Functional disorders of the pelvic floor are common healthcare problems owing to increased incidence of obesity, pelvic surgeries, childbirth, heavy physical exertion etc. In the past, fluoroscopic defecography was used in their diagnosis, but it had its limitations like radiation exposure. Endoanal sonography and Magnetic Resonance Imaging (MRI) were also used to assess the pelvic pathologies but they could not assess the pelvic floor function. Magnetic Resonance Defecography (MRD) is a new modality that has come up over the years which allows dynamic imaging of the pelvic floor during defecation and thus plays a role in diagnosing these disorders.
To study the technique, applications and limitations of MR Defecography in evaluating Pelvic Floor Dysfunctional Disorders.
Twenty one patients of age range 20-80 years with suspected pelvic floor dysfunction referred to undergo MR Defecography scanning were included. For scanning Wipro GE Healthcare 1.5 Tesla MRI machine was used. Ultrasound jelly was instilled into the rectum of patient and was asked to defecate when instructed. Scanning was done in four phases-resting, straining, squeezing and defecation as per the standard protocol. Studies were interpreted using the parameters mentioned in literature and results were analyzed.
Most common complaint encountered was that of sense of incomplete defecation. Out of 21 patients, 11 were found normal and 31 were found to have one of the pelvic floor dysfunction disorder. Out of these, 21% were diagnosed as Spastic Perinuem Syndrome, 19% as Pelvic Floor Dysynergia, 14% were found to have Rectal Prolapse, 9% had Rectocoele, in 4.5% each Uterine prolapse and Cystocoele was found. Obstructive defecation disorders are more common in middle age, while the relaxing type which include Pelvic organ prolapse are more common in either younger age or elderly age. Obstructive defecation disorders are more common in males while Organ prolapse is more common in females.
MR Defecography is a new modality that invariably helps in diagnosing Pelvic floor functional pathologies. Based on the pelvic floor function during defecation, the disorders can be classified into two i.e Relaxing and non-relaxing types. In the past, fluoroscopic defecography was used in their diagnosis, but it had its limitations like radiation exposure. MR Defecography is a novel tool that enables real-time imaging of the defecation function, providing a multiplanar information. Also, good temporal resolution, high soft-tissue contrast and lack of radiation exposure, make it the preferred imaging modality for evaluation.
Magnetic resonance defecography, Pelvic floor dysfunctional disorders, Obstructed defecation syndrome, Organ prolapse, Spastic perineum syndrome, Pelvic floor dyssynergia, Rectal prolapse, Rectocoele, Uterine prolapse
MRI: Magnetic Resonance Imaging; MR: Magnetic Resonance; STIR: Short Tau Inversion Recovery; PCL: Pubo-coccygeal line
Pelvic floor dysfunctional disorders is an umbrella term for a variety of disorders in which the pelvic floor muscles and ligaments are impaired leading to the patient losing his ability to control them voluntarily. These are increasingly becoming a common health care problem owing to greater compromise of the integrity of pelvic floor because of obesity, vaginal delivery, pelvic surgeries, constipation, age and heavy physical exertion, all of these becoming important risk factors for the same [1].
The patients suspected with pelvic floor dysfunction disorders present with a variety of symptoms. These can range from dysfunctional defecation symptoms like chronic constipation, sense of incomplete evacuation, tenesmus i.e. recurrent urge to defecate, excessive straining, rectal pain etc. to gross organ protrusions per rectum or per vaginum, urinary or fecal incontinence [2].
The diagnostic approach to these disorders has been by means of clinical examination followed by various radiological investigations that came up over the years like fluoroscopic defecography, micturating cystourethrography, endoanal Ultrasound, Pelvic MRI, Endoanal MRI etc. While all of them came with advantages of their own in assessing pelvic pathologies but none of them proved to be an adequate tool to assess the pelvic floor function.
MR Defecography has emerged over the last decade as a modality which additionally images the pelvic floor function in real time besides combining the advantages of previously used modalities and that of magnetic resonance i.e. multiplanar imaging, good temporal resolution and lack of radiation exposure [3].
Thus the aim of this research is to study the diagnostic utility of MR Defecography in evaluation of Pelvic floor disorders, explaining its methodology, the protocol, the anatomical description and characterization of these disorders on a preliminary basis in the light of literature.
Twenty one patients suspected with pelvic floor dysfunction having symptoms of either obstructive defecation or organ prolapse referred to the department of Radiology for MR Defecography were studied. History was obtained from the patient and clinical findings were recorded. MR Defecography procedure was performed as per the standard protocol, observations were made and findings were interpreted based on the parameters mentioned in the literature and results were analyzed.
Scans were performed on 1.5 Tesla Wipro GE Healthcare (Optima 360-16Ch) MRI machine having a tunnel configuration using a standardized protocol. No prior bowel or rectal preparation was done. The procedure requires patient to follow instructions through various phases of defecation hence the procedure is first coherently explained to the patient, answering their queries and after taking proper consent the scan was carried out. Patient is made to lie supine, feet first on the MRI machine gantry. A sagittal localizer is acquired with high resolution T2 weighted FSE sequence. From this series, a midsagittal slice is chosen and transcribed to a new series in which this slice is repeated 15 times at 2-second intervals for each phase. Sequences are taken in following phases.
STIR and T2 weighted static scans of pelvis at rest.
Patient is made to lie in left lateral decubitus position and 180-220 cc of ultrasound jelly is instilled into the rectal lumen using a rectal tube. Sequences are repeated when rectum is fully distended.
Patient is then asked to perform various maneuvers through the whole procedure during which T2/STIR sequences are taken.
Patient is asked to squeeze pelvic floor upwards and images are acquired.
Patient is asked to apply strain and bear down effort and imaging is done.
Patient is asked to completely defecate the ultrasound jelly and FIESTA B4 sequence is obtained in sagittal plane repeating a single slice 15-25 times at the same slice position. These images are viewed in cine loop format to view the defecation action.
When the patient has defecated all the jelly, a post evacuation scan is acquired.
The pelvic cavity contains urinary bladder, reproductive organs, rectum anus, pelvic muscles, ligaments and connective tissue keeping all of them in place.
All these pelvic structures are provided with a plate like floor of muscles of which levator ani muscle forms the most important component. This muscular pelvic floor provides support to the abdomino-pelvic contents against the intra-abdominal pressure by maintaining a constant state of contraction [4]. The urogenital hiatus which is just below this levator hiatus is kept in a closed state due to this baseline activity of levator muscle, thereby keeping the urethral, vaginal and anorectal distal segments towards the pubic bone and maintain their contractility [4]. The relaxation of levator ani muscle occurs during voluntary action of evacuation like urination or defecation.
The plate like Levator ani of pelvic floor is constituted by three muscles i.e. pubo-coccygeus, Puborectalis and ilio-coccygeus. The pubo-coccygeus is further divided into pubo-vaginalis, pubo-analis and pubo-perinealis components [4]. The pubo-analis elevates the anus and together with rest of pubococcygeus and Puborectalis keeps the uro-genital hiatus closed. The Puborectalis arises from either side of pelvic wall and passing posterior to the anorectal junction it forms a U-shaped sling around it just above the external sphincter of anus [4]. The action of this muscle is to draw the ano-rectal junction inwards towards pubis thus contributing to the anorectal angle [4].
During resting the Puborectalis muscle is in contracted state and anal sphincter is closed. Due to sensory perception of stool and rectal distension, the levator ani muscle gets relaxed, rectal muscles contract and external anal sphincter pressure is decreased causing its opening.
Any impairment in the normal functioning of these pelvic muscles lead to dysfunctional defecation. Any neuromuscular injury to the levator muscle leads to eventual sagging of the plate causing increased strain on the pelvic ligaments and fascia which are a support to these organs in pelvis, causing increased risk of organ prolapse [4].
A mid-sagittal section through pelvis is used to best study the anatomical details and mark the parameters to be studied. In females, the pelvis is divided into anterior, middle and posterior compartments comprising of Urinary bladder with urethra, uterus with cervix and vagina and rectum with anus respectively while in males they are divided into anterior and posterior compartments with corresponding organs in them. Following reference lines and angles are studies on the MR images [5].
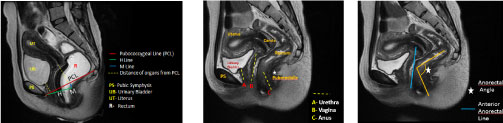 Figure 1: T2 weighted mid sagittal sections through pelvis showing MR anatomy and reference lines and angles. View Figure 1
Figure 1: T2 weighted mid sagittal sections through pelvis showing MR anatomy and reference lines and angles. View Figure 1
A line drawn from inferior border of pubic symphysis to the first sacro-coccygeal joint. It is a reference line drawn to assess the level of pelvic organs. Perpendicular distance between the inferior-most part of the corresponding organ and PCL is measured during rest and while full pelvic straining [5].
Drawn from the inferior border of the pubic symphysis to the posterior wall of the rectum, marks the AP distance of the levator hiatus. Normal < 5 cm [5].
Perpendicular line drawn most posterior aspect of the H line till PCL, suggests ano-rectal descent at rest, if increased. Normal < 2 cm [5].
Angle between the posterior border of the distal rectum and central axis of the anal canal. Normal range: 108°-127° at rest [5].
As per literature, it is drawn along the expected margin of normal anorectal wall behind the posterior wall of vagina. Depth of wall protrusion beyond it during resting and straining is used to assess Rectocoeles.
On defecation, there is mild descent of the pelvic floor and relaxation of the Puborectalis muscle. Following are the points considered on MR for normal defecation.
1. Anorectal angle becomes narrower during squeezing and widens during defecation by about 10°-20° from resting phase [5].
2. All pelvic organs lie above the pubo-coccygeal line during rest and straining and no descent is seen.
3. H line and M line remain within their normal limits.
4. No protrusion of anterior wall of rectum beyond expected margin of anterior rectal line.
Following were the various pathologies encountered:
There was hypertrophied Puborectalis muscle seen causing persistent prominent indentation over the anorectal junction leading to paradoxically narrowed anorectal angle. The patient was not able to defecate the jelly at all and thus there was significant retention of contrast post evacuation. Rest of the parameters within normal limits.
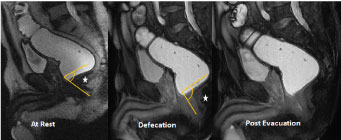 Figure 2: Spastic Perineum Syndrome- Narrow Anorectal angle at defecation and rest. Hypertrophied Puborectalis muscle and post evacuation retention of contents. View Figure 2
Figure 2: Spastic Perineum Syndrome- Narrow Anorectal angle at defecation and rest. Hypertrophied Puborectalis muscle and post evacuation retention of contents. View Figure 2
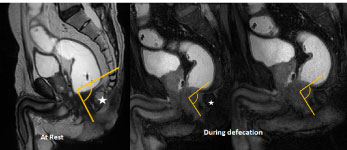 Figure 3: Another case of Spastic Perineum Syndrome- Narrow Anorectal angle at defecation and rest. Hypertrophied Puborectalis muscle and post evacuation retention of contents. View Figure 3
Figure 3: Another case of Spastic Perineum Syndrome- Narrow Anorectal angle at defecation and rest. Hypertrophied Puborectalis muscle and post evacuation retention of contents. View Figure 3
The normal alignment of rectum, anus and ano-rectal junction not maintained. Abnormal anorectal angles at rest. Patient not able to defecate, with significant retention of contents.
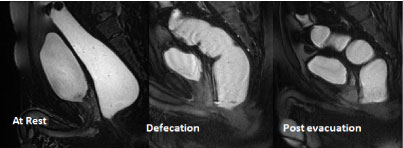 Figure 4: Pelvic Floor Dyssynergia- loss of normal alignment of rectum and anus and retention of contents post evacuation. View Figure 4
Figure 4: Pelvic Floor Dyssynergia- loss of normal alignment of rectum and anus and retention of contents post evacuation. View Figure 4
Increased values of H line and M-line from resting to straining suggesting enlarged levator hiatus. Ano-rectal descent below Pubococcygeal line during defecation. Distance between PCL and organ descent beyond it measured and Graded as Mild: 3cm or less, Moderate: 3-6 cm, and Severe: > 6 cm [5].
 Figure 5: Rectal Prolapse- moderate descent of rectum below PCL line. Increase values of H and M line. View Figure 5
Figure 5: Rectal Prolapse- moderate descent of rectum below PCL line. Increase values of H and M line. View Figure 5
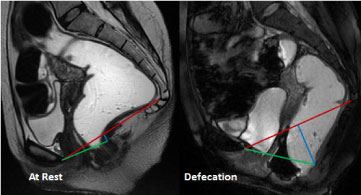 Figure 6: Another case of Rectal Prolapse- moderate descent of rectum below PCL line. Increase values of H and M line. View Figure 6
Figure 6: Another case of Rectal Prolapse- moderate descent of rectum below PCL line. Increase values of H and M line. View Figure 6
Bulging of anterior wall of rectum through posterior vaginal wall beyond the expected margin of Anterior rectal line. Post defecation retention of contents. Depth of protrusion measured and Graded as mild (< 2 cm), moderate (2-4 cm) and large (> 4 cm) [5].
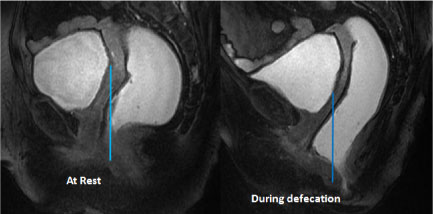 Figure 7: Rectocoele- Moderate bulge of rectum beyond anterior rectal line. View Figure 7
Figure 7: Rectocoele- Moderate bulge of rectum beyond anterior rectal line. View Figure 7
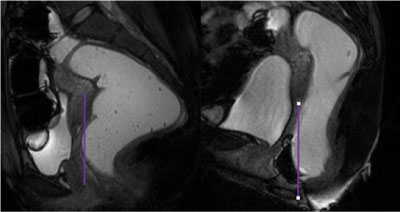 Figure 8: Another case of Rectocoele- Moderate bulge of rectum beyond anterior rectal line. View Figure 8
Figure 8: Another case of Rectocoele- Moderate bulge of rectum beyond anterior rectal line. View Figure 8
Descent of Uterus below PCL at rest or during straining is measured and graded as Mild: > 3 cm, Moderate: 3-6 cm, Severe: > 6 cm. Concurrent Rectal and/or bladder prolapse may be seen.
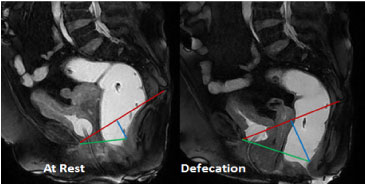 Figure 9: Uterine Prolapse with Cystocoele and Rectal prolapse- Descent of Rectum below PCL at rest. Descent of Urinary bladder, Uterus and rectum on defecation. View Figure 9
Figure 9: Uterine Prolapse with Cystocoele and Rectal prolapse- Descent of Rectum below PCL at rest. Descent of Urinary bladder, Uterus and rectum on defecation. View Figure 9
Stretching of H and M lines as urinary bladder occupies hiatus and displaces uterus and rectum posteriorly and inferiorly [5]. Descent of Urinary bladder > 1 cm below PCL at rest or during straining is considered as cystocoele and graded as Mild: > 3 cm, Moderate: 3-6 cm, Severe: > 6 cm.
Patients in age group 20-85 years were studied. Maximum patient were of the age group 30-40 years (Figure 10). Out of total patients studied 12 were male and 09 were females (Figure 11 and Figure 12). The most common complaint encountered was that of sense of incomplete defecation, followed by chronic constipation and difficulty defecation pelvic pain and fecal and urinary incontinence (Figure 13). Out of 21 patients, 6 were found to be normal and 15 had some or the other pelvic floor pathology (Figure 14). 4 were diagnosed to have Spastic perineum syndrome, 4 had Pelvic floor dyssynergia and 7 had Organ Prolapse. Out of that, 2 had anterior or middle compartment prolapse comprising 1 Cystocoele and 1 Uterine prolapse, while 5 had posterior compartment prolapse i.e. 3 Rectal prolapse and 2 Rectocoele. There were no cases of urethrocoele, urethral hypermobility, descending perineum syndrome, rectal intussusception, perineocoele or enterocoele found in our study.
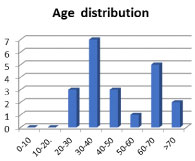 Figure 10: Chart showing Age Distribution of patients. View Figure 10
Figure 10: Chart showing Age Distribution of patients. View Figure 10
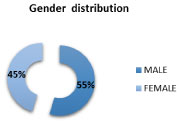 Figure 11: Chart showing Gender Distribution of patients. View Figure 11
Figure 11: Chart showing Gender Distribution of patients. View Figure 11
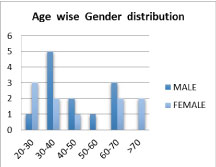 Figure 12: Chart showing Age wise Gender Distribution of patients. View Figure 12
Figure 12: Chart showing Age wise Gender Distribution of patients. View Figure 12
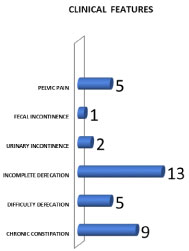 Figure 13: Chart showing distribution of Clinical Features. View Figure 13
Figure 13: Chart showing distribution of Clinical Features. View Figure 13
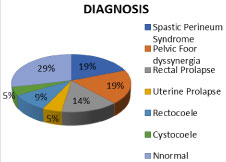 Figure 14: Chart showing Distribution of various Pathologies diagnosed. View Figure 14
Figure 14: Chart showing Distribution of various Pathologies diagnosed. View Figure 14
Pelvic floor pathologies can be broadly divided into two categories- Relaxing and non-relaxing types. Relaxing types involve pelvic floor muscle weakness and thus includes all the organ prolapse cases. Non relaxing type involves pelvic floor's impaired action during defecation process leading to its inability to sustain defecation and thus comprises spastic perineum syndrome, pelvic floor dyssynergia etc.
MR Defecography is successfully able to diagnose these disorders. As per our observations, The non-relaxing types were found to be more common in middle age group i.e. 30-50 years, while the relaxing type of disorders i.e. organ prolapse were more common in either younger age group i.e. 20-30 years owing to childbirth or elderly age group i.e. 60-70 years and beyond owing to old age (Figure 15). Non-relaxing types were found to be more common in males while Organ prolapse were more common in females (Figure 16).
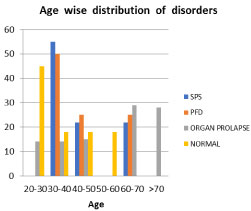 Figure 15: Chart showing Age wise Distribution of disorders. View Figure 15
Figure 15: Chart showing Age wise Distribution of disorders. View Figure 15
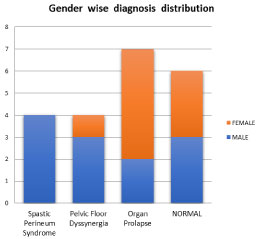 Figure 16: Chart showing Gender wise Distribution of pathologies. View Figure 16
Figure 16: Chart showing Gender wise Distribution of pathologies. View Figure 16
Clinical evaluation of these disorders is done by physical examination including Valsalva maneuver in lithotomy position, which may provide preliminary information in cases of organ prolapse, however it remains inadequate as the total number of compartments affected may often be underdiagnosed [2]. Also, assessment of evacuation disorders is only inadequately done by performing clinical maneuvers. It is only during defecation that the levator ani muscle is maximally relaxed, providing maximal stress to the pelvic floor, thereby revealing the underlying defecation dysfunction or organ prolapse precisely [2].
In the past Fluoroscopic Defecography has been the diagnostic modality to assess these disorders which was first introduced in 1952 however it had its inherent limitations like lower sensitivity, inability to visualize anterior and middle compartments, other pelvic soft tissue or any concomitant pelvic pathology besides radiation exposure [1].
Yang, et al. and Kruyt, et al. introduced MR imaging of pelvic floor in 1991 [2]. Endoanal Ultrasound and Endoanal MRI have also been introduced, all of which image the pelvis- its anatomy and pathologies in exquisite details but the pelvic floor function cannot be assessed in these static imaging techniques.
The limitation of this technique is the patient compliance as it involves performing various maneuvers and hence patience compliance and cooperation is a must for proper acquisition of images. Also, defecating in non-physiological i.e. a supine position can be difficult for the patient. It was thought that this position may also vary the results of defecation action during scanning from the actual but it has been studied that no substantial difference in imaging in supine or sitting positions exists [6]. However with the advent of open MRI, MR defecography technique in sitting position is replacing this conventional supine technique because of better compliance and ease of the patient [7].
For rectal opacification ultrasound jelly was used in our study since it is the most conveniently available product, however mashed potatoes with gadopentetate dimeglumine can also be used [7].
Dynamic MR Pelvic imaging has come up over the last decade and MR Defecography is one of its kind. It is a novel and an emerging modality which, in addition to providing a multiplanar detailed MR imaging of the pelvis with good temporal resolution and high soft-tissue contrast, also allows visualization of the pelvic floor function in real-time without any radiation load. Imaging the defecation process in real-time leads to a definitive diagnosis in cases of dysfunctional defecation and a precise diagnostic and pre-operative assessment in cases of organ prolapse. The variety of disorders of pelvic floor that can be diagnosed on an MR Defecography range from Non relaxing type like Spastic Perineum Syndrome, Pelvic floor dyssynergia to the relaxing types i.e. Uterine Prolapse, Rectal Prolapse, Rectocoele etc. amongst others. All these benefits together make MR Defecography a preferred imaging modality and a good knowledge of the technique and its interpretation is desirable in the advancing era.
Mr. Anwar Gulab Pathan (MRI Technologist). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
None.
Sources of support- None.
Statement of equal authors' contribution- None.