The aim of the present review was to analyze the literature and describe the clinical and radiographic features of HD-SOD. In addition, an unusual new case which was thought to be a subtle type of HD-SOD, involving a girl, was presented with detailed characteristics of HD-SOD. All HD-SOD cases published between 1987 and 2020, along with the present case, making a total of 66 cases, were evaluated according to criteria which included gender, age, and location of the lesion, clinical and radiological findings. Some of the previously reported cases lacked information regarding various criteria.
We have found that the lesion was discovered mainly in the 1st decade of life, and has a significant male predilection with a female-to-male ratio of 1:1.9. In all cases except one, the alveolar process of the maxilla was affected unilaterally, with gingival and bone enlargement and facial asymmetry being constant findings. Missing maxillary permanent premolars and skin manifestations such as; hypertrichosis and nevus are also common symptoms. Bone pattern was generally termed as vertically oriented, sclerotic, ill-defined, dense and granular radiopacity. Early recognition of HD/SOD also requires appropriate referrals to colleagues and interdisciplinary team approach, thus patients with HD/SOD can gain access to specialist dental care, including orthodontics, prosthodontics, and oral surgery.
Segmental odontomaxillary dysplasia, Hemimaxillofacial dysplasia, Diagnosis
• HD-SOD is detected at birth or childhood and characterized by unilateral enlargement of the alveolar process of maxilla in association with gingiva and teeth.
• We presented a unique mild case along with expansive literature review.
• New cases should include clinical, radiographic, histologic findings, follow-up reports and treatment protocols.
Miles, et al. [1] in 1987 were the first to mention Hemimaxillofacial dysplasia (segmental odontomaxillary dysplasia) (HD-SOD) in a report of two cases. Since then, several authors have made noteworthy contributions to our knowledge concerning the disorder. It is a rare developmental and non-progressive abnormality of unknown etiology first recognized almost 30 years ago, and relevant data is incomplete. It is detected at birth or childhood and characterized by unilateral enlargement of the alveolar process of maxilla in association with gingiva and teeth. Radiographic appearance of the affected bone is sclerotic and often vertically oriented. Missing permanent premolars, tooth abnormalities, delayed eruption and displayed teeth are common findings. There are accompanying manifestations, such as; facial asymmetry, hypertrichosis, nevus, erythema and hypopigmentation in the skin. Immature woven bone with irregular patterns and gingival hyperplasia are histologically common findings. Differential diagnosis includes hemifacial hyperplasia, monostatic fibrous dysplasia, and regional odontodysplasia [1-31].
An 11-year-old girl with the chief complaint of ineffective chewing of food as a result of anterior open bite was referred to Ankara University, Department of Orthodontics in Turkey (Figure 1). Patient was asymptomatic and her medical history was non-contributory. An informed consent was received from the patient's family. The patient presented with a skeletal Cl I malocclusion. The intra-oral examination revealed that there was anterior open bite and tongue thrust (Figure 1c). Extra-orally, mild facial asymmetry and dropping of the inferior border of upper right eye were observed. Hypertrichosis and several nevi from light to dark brown were evident on right cheek (Figure 2a and Figure 2b). Intraoral examination showed that there was a deciduous carious tooth and missing 2nd premolar. Radiological examination showed that there was a deciduous carious tooth and missing 2nd premolar involving the right posterior maxilla along with irregular trabeculation of the bone. Panoramic and intraoral radiography taken at the time of examination showed that the affected maxillary posterior bone showed altered, irregular and vertically oriented trabeculae. Hypodontia of the permanent maxillary right second premolar along with resorbed and carious deciduous molars were also detected (Figure 3a and Figure 3b). Axial CBCT scans indicated slightly enlarged right maxillary posterior alveolar ridge with irregular bone when compared to left side alveolar ridge (Figure 3c). Fluid retention in maxillary sinus along with nasal airway obstruction was easily detected (Figure 3d).
 Figure 1: (a,b) Extraoral images before and after orthodontic treatment; (c,d) Intraoral images before and after orthodontic treatment. View Figure 1
Figure 1: (a,b) Extraoral images before and after orthodontic treatment; (c,d) Intraoral images before and after orthodontic treatment. View Figure 1
 Figure 2: (a) Extraoral image illustrating mild facial asymmetry and dropping of the inferior border of upper right eye; (b) Hypertrichosis and several nevi from light to dark brown were evident on right cheek. View Figure 2
Figure 2: (a) Extraoral image illustrating mild facial asymmetry and dropping of the inferior border of upper right eye; (b) Hypertrichosis and several nevi from light to dark brown were evident on right cheek. View Figure 2
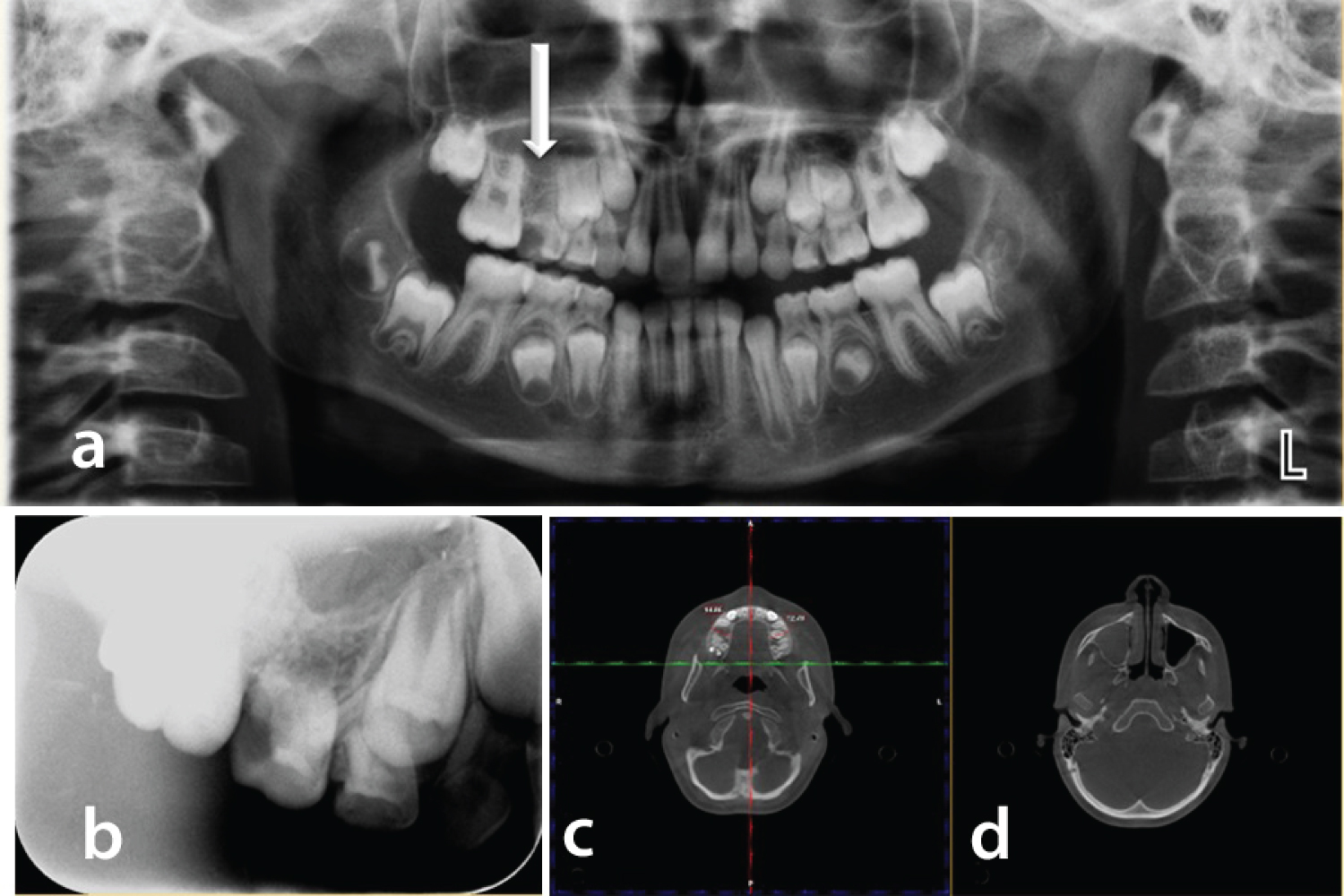 Figure 3: (a,b) Panoramic and periapical radiographic images taken at the time of examination showed that the affected maxillary posterior bone showed altered, irregular and vertically oriented trabeculae. Periapical radiographic image showed hypodontia of the permanent maxillary right second premolar along with resorbed and carious deciduous molars; (c) Axial CBCT scans indicated slightly enlarged right maxillary posterior alveolar ridge with irregular bone when compared to left side alveolar ridge; (d) Fluid retention in maxillary sinus along with nasal airway obstruction was easily detected. View Figure 3
Figure 3: (a,b) Panoramic and periapical radiographic images taken at the time of examination showed that the affected maxillary posterior bone showed altered, irregular and vertically oriented trabeculae. Periapical radiographic image showed hypodontia of the permanent maxillary right second premolar along with resorbed and carious deciduous molars; (c) Axial CBCT scans indicated slightly enlarged right maxillary posterior alveolar ridge with irregular bone when compared to left side alveolar ridge; (d) Fluid retention in maxillary sinus along with nasal airway obstruction was easily detected. View Figure 3
Panoramic radiography of the patient taken 1 year after the beginning of the treatment shows the affected region (Figure 4a). Intra-orally, the edentulous right maxillary alveolar process appeared slightly larger than the left 1 month after extraction of deciduous molars (Figure 4b). Biopsy obtained from the patient showed fibrous connective tissue in the interstitial space between osseous trabeculae. Hard tissue demonstrated irregular lamellar trabecular bone. Some trabeculea were seen as round shaped sementoid tissue similar to fibro osseous lesions (Figure 4c, Figure 4d and Figure 4e). Besides, distrophic calcifications in the pulp were also detected (Figure 4f). Regional odontodysplasia, hemifacial hyperplasia, and monostatic fibrous dysplasia were all considered for differential diagnosis. On the basis of the clinical, radiographic and histologic findings, a diagnosis of HD-SOD was made.
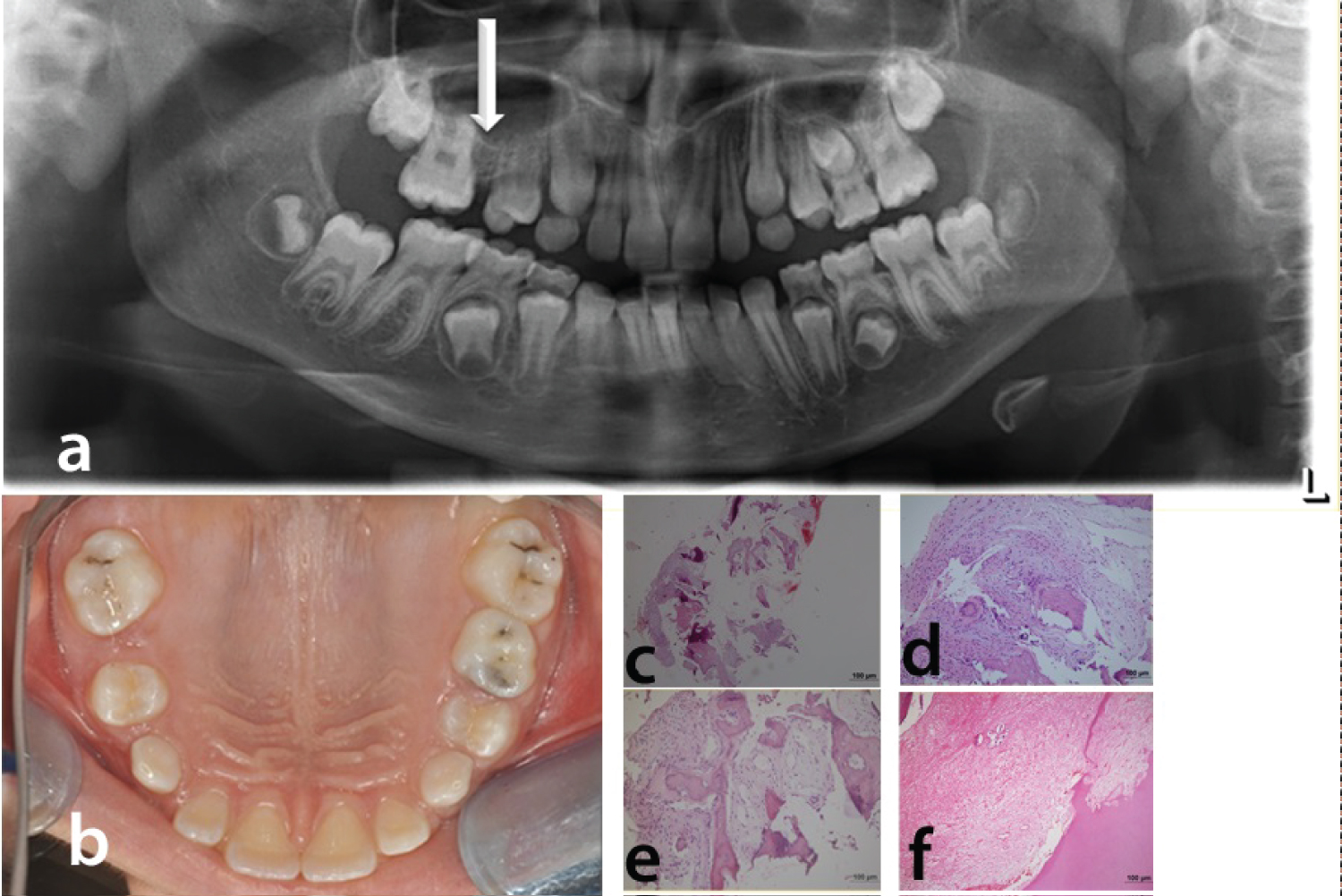 Figure 4: (a) Recent panoramic radiography of the patient taken 1 year after the beginning of the treatment. White arrow shows the affected region; (b) Intraoral photography of the patient; (c) (HE staining x40); (d,e) (HE staining x100): Fibrous connective tissue in the interstitial space between osseous trabeculae. Hard tissue demonstrated irregular lamellar trabecular bone; (f) (HE staining x100): Distrophic calcifications in the pulp tissue. View Figure 4
Figure 4: (a) Recent panoramic radiography of the patient taken 1 year after the beginning of the treatment. White arrow shows the affected region; (b) Intraoral photography of the patient; (c) (HE staining x40); (d,e) (HE staining x100): Fibrous connective tissue in the interstitial space between osseous trabeculae. Hard tissue demonstrated irregular lamellar trabecular bone; (f) (HE staining x100): Distrophic calcifications in the pulp tissue. View Figure 4
Right IV, III, and left III, IV were extracted. An open-bite activator (Functional Orthodontic Therapy) was applied for 12 months and a swallowing exercise was planned simultaneously. Then the appliance was worn at night as a retention appliance for almost 6 months. The open-bite activator had posterior acrylic bite blocks in order to prevent posterior teeth from coming out [14]. The appliance that did not contact the incisal edges of the maxillary and mandibular incisors allowed extrusion of incisors. During 1 year of follow-up, the condition was non-progressive.
A review of the literature was completed by searching PubMed for cases published in English before January 2020. Up until now 65 cases of HD/SOD were reported except for the present case. Clinical and radiographic findings in HD-SOD of 65 cases diagnosed between 1987 and 2020 and the present case is presented in Table 1. Although the etiology is unclear, systemic or endocrine aberration, post-zygotic mutation of bone and skin, and viral or bacterial infection along the branches of the maxillary division of the trigeminal nerve are among the possible causes of the syndrome [1-31]. The clinical and radiological findings accompanying the syndrome represent a large spectrum of variations among individuals. We have found that the lesion is discovered mainly in the 1st decade of life. The maxillary alveolar process enlargement involving the gingiva, the bone, or both in all cases along with facial asymmetry were constant findings. Facial asymmetry was usually mild and not stated in most cases. Since facial asymmetry is non-progressive, recontouring osteotomy is not necessary for most patients. The main objective should be to maintain the primary teeth and to enhance eruption of the permanent molars in order to restore occlusion [1-31]. In the case presented here, an open bite activator was applied after extraction and during 1 year of follow-up, the condition was non-progressive. In case of severe facial asymmetry cases appropriate functional orthopedic or surgical treatment by conducting ortognathic distraction may be applied. In addition, tooth eruption guidance and unilateral expansion may be important tools for the treatment of this disorder. Missing teeth should be replaced by the combined efforts of prosthodontist, surgeon and orthodontist.
Table 1: Clinical and radiographic findings in HD-SOD of 66cases diagnosed between 1987-2020. View Table 1
The age at diagnosis ranged between 2 and 45 years. There were 41 male (63%) and 24 female (37%) patients and an almost equal distribution for right (32 of 62) and left (32 of 62) maxilla. In a unique case of a SOD it was unclear from the radiographic and surgical images assessed whether the patient demonstrated buccolingual bony expansion with radiographic changes but the authors were the first to report SOD along midline. This case was characterized with pre-maxillary enlargement and abnormal pattern of eruption of anterior maxillary permanent teeth [26]. Twenty-five of 65 cases described showed ipsilateral cutaneous changes, including hypertrichosis, hyperpigmentation, hypopigmentation, erythema, lesions, ectopic eyelashes, Becker nevus, cleft lip, facial depression, and commissural lip pit. Distribution of clinical findings in hemimaxillofacial dysplasia/segmental odontomaxillary dysplasia of 65 cases diagnosed between 1987 and 2020 is given in Table 2.
Table 2: Distribution of clinical findings in hemimaxillofacial dysplasia/segmental odontomaxillary dysplasia of 65 cases diagnosed between 1987 and 2020. View Table 2
Radiologically, in most cases the first premolar or both permanent premolars were missing. Delayed eruption, displaced teeth, root resorption, hypoplastic teeth and enlarged pulps were among the most reported dental abnormalities. Bone pattern was generally termed as vertically oriented, sclerotic, ill-defined, dense and granular radiopacity in some cases extending in to the maxillary sinus making it depicted smaller than the opposite side in the radiological images [1-31]. We defined the radiographic appearance as altered, irregular and vertically oriented trabeculae. Our case report was radiologically unique. On axial sections of CBCT, rather than extensive alveolar enlargement mildly enlarged right maxillary posterior alveolar ridge was observed, therefore; this case might be considered as a mild form of the disorder. Rather than taking occlusal radiographs the mediolateral expansion of the alveolar process and extent of the enlargement was accurately determined by CBCT in three dimensions. CBCT imaging also indicated fluid retention in maxillary sinus along with nasal airway obstruction. Sinus involvement was reported in approximately one half of the previous cases. In our case, CBCT examination of the patient provided more accurate data compared to panoramic and periapical radiographs. CBCT imaging of HD cases are encouraged to understand the full extent of the maxillofacial involvement in this disorder [1-31]. Radiological findings in hemimaxillofacial dysplasia/segmental odontomaxillary dysplasia of 65 cases diagnosed between 1987 and 2020 are shown in Table 3.
Table 3: Radiological findings in hemimaxillofacial dysplasia/segmental odontomaxillary dysplasia of 65 cases diagnosed between 1987 and 2020. View Table 3
As unilateral enlargement of the alveolar process was not prominent in the case reported here the diagnosis could not be made without the assessment of skin manifestations. Hypertrichosis and nevi were observed along with the dropping of the right eye and right vermillion border in the presented patient. Hypertrichosis has been previously reported in male patients mostly. In most patients, it is possible that skin lesions were unrecognizable or ignored because of the dento-maxillary involvement. Hypertrichosis, Becker's nevus, nevus, erythema of the cheek, erythematous lesions, lip hypopigmentation, cheek hyperpigmentation, depression of the cheek, cleft of the vermillion border, and lip clefting were among commonly diagnosed skin manifestations. Some patients had different manifestations simultaneously [1-31].
Regional odontodysplasia, hemifacial hyperplasia, and monostatic fibrous dysplasia were all considered for differential diagnosis of HD/SOD. In regional odontodysplasia affected teeth may be unerupted, however; there is no association with alteration of alveolar bone. Hemifacial hyperplasia is not associated with coarse vertically oriented trabeculae. Fibrous dysplasia is not associated with skin manifestations and unerupted teeth [24].
In our notion, the reported cases are insufficient to completely describe HD/SOD. New cases should include clinical, radiographic, histologic findings, follow-up reports and treatment protocols to improve dentist and parent information regarding HD/SOD.
HD/SOD is a rare and unusual condition affecting the maxilla and associated structures. Early recognition of HD/SOD also requires appropriate referrals to specialists and interdisciplinary team approach, thus patients with HD/SOD can gain access to specialist dental care, including orthodontics, prosthodontics, and oral surgery.