming was decided to perform abdominal wall plasty (Figure 1, Figure 2 and Figure 3). Right and left inguinal plasty with mesh and umbilical plasty without mesh were performed (Figure 4 and Figure 5). The patient is discharged 24 hours after the procedures were performed. In her follow-up, the patient is asymptomatic and incorporated into her daily activities.
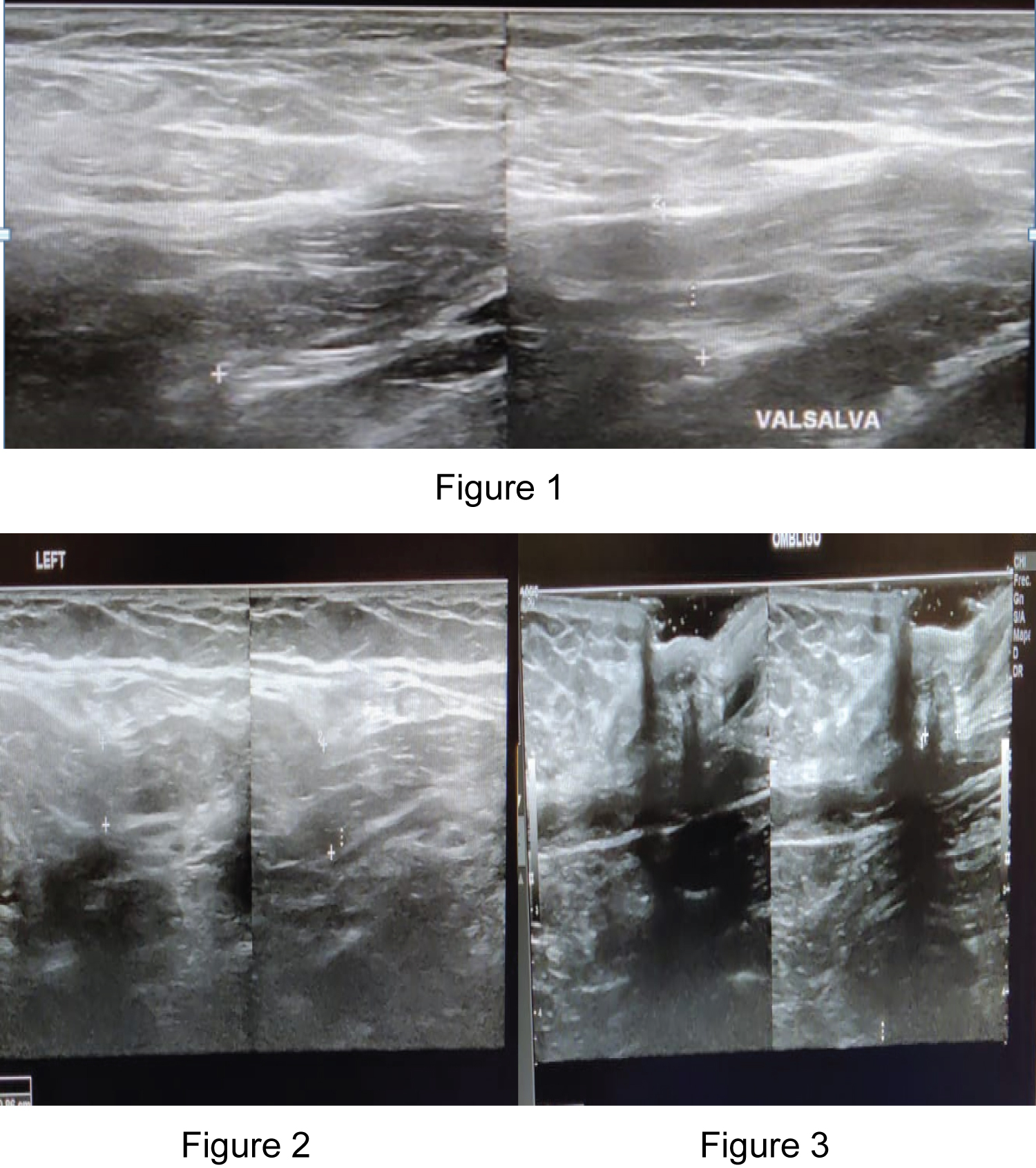 Figure 1, 2 and 3: The diagnostic protocol was started where the presence of bilateral inguinal and umbilical hernia was evidenced, for which a surgical programming was decided to perform abdominal wall plasty.
View Figure 1, 2 and 3
Figure 1, 2 and 3: The diagnostic protocol was started where the presence of bilateral inguinal and umbilical hernia was evidenced, for which a surgical programming was decided to perform abdominal wall plasty.
View Figure 1, 2 and 3
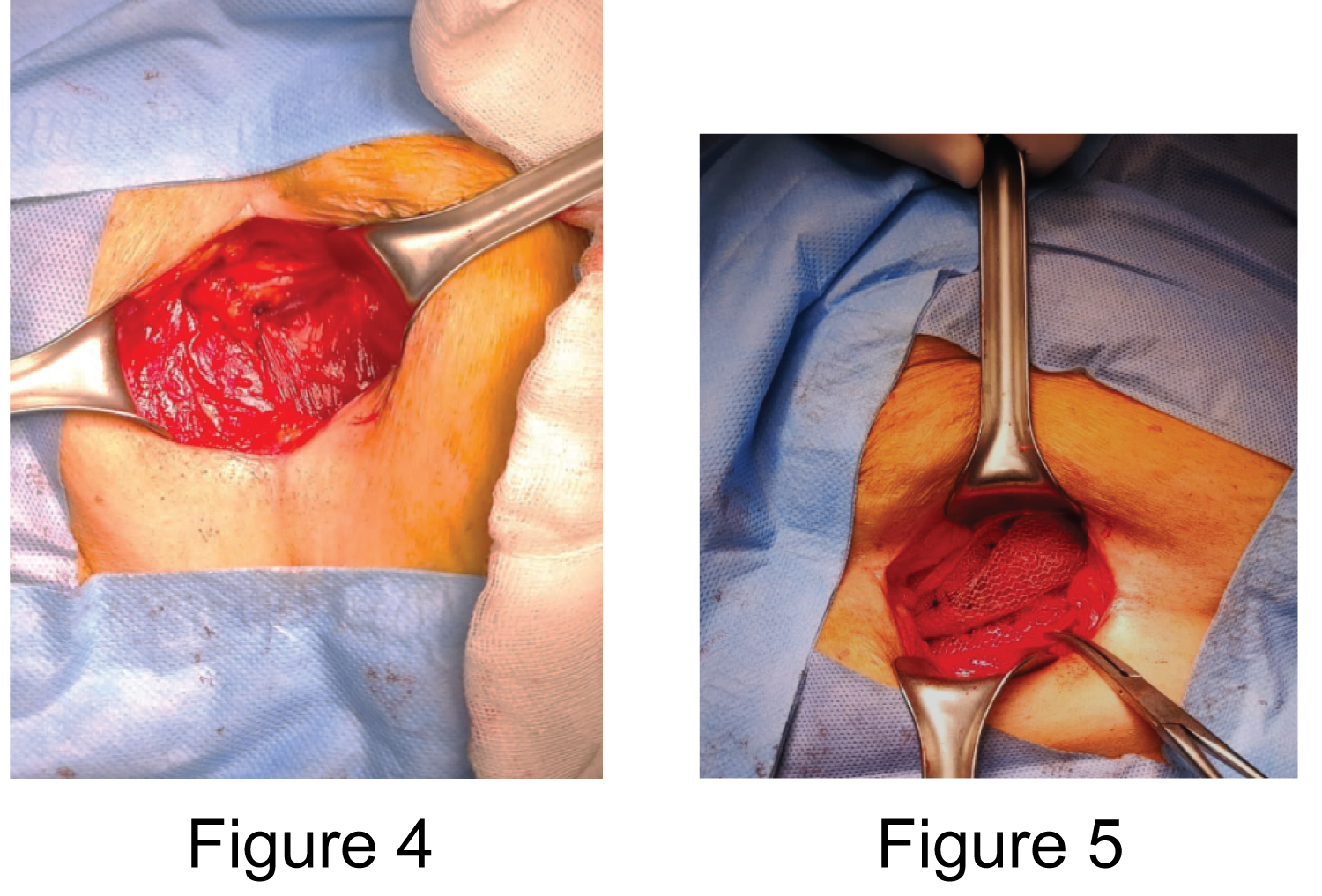 Figure 4 and 5: Right and left inguinal plasty with mesh and umbilical plasty without mesh were performed.
View Figure 4 and 5
Figure 4 and 5: Right and left inguinal plasty with mesh and umbilical plasty without mesh were performed.
View Figure 4 and 5
In the last 30 years, research on the etiopathogenesis of abdominal wall hernias has revealed that one of the causes is due to multifactorial systemic tissue disease, currently known as herniosis [1]. Defined as a systemic disease of the connective tissue originating in the extracellular matrix and related to a deficient or abnormal production of collagen (collagenosis), or with its accelerated or increased degradation, mediated by proteolytic enzymatic processes [2] and linked to hereditary and environmental factors. Herniosis carriers often have multiple hernias (primary, recurrent, and incisional) and a high recurrence rate when repaired. Abdominal wall hernias are the following: direct or indirect inguinal hernias; femoral hernia; umbilical hernia; epigastric or white line hernias; Spigiel's hernia; athlete's hernia; traumatic hernia; obturator foramen hernia; intraparietales hernias [3-6].
In the muscular structures, thinning of the muscle fibers and separation of the bundles with herniation of the preperitoneal fat in their interstices are observed. These findings alone should alert about the coexistence of other pathologies. On the other hand, it is convenient to know that patients with herniosis (collagenosis) are prone to present higher rates of recurrence and complications when they undergo surgical procedures and, in addition, to have higher risks of complications.
Another aspect to consider is the fact of suspecting coexisting multiple pathologies, even in their asymptomatic form due to the predisposition conferred by collagenosis and which, when ignored, can be complicated by not being detected. Examples of this are the association of emphysema and chronic obstructive pulmonary disease, or herniated varicose veins, which can increase the risk of serious complications in the postoperative period, such as pulmonary thromboembolism. These pathological conditions should be investigated in patients with hereditary collagen disorders, such as Ehlers-Danlos disease, Marfan syndrome in its incomplete or atypical forms [7,8].
Abdominal hernias have a multifactorial cause, such as the weakness of the wall that contains them due to a disease of the extracellular matrix with deficient collagen production, making carriers more susceptible to suffering from them and the appearance of recurrences, so that patients with multiple hernias should be studies looking for defects in the extracellular matrix.