Background: Chronic venous insufficiency (CVI) often presents with the development of incompetent short or great saphenous veins (SSV or GSV), resulting in a condition known as varicose veins.
Methods: The present study was conducted with the aim of evaluating the outcomes following endovenous laser therapy (EVLT) for CVI by discharging the patient on the same day following the procedure.
Results: In this study, varicose vein treatment was done in 102 patients with EVLT on a daycare basis. An occlusion of GSV along with its branches was achieved in most of the cases with self-limiting adverse effects and very few recurrence rates in the follow-up period.
Conclusion: Relief of symptoms and a significant improvement in the appearance of varicose veins were noted 4-6 months after initial treatment, and pain was greatly resolved in all the treated limbs. In this study, only 4 patients developed recurrence following varicose vein treatment out of 102 patients with EVLT on a daycare basis.
Chronic Venous Insufficiency (CVI), Varicose Veins, Endovenous Laser Therapy, Recurrence, Day Care Surgery
Chronic venous insufficiency (CVI) is a term used to describe the discomfort brought on by venous hypertension as well as lower extremity edema and skin trophic alterations [1]. Primary chronic venous insufficiency is caused by congenital abnormalities or changes in the biochemistry of the venous wall and describes the clinical presentation without a precipitating event. According to recent research, 30% of patients have secondary disease, and about 70% of patients have basic chronic venous insufficiency [2]. Chronic venous insufficiency-related disability results in diminished quality of life and decreased productivity at work [3]. A frequent ailment known as varicose veins is brought on by weak or damaged vein walls and valves. One-way valves within veins open and close to maintain blood flow toward the heart. Blood can pool and even flow backward in veins that have weak or broken walls or valves. We refer to this as reflux [4].
The natural history and pathogenesis of chronic venous diseases are still unclear, possibly as a result of the disease's complex origination, which makes identifying its causal elements challenging. Varicose veins and skin trophic changes have been linked to the pathophysiology of the venous system from a hemodynamic point of view and the effects of valvular dysfunction in superficial, deep, and perforating veins [4,5]. Untreated CVI typically progresses and causes venous ulcers and post-phlebitis syndrome [5]. The patient might additionally experience pain, swelling in the legs, pruritus, and skin discoloration in addition to the cosmetic damage. Compression stocking use is the cornerstone of treatment; however, compliance rates are low. Most procedures for varicose veins are minimally invasive and do not require a long recovery [6].
In a study conducted by Agarwal, et al. [7] a high prevalence of varicose veins was noted in Indian population, which affect over half of the female population and almost one third of the male population. Vascular symptoms have been observed in 18.9% of the male population and 49.3% of the female population. Skin trophic changes have been observed in 5.2% of males and 18.9% of females, respectively [7]. The pathophysiology of chronic venous insufficiency is triggered by reflux (backward flow) or blockage of venous blood flow [8,9]. The persistent valvular dysfunction of superficial veins, deep veins, or the perforating veins that join them can result in chronic venous insufficiency [10].
Typically, weak or irregularly shaped valves or enlarged venous widths cause superficial incompetence because they prevent normal valve congruence [11]. The most common cause of deep vein dysfunction is a prior DVT, which causes inflammation, valve scarring and adhesion, and luminal constriction [12]. Varicose veins caused by chronic venous disease are treated and managed using endovascular laser ablation [13]. The primary indication for this course of treatment is a disease that fails to respond well to compression stocking-based conservative therapy [14].
The framework for characterizing venous disease, including varicose veins, is provided by the CEAP classification system. For instance, C3S venous disease could be diagnosed in a patient who comes into the medical facility with varicose veins, mild oedema, and pain, but no lower extremity hemosiderin staining. Venous investigations would be required in order to use the remaining CEAP system components to further categorize the patient. While the CEAP categorization system is useful for diagnosis, it is not a recommendation for choosing a course of therapy [13,14].
Conservative care and interventional therapies such endovenous sclerotherapy, thermal ablation, and surgery are available for the treatment of varicose veins. Both the choice of treatment and the decision to continue with it are determined by the patient's preferences and symptoms. Cost, the possibility of problems, the accessibility of resources, insurance payment, and medical education are other factors to be taken into account. Treatment can also be guided by the features of the afflicted veins and the existence or absence of profound venous insufficiency [15].
Consequently, the purpose of this study was to determine the prevalence, risk factors, and analysis of varicose veins, skin trophic changes, as well as the outcomes including recurrence of day care operations in these individuals.
This prospective cohort study was conducted at the Department of Cardiothoracic & Vascular Surgery from November 2016 to October 2018 (2 years). The present study was conducted with the aim of evaluating the outcomes in terms of achievement of occlusion of the GSV and disappearance of the associated varicosities, complications, and recurrence rates following endovenous laser therapy (EVLT) for CVI by discharging the patient on the same day following the procedure, i.e., on a daycare basis.
During this time, a total of 102 patients (after sample size estimation) who presented to the outpatient department and met the inclusion criteria were included in the study. For this study, institutional ethics committee approval was taken from the present institute as well as from the cath lab (IEC/GSVM/LPSIC/Thesis/2016-14/CC-5802).
The study's protocols adhered to the Declaration of Helsinki's 1975 ethical criteria. Every patient gave their proper, written, informed consent. They were treated with EVLA and were followed up every week in the first month post procedure and thereafter on monthly basis till the completion of follow up visits i.e. for one year and during every visit patients were evaluated clinically and were also subjected to ultrasonography Doppler to rule out or check for recurrence following procedure.
The inclusion criteria included patients with age at least 14 years, patients willing to consent (for the patients in the age groups 14-18 years consent was obtained from the parents), patients with saphenofemoral junction reflux or saphenopopliteal junction reflux with great and short saphenous vein reflux, as demonstrated by bidirectional continuous wave doppler and duplex ultrasonography, and patients ready to follow-up for 1 year after the treatment, were included in the study.
Exclusion criteria included patients with suspected deep vein thrombosis (DVT), patients not able to ambulate, patients with poor health who are non-compliant with severe illnesses and comorbidities with non-palpable pedal pulses and females who are pregnant or planning to conceive during the course of treatment and follow-up. Patients were included after meeting the inclusion and exclusion criteria.
Varicosity and incompetent perforators were first marked (using Henna, a dye obtained from the plant species Lawsonia inermis , was used to mark the site of the varicose vein perforators) as described in the methods section. Great Saphenous Vein was punctured ideally below the knee in the Trendelenburg position, as shown in Figure 1.
 Figure 1: (A) A picture showing markings being done for perforators and varicose veins; (B) An intraoperative picture showing perforator ligation being done.
View Figure 1
Figure 1: (A) A picture showing markings being done for perforators and varicose veins; (B) An intraoperative picture showing perforator ligation being done.
View Figure 1
The vein and perforators were inspected in the c-arm after injecting gadollium-based dye measuring around 50 ml into the vein. After sheath and fibre were introduced, tumescent anaesthesia was given in the perivenous plane safely with use of an intraoperative doppler (for making neighbouring tissue firm and tense for pain relief and preventing neighbouring structures from getting burned), and a laser was fired at 80 J and 8 Watts. Energy was reduced to 60 J below the knee, as shown in Figure 2.
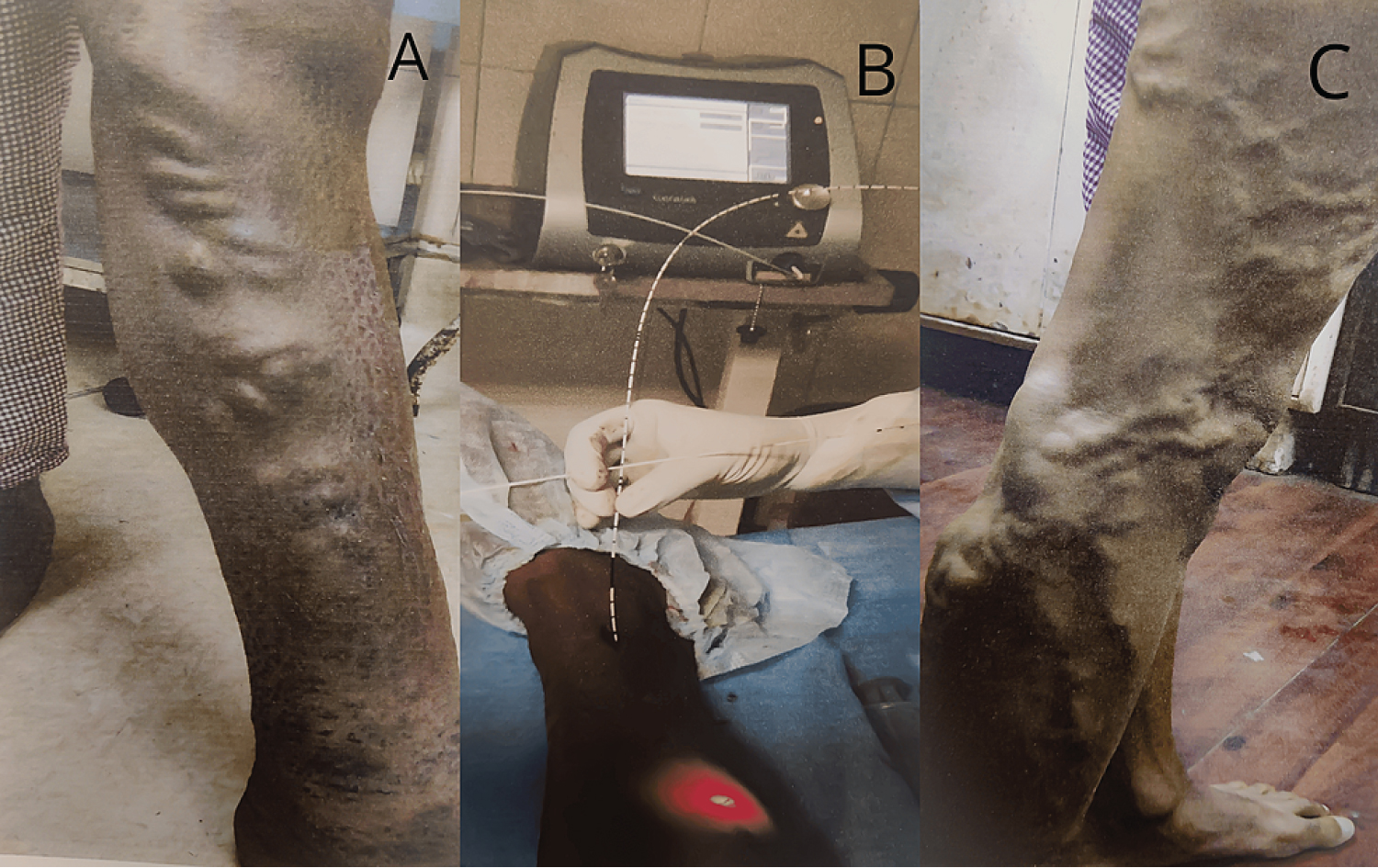 Figure 2: (A) Varicose veins with perforators in the left lower limb; (B) Endovenous laser ablation (EVLA) being done; (C) Varicose veins with perforators in the right lower limb.
View Figure 2
Figure 2: (A) Varicose veins with perforators in the left lower limb; (B) Endovenous laser ablation (EVLA) being done; (C) Varicose veins with perforators in the right lower limb.
View Figure 2
Fibre was withdrawn slowly at the rate of 3 mm. Perforators were ligated and divided, and dressing was done with Crepe bandage followed by compression stocking advised for 2 weeks following the intervention. During follow-up, duplex USG was done at one month, three months, six months, and yearly thereafter to assess treatment efficiency and adverse effects associated with the procedure. Patients with incompetent GSV, SSV, and perforators were treated with the EVLT and the ligation of the perforators. The follow-up period ranged from 30 days to 1 year.
All the patients were preoperatively assessed by colour Doppler and duplex ultrasonography, which was done by an experienced radiologist who was a member of the team prior to the instrumentation, and on subsequent follow-up visits, duplex was performed in an upright position. Reflux was defined as being antegrade and could be triggered by manual compression of the leg. Reflux was defined as a retrograde flow lasting more than 0.5 seconds with patients standing during a valsalva manoeuvre or with compression or decompression of the calf.
The pre- and post-operative diameters of SSV and GSV were measured at 3 cm distally from the Saphenopopliteal junction (SPJ)-SFJ junction. Even a slight marginal flow or reflux with largely closed veins was defined as subcutaneous varicosity of more than 3 mm in diameter in the treatment area, which occurred after initial treatment. The entire venous system was checked for any signs of DVT. Then, only patients were subjected to EVLT, as explained earlier.
All the patients were examined with bidirectional continuous wave doppler examination and duplex ultrasonography to identify sources of venous incompetence and precisely map out abnormal venous pathways.
The patients were followed up every week in the first month post procedure and thereafter on monthly basis till the completion of follow up visits i.e. for 1 year and during every visit patients were evaluated clinically and were also subjected to ultrasonography Doppler to rule out or check for recurrence following procedure.
Our estimated sample size was based on the study of the role of EVLT in the management of CVI by M.A. Sharif, et al. [16]. Thus, a sample size of 102 provided 90% power at a 95% confidence level. A total of 102 patients were included from the outpatient department who met the inclusion criteria and who met the criteria as shown in Table 1.
Table 1: A table showing the inclusion and exclusion criteria for the patients. View Table 1
The total number of 102 patients who presented to outpatient department of Cardiothoracic & Vascular Surgery within the study duration i.e., from November 2016 to October 2018 (2 years) and met the inclusion criteria were admitted and treated by these methods after obtaining the informed consent.
The sampling method used in our study was simple random sampling technique in order to provide accurate representation of the larger group, bias reduction, solid basis for hypothesis testing and to calculate margin of error and confidence intervals. For testing the significance of proportion, we used the Fisher-Z test to declare that the aim or hypothesis is significant or not at p < 0.05 (significant) or p > 0.05 (non-significant) at different degrees of freedom and the tabulated value of Z.
In our study, a total of 102 patients have undergone treatment for varicose veins. The maximum number of patients (34.3%) were found in the 41-50 year-old age group, followed by the 18-30 year-old age group, i.e., 32.3%, and the male prevalence was 82.4% higher when compared to the female prevalence (p = 0.021), i.e., 17.6%. Most of the patients presented with complaints of dilated veins (88.0%) (p = 0.032), followed by pain (41.0%). The demographic profile and disease characteristics of the patients have been shown in Table 2.
Table 2: A table showing the demographic profile and disease characteristics of the patients included in the present study. View Table 2
In our study, there was male preponderance and the most prevalent risk factor contributing to this condition was prolonged standing at 74.5% (p = 0.043), followed by obesity, i.e., 24.5% observed during the clinical assessment.
The majority of the patients had combined segment involvement of 60.7% (p = 0.046), followed by GSV involvement of 29.4% as shown in Table 3.
Table 3: A table showing the limb involvement etiology, anatomical variation and pathology leading to varicose veins. View Table 3
As per the above-mentioned table, the left limb was most frequently involved (46.0%) (p = 0.029), followed by bilateral lower limb involvement (34.3%), and all the patients had primary aetiology and superficial vein involvement pertaining to chronic venous insufficiency in our study.
The pathology associated with the disease was reflux in 76.4% (p = 0.016) and arteriovenous fistula/venous malformation in 23.5% of cases. As per the below-mentioned chart, most of the patients fell into clinical class II (varicose veins) (P ≤ 0.016), followed by clinical class IV (skin changes with varicose veins) (p = 0.019), as shown in Figure 3.
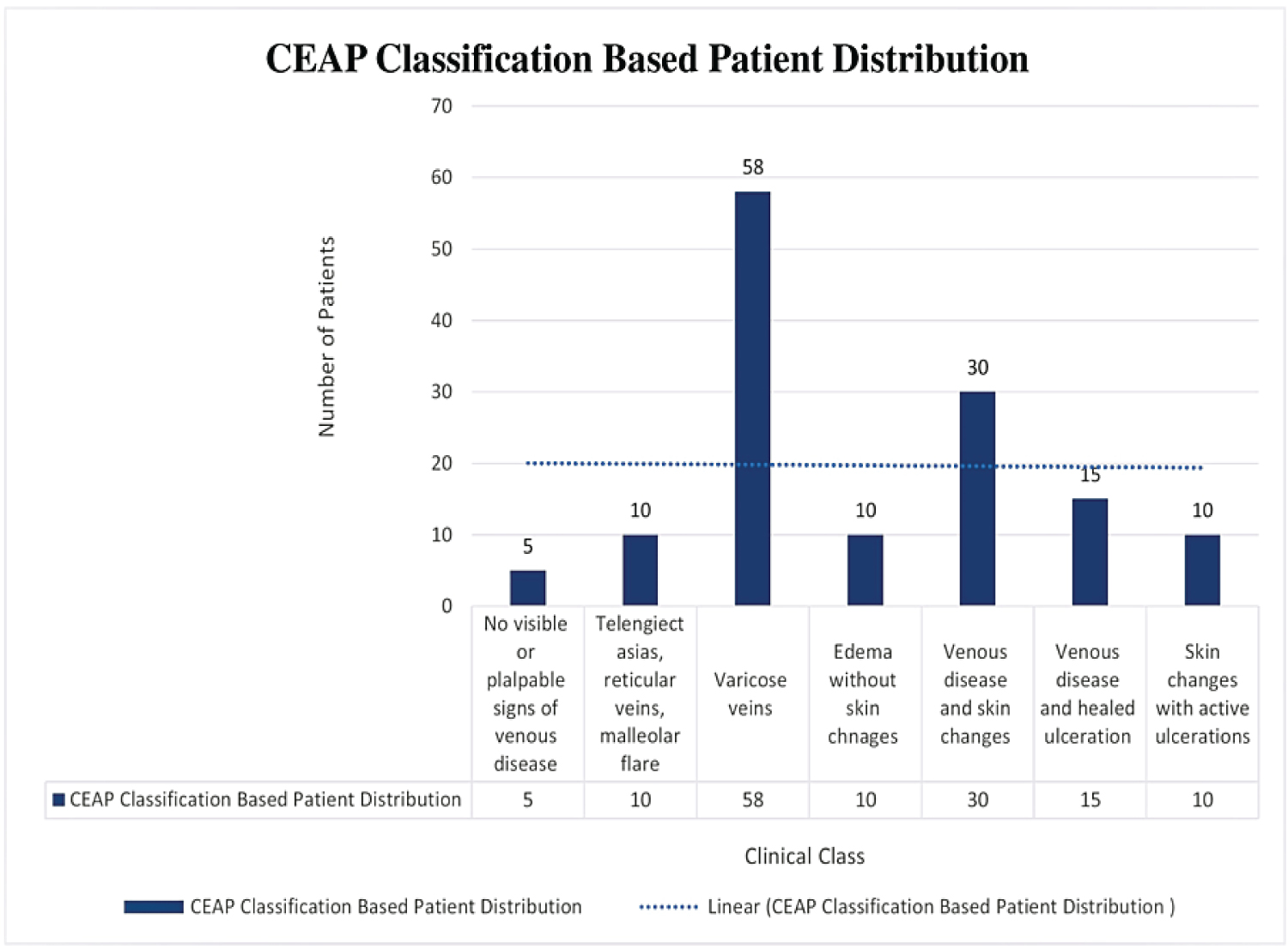 Figure 3: A figure showing Clinical (C), Etiological (E), Anatomical (A), and Pathophysiological (P) CEAP classification-based patient distribution in our study.
View Figure 3
Figure 3: A figure showing Clinical (C), Etiological (E), Anatomical (A), and Pathophysiological (P) CEAP classification-based patient distribution in our study.
View Figure 3
The endolaser was used to treat primary superficial varicosity in 102 patients with age ranging from 18-70 years (mean 44 years). Of all patients, 82.4% were male and 17.6% were females. Out of 102 patients, 30 (29.4%) cases were of primary GSV insufficiency (p = 0.047), 5 (4.9%) limbs had primary SSV incompetence, associated venous incompetence (including perforators) were observed in 5 (4.9%), rest 62 (60.7%) limbs showed combined pathology.
The GSV diameter range between 5-21.4 mm (mean 1.31 cm) (p = 0.022) measured 3 cm below the SFJ whereas the SSV diameter ranged between 6-9 mm (mean 7 mm) measured 3 cm below popliteal crease. Total length of GSV treated range from 55-70 cm (mean 61 cm) and that of SSV was 15-22 cm (mean 18 cm). In 35 (34.3%) subjects the involvement was bilateral in the rest 67 (65.7%) (p = 0.028) of the subjects, it was unilateral. Overall we treated 47 (46%) left limbs and 20 (19.7%) right limbs.
We used an average linear endovenous energy density (LEED) for GSV of 72.2 J/cm vein with a minimum of 60 J/cm (50 to 80 J/cm). The dilated tributaries of GSV and SSV were also ablated with laser using multiple punctures.
In our study, the most common complication was pain and tightness in the lower limbs in 30 patients (29.4%) (p = 0.039), paraesthesia in 20 patients (19.6%), skin burn in 10 patients (9.8%), and infections in 2 patients (1.9%) after undergoing EVLT at our centre, as shown in Figure 4.
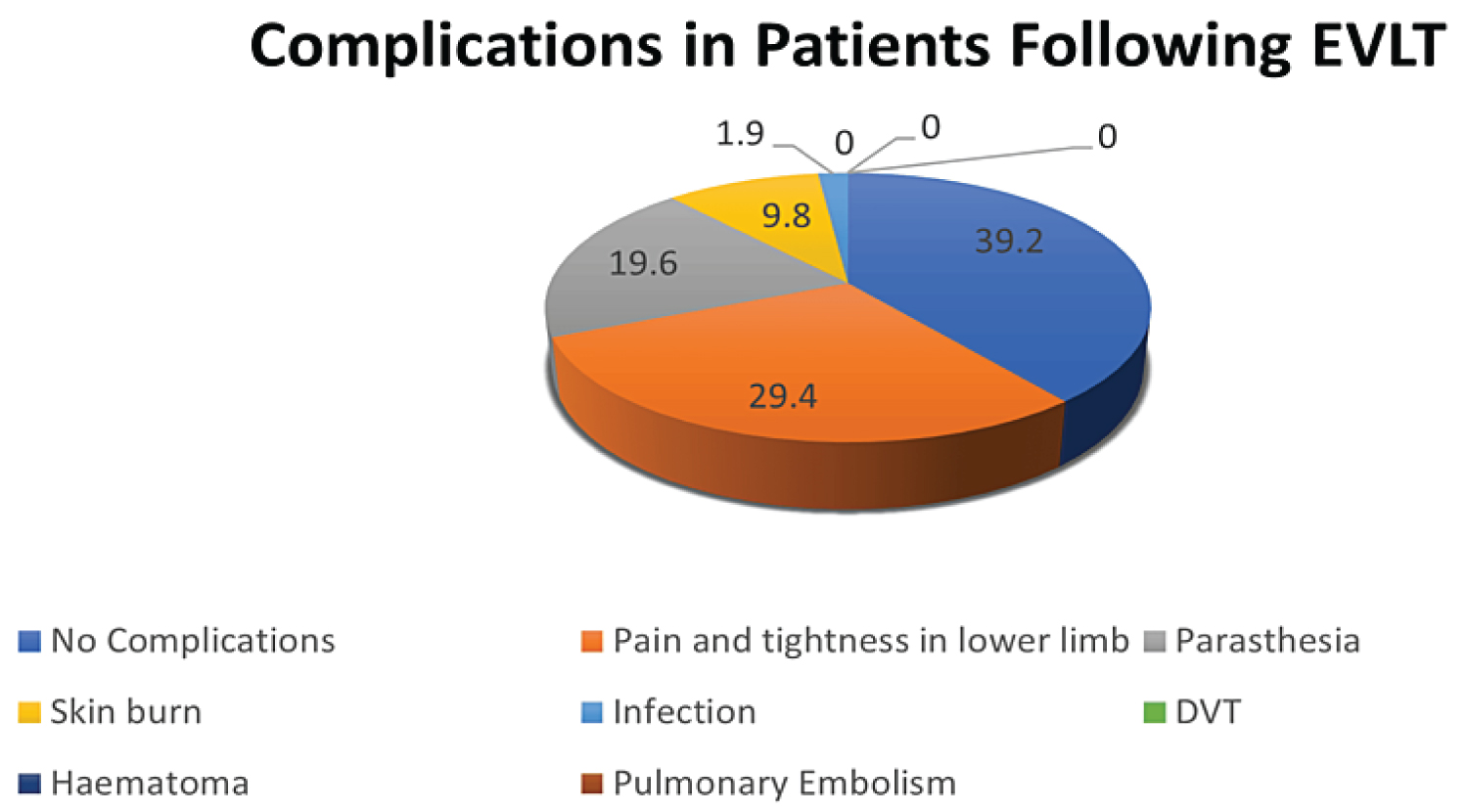 Figure 4: A figure showing complications in the patients following endovenous laser ablation therapy (EVLT) in our study.
Figure 4: A figure showing complications in the patients following endovenous laser ablation therapy (EVLT) in our study.
EVLT: Endo Venous Laser Therapy; DVT: Deep Vein Thrombosis
View Figure 4
In the present study, all the patients completed follow up protocols. The mean follow up duration was 1 year. Clinical examination correlated well with duplex USG findings. All patients showed improvement in the appearance of the limb with disappearance in the sizer and number of visible varicosities, one month after EVLT, relief of symptoms and significant improvement in the appearance of varicose veins was noted by 4-6 months after the initial treatment, pain was greatly improved or resolved in all treated limbs. Only 4 patients developed recurrence following varicose vein treatment out of 102 patients with EVLT on a daycare basis as shown in Figure 5.
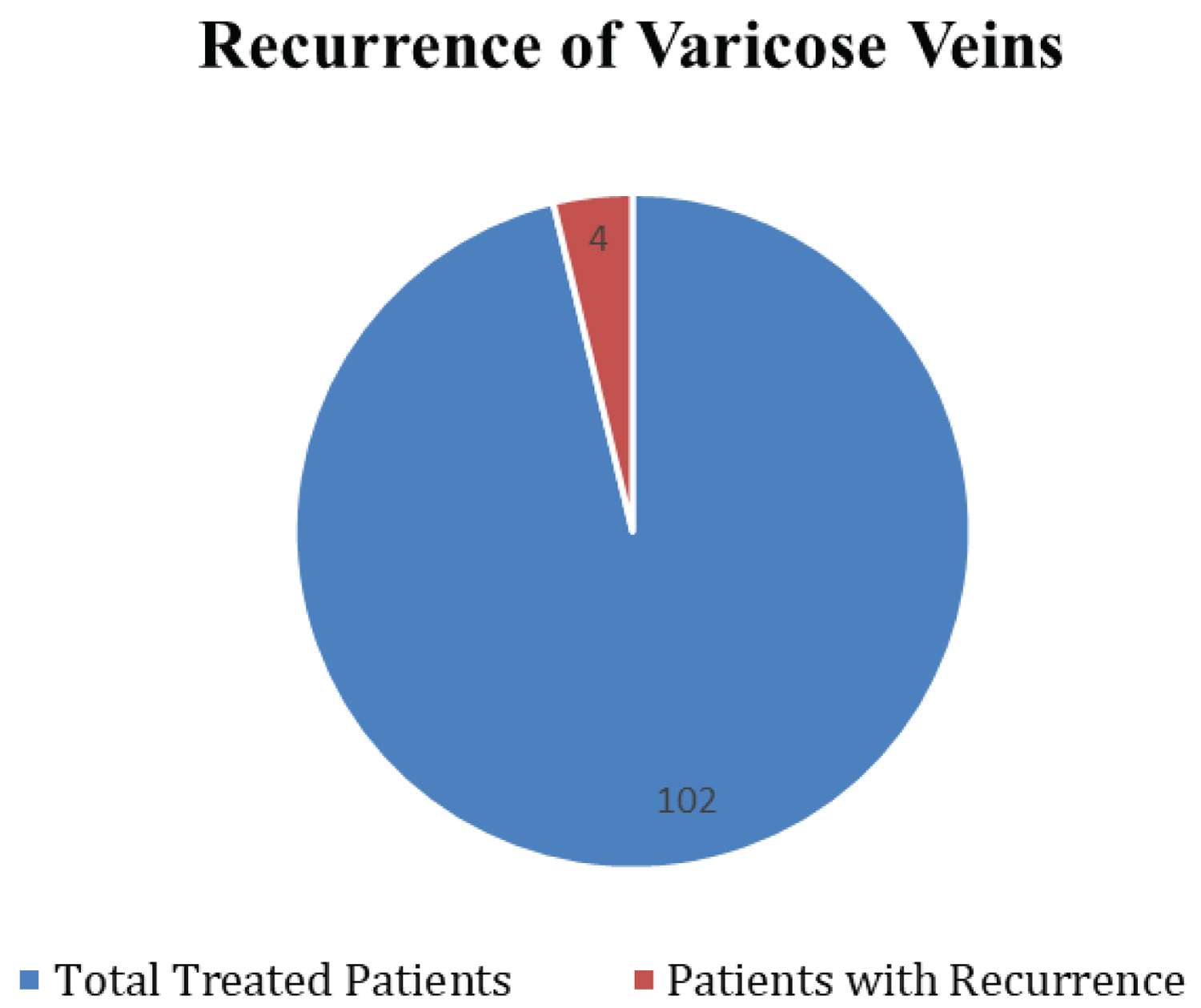 Figure 5: A figure showing recurrence of varicose veins in treated patients with EVLT.
View Figure 5
Figure 5: A figure showing recurrence of varicose veins in treated patients with EVLT.
View Figure 5
The development of minimally invasive endovascular procedures within the past ten years has resulted in a significant shift in the guidelines for treating symptomatic varicose veins [15]. In terms of occlusion rate and recovery time, radiofrequency ablation (RFA) and endovenous laser ablation (EVLA) are equally safe and effective [17]. Dr. Carlos Bone first presented EVLA at the 1999 International Union of Phlebology as a treatment for varicose veins. After inserting the laser fibre into the intended vein, a heat generator produces laser energy. The thermal light that the fibre tip generates causes localised thermal injury to the veins, which causes venous fibrosis, blood thrombosis, and vein constriction. Patients with inadequate saphenous veins seemed to respond well to EVLA therapy. For patients with symptomatic varicose veins, endovenous thermal ablation is advised as a first-line treatment and has replaced surgery to occlude and destroy the veins by employing heat [18].
In a comparative study conducted, ninety percent of patients in both treatment groups i.e EVLT and radiofrequency ablation groups reported symptom improvement following the operations, indicating that the primary clinical outcomes were similar for the two groups. In the limbs treated with laser therapy, ecchymosis, soreness, and intra- and post-procedural pain were somewhat but not significantly more common. At eight hours, twenty-four hours, one week, six months, and twelve months, there was statistically similarity between the two groups for all pain and tenderness levels. There were no serious issues, although the EVLA group saw a higher frequency of minor complications (p = 0.0210). Every follow-up visit, we also computed the AVVSS score for every patient and compared the outcomes [19].
During the past decade, increased interest in venous disorders and the development of new non-invasive diagnostic tests and minimally invasive treatment options have led to tremendous advancements in the understanding and management of varicose veins [18]. EVL ablation was introduced as an alternative to ligation and stripping and has rapidly become the treatment of choice for treating saphenous vein insufficiency [20].
The surgical treatment of varicose veins is not an issue that has been settled, and the dogmas do not represent absolute truths. Evidence suggests that the surgical approach, as has been recommended so far, may be the main event responsible for triggering biological phenomena that cause recurrent varicose veins for the ligation site of the SFJ, therefore it is paradoxically contrary to the objective of surgery itself. A more modern technique of the use and radiofrequency energy to eliminate saphenous vein reflux has been developed [21].
So despite the usage of low watt (10 watt) laser comparable results as reported in the literature with higher watt laser were achieved with low morbidity which further needs to be evaluated with prospective randomized control trails comparing different regimens. Even larger diameter veins more than 1 cm can be closed although they require more energy. So keeping this fact in the mind we routinely treat full of GSV although for SSV we spare lower one third to prevent nerve damage. Literature review suggests that female sex, increased age, pregnancy, geographical site and race are risk factors for varicose veins, however there is no hard evidence that family history or occupation are risk factors. Obesity also does not appear to carry any excess risk [22].
One possible explanation for the superiority of EVLT in terms of venous refilling time and clinical recurrence at distant sites is that a distinct hemodynamic state with physiological antegrade flow via groin tributaries follows EVLT. However, it is impossible to rule out a center bias brought on by varying intensities when doing the phlebectomies. Recurrent varicose veins, on the other hand, were more visually pleasing than clinically significant, as evidenced by the fact that they did not significantly affect venous severity rating or quality of life (QOL) in either group at the 2-year follow-up.
When it came to the time it took for a patient to resume work, endovenous laser treatment was helpful, but the difference was only 1.4 days, and the recovery period of 10 days was greater than what was predicted by the literature [16,17]. However, because recovery is a highly variable parameter that depends on a number of variables (such as the number of varicose veins and the number of phlebectomies performed simultaneously), the published studies are completely non-comparable due to the variety of methodologies and study populations used [23]. Varicose veins have been treated extensively with EVLT. For the treatment of varicosity of the GSV, EVLT is at least as successful as surgical procedures, despite the fact that different approaches yield varying outcomes. When it came to primary failure and recurrence, EVLT and surgery did not differ appreciably. EVLT is safe, and despite using more energy, the rate of complications has not increased.
Although few of the patients required additional complimentary procedures i.e. perforator ligation for residual varicosities starting one month after the discharge from the hospital, while most of the patients were discharged within 24 hours of the procedure.
Further prospective research on this subject would be beneficial, taking into consideration aspects like the Visual Analogue Score (VAS) pain score, the impact of compression stockings post-procedure, and the use of pre-procedure anaesthesia to determine its impact on complications and results.
In this study, only 4 patients developed recurrence following varicose vein treatment out of 102 patients with EVLT on a daycare basis. An occlusion of GSV along with its branches was achieved in most of the cases with self-limiting adverse effects and very few recurrence rates in the follow-up period. Relief of symptoms and a significant improvement in the appearance of varicose veins were noted 4-6 months after initial treatment, and pain was greatly resolved in all the treated limbs.
Nil.
Consent was obtained from or waived by all participants in this study.
In compliance with the ICMJE uniform disclosure form, all authors declare the following:
All authors have declared that no financial support was received from any organization for the submitted work.
All authors have declared that they have no financial relationships at present or within the previous three years with any organisations that might have an interest in the submitted work.
All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Dr. Aditya Sharma: Drafted the manuscript and submitted the manuscript under the supervision of Dr. Swati Pathak and Dr. Rajeshwar Yadav; Dr. Swati Pathak: Checked and made substantial contributions to the conception or design of the work and the acquisition, analysis, interpretation of data for the work and approved the final manuscript for publication; Dr. Rajeshwar Yadav: Checked and made substantial contributions to the conception or design of the work and the acquisition, analysis, interpretation of data for the work and approved the final manuscript for publication.