Follicular mucinosis (FM) is a rare cutaneous disease with unclear etiology; it was firstly described by Pinkus, et al. in 1957, who named it mucinous alopecia, referring to a characteristic process of the FM, which leads to alopecia. As this process was not seen on all developments of the disease, in 1959 Jablonska, et al. proposed to name it Follicular mucinosis. Follicular mucinosis is uncommon in children. Using the online searching databases Scielo and PubMed, during the past 10 years, only 16 pediatric case reports about the disease were found: 3 associated with mycosis fungoides (MF), 1 about the acneiform presentation of the disease, 9 discussing the primary type, 1 did not specify the diagnosis in the report and 2 were about other presentations of the disease. The main concern of diagnosing a child with FM is whether it is associated with MF, a cutaneous T-cell lymphoma, that although rare in children, when present is mostly associated with FM. The earlier the diagnosis of MF is made, the better is the prognosis of the patient. Therefore, it is of great importance that a general practitioner pediatrician can diagnose a case of FM and identify whether it is associated with MF or other systemic diseases.
FM: Follicular Mucinosis; MF: Mycosis Fungoides; LSC: Lichen Simplex Chronicus
Follicular mucinosis (FM) is a rare cutaneous disease with unclear etiology [1]. FM can occur as a primary "idiopathic" disorder or associated to various benign or malignant diseases, such as mycosis fungoides (MF) or lupus erythematosus [2]. The clinical presentation is variable, and the main findings include the presence of well-delimited plaques or papules that are erythematous or brownish-erythematous, and erupt acutely or sub acutely, mostly on the head or neck [2]. Less usual manifestations include lesions similar to scarring alopecia, alopecia areata, cysts, nodules, eczema and chronic acneiform eruptions [3]. FM is characterized histopathologically by the deposition of mucin in the sebaceous glands and the follicular epithelium. Because of its unclear etiology, the histopathological exam is necessary to confirm diagnosis.
Using the online searching databases Scielo and PubMed, during the past 10 years, only 16 pediatric case reports about the disease were found: 3 associated with mycosis fungoides (MFg), 1 about the acneiform presentation of the disease, 9 discussing the primary type, 1 did not specify the diagnosis in the report and 2 were about other presentations of the disease. Among the published reports, FM lesions have been reported to mimic lichen spinulosus (Figure 1) and keratosis pilaris (Figure 2), both of which are the main entities in the differential diagnosis of children with suspicious lesions. The lesions generally have a good prognosis and resolve spontaneously, especially in young children [1-6], although some of the presentations can be secondary to cutaneous T-cell Lymphomas, requiring more intensive treatment and long-term clinical evaluation [2-5,7-12].
 Figure 1: Lichen spinulosus: Grouped white papules forming a plaque, in the thoracic region. View Figure 1
Figure 1: Lichen spinulosus: Grouped white papules forming a plaque, in the thoracic region. View Figure 1
 Figure 2: Keratosis pilaris: Skin-colored papules with an erythematous base in the extensor region of the upper limb. View Figure 2
Figure 2: Keratosis pilaris: Skin-colored papules with an erythematous base in the extensor region of the upper limb. View Figure 2
A 5-year-old boy presented with a one-year history of erythematous papules, distributed linearly along 5 cm on the posterior part of his left leg (Figure 3a). He complained about pruritus and the lesion was excoriated. He had previously been treated, in another medical service, for impetigo and larva migrans cutanea, using topic antibiotics and antifungals, with no response to the treatments.
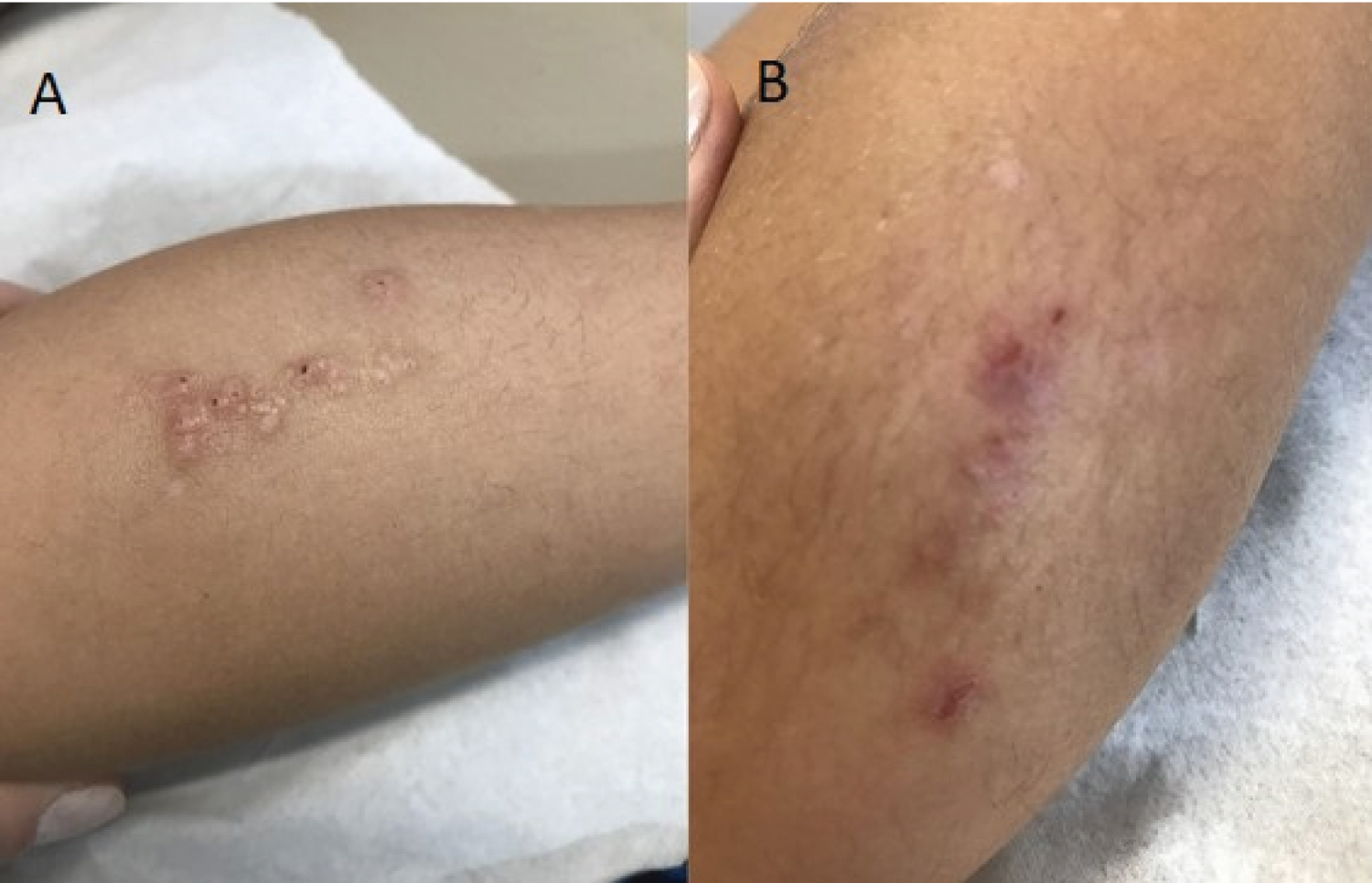 Figure 3: Skin lesions during the first consult (a) and at the moment of the biopsy after four months (b). View Figure 3
Figure 3: Skin lesions during the first consult (a) and at the moment of the biopsy after four months (b). View Figure 3
The first clinical hypothesis in our service was Lichen simplex chronicus (LSC) since the clinical presentation remained the same and there was no response to the previous treatments. Therefore, the next line of treatment was the use of topical occlusive corticosteroids for 30 days, with reduction of the skin lesions and pruritus.
Table 1: Profile of the patients according to the type of osteogenesis imperfecta (values in mean and standard deviation). View Table 1
Table 2: Peds QL 4.0 scores according to the type of osteogenesis imperfecta (values in meansand standard deviation). View Table 2
Four months after the end of the treatment, the lesions returned, with the same clinical presentation and accompanied by pruritus (Figure 3b). The lesion was biopsied and, after histological evaluation (Figure 4), diagnosed as follicular mucinosis. Among the classical findings of the disease, there was also syringometaplasia and lymphoid infiltration, conditions that can be caused primarily by the FM or secondarily to the history of previously treated Impetigo.
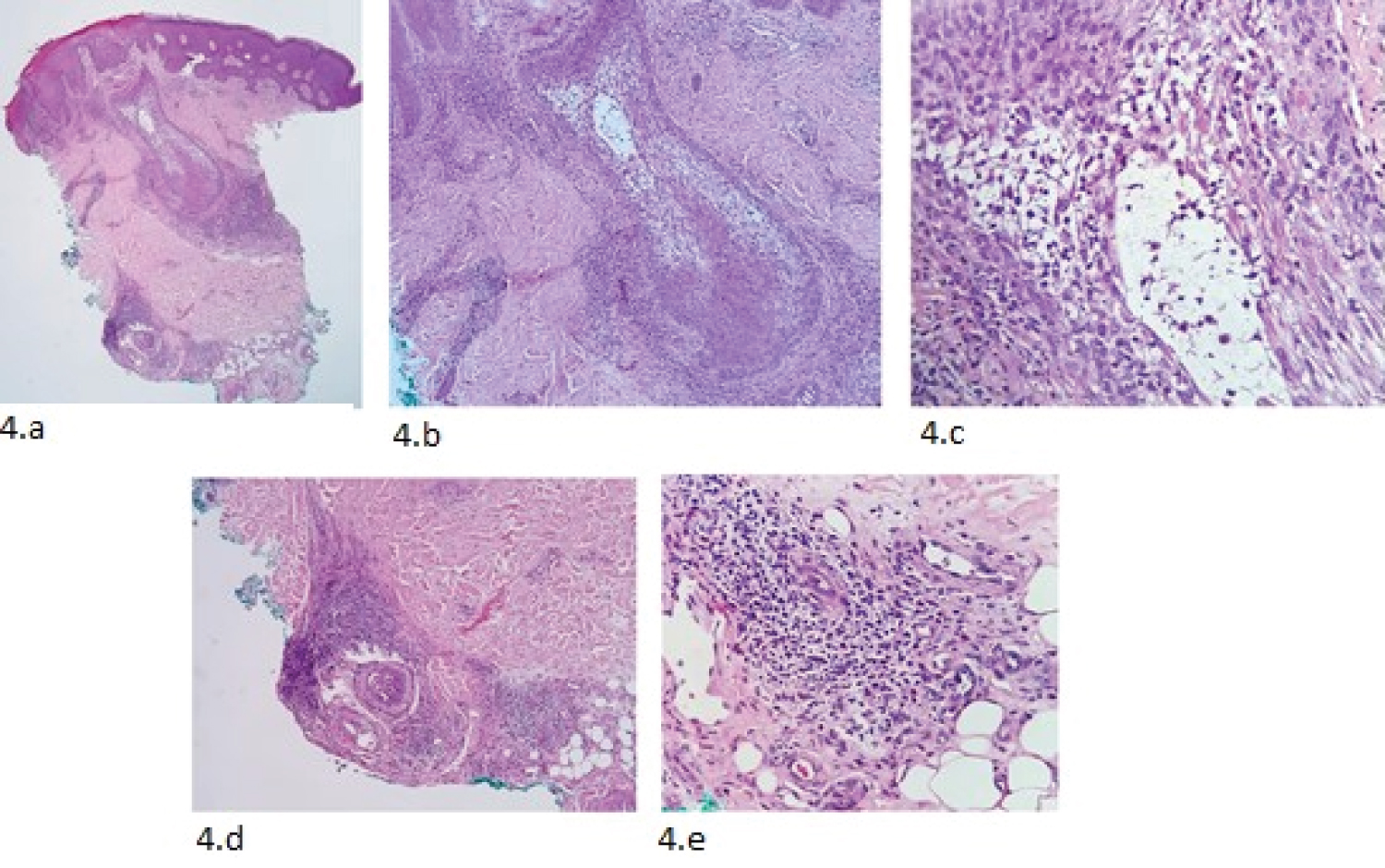 Figure 4: Histological evaluation of the biopsied tissue (hematoxylin-eosin). (a,b) Central hair follicle with intracellular mucin; (c) High-power image showing perifollicular lymphocytic infiltrate and keratinocyte separation; (d,e) Infiltrate surrounding vasculonervous plexus and eccrine gland, with area of syringometaplasia. View Figure 4
Figure 4: Histological evaluation of the biopsied tissue (hematoxylin-eosin). (a,b) Central hair follicle with intracellular mucin; (c) High-power image showing perifollicular lymphocytic infiltrate and keratinocyte separation; (d,e) Infiltrate surrounding vasculonervous plexus and eccrine gland, with area of syringometaplasia. View Figure 4
The first line of treatment was a calcineurin inhibitor for 60 days, with no clinical response. After that, the treatment with topical occlusive corticosteroids was restarted for 60 days, with good response to the treatment and no relapses until now. Despite that, it is not possible to ascertain whether the case was idiopathic or secondary to the impetigo case reported by the previous medical service. Considering the age and clinical presentation of the patient, he is unlikely to have any malignant diseases associated with the FM, such as mycosis fungoides, for example, but the family was oriented to return to the medical service for further tests in case of a new relapse.
FM was described for the first time in 1957 by Pinkus, et al. using the term alopecia mucinosa [1,5,8-10,13], which was further modified to Follicular Mucinosis by Jablonska, et al. in 1959 [1,5,8,13]. The etiology of the disease remains unclear, although four main clinical manifestations have been described, three of them by Coskey and Mehregan in 1970 [10].
The first type of FM is known as benign follicular mucinosis, has a primary and short evolution and usually affects children and young adults. The second type is known as lymphoma-associated FM and is also primary, comprising conditions such as MF, but affects mostly older adults. The third type of FM is secondary, runs with systemic malignancies and usually affects elderly patients. At last, the fourth type of FM is known as Reactive Follicular Mucinosis and refers to the histopathological findings that describe FM but are found in a variety of neoplasms and dermatosis [10].
FM is rare in children [8] and the main differential diagnoses are with lichen spinulosus and keratosis pilaris. Diagnosis of FM can be confirmed only after histologic evaluation of a biopsy of the skin, in which is evident the accumulation of mucin in the follicular infundibulum and adjacent sebaceous gland, with dissolution of cellular attachments; variable degrees of perifollicular inflammation are also observed, with a predominance of lymphocytes and eosinophils. Rarely, syringometaplasiamay also be present, as was the case in our patient. In cases of FM associated with cutaneous lymphoma, more pronounced folliculotropism may be observed, with or without associated epidermotropism and cellular atypia.
A standardized line of treatment has not yet been established, but the treatments can include antimalarials, topical or systemic corticosteroids, among other approaches [8]. The treatment used in this case was a medium capacity topic occlusive corticosteroid. This choice was made based on good reviews about this line of treatment in the literature, along with its easy access and low cost when compared to other available approaches.
The patient reported in this case had a good response to the treatment; despite that, long-term clinical evaluations with biopsy specimens of the remaining lesions are important to confirm that his FM is not associated with mycosis fungoides. MF is a cutaneous T-cell lymphoma and, as happens with FM, there is no standardized treatment for pediatric cases of MF. Some clinical presentations of the disease usually indicate a good prognosis, such as single lesions, located on the head or neck, and those diagnosed still during childhood.
It is important to draw attention to the fact that, although rare in a juvenile age, MF requires diagnosis as early as possible in order to ensure a good prognosis. Because of this situation, it is crucial that pediatricians can evaluate and diagnose lesions of FM, in order to evaluate if it is a primary idiopathic manifestation, if it's associated with MF, or if it's secondary to other diseases, such as Lupus erythematosus, for example. In these secondary cases, the treatment must be directed to the baseline condition that caused the FM. Also, more studies are needed about the relationship between Follicular mucinosis and Mycosis fungoides. Since the pathophysiology of the association is still unknown, the patients need serial medical evaluations until complete resolution of the lesions, which is onerous for the Health system and for the family's quality of life.
The early diagnosis of Follicular mucinosis is important because, despite being rare, the disease might have a bad prognosis when associated with Mycosis fungoides or other diseases. Therefore, medical intervention in such cases is especially relevant to improve the prognosis of the patients.
Furthermore, even the idiopathic forms of Follicular mucinosis cause a burden to the patient and the family, either by the constant pruritus, or the repeated non resolutive diagnosis, since the disease is rare. These situations can cause a series of wrongful diagnosis and consequent diminished quality of life.
No funding was secured for this study.
The authors have no financial relationships relevant to this article to disclose.
The authors have no conflicts of interest to disclose.
The present study highlights the importance of diagnosing Follicular mucinosis as a general practitioner, and how it impacts the patients prognosis.
Maria Luiza Cimardi Rupp designed the study, analyzed data, wrote the original manuscript, made the literature review and revised the manuscript; Marice El Achkar Mello designed the study, collected data and made the initial data analysis and reviewed and corrected the manuscript; Maria Marlene de Souza Pires designed the study, coordinated and supervised the data collection and reviewed and corrected the manuscript; Amanda Amaro Pereira analyzed data and reviewed and corrected the manuscript.
All authors approved the final manuscript as submitted and agreed to be responsible for all aspects of the document.