Background: Irreducible interphalangeal dislocations of the toes have traditionally been treated by surgical reduction fixed with a K-wire, screw or external fixator. In this study, the surgical implant was replaced by a plaster splint. This study aimed to describe an innovative approach to treating irreducible interphalangeal toe dislocations using a plaster splint in syndactyly and to evaluate the complications associated with this technique.
Method: This was a prospective, desciptive, multicenter study (Ivory Coast, Central African Republic) of 13 patients, seven men and six women with a mean age of 31.6 years (Extremes: 18 and 53), between July 2019 and November 2022. The diagnosis was confirmed by X-ray. The procedure was in all cases performed under Wide Awake Local Anesthesia No Tourniquet (WALANT). A classification based on the X-ray proved to be essential. It allowed the planning of therapeutic choices according to a precise algorithm. The surgical operation ended with a plaster cast splinting the toes for at least six months to evaluate the anatomical results and possible complications.
Results: The clinical and functional results were generally good. No dislocation had recurred. All patients were painless by the end of the first postoperative month. The reduction remained consistently stable in all cases. The patients showed significant clinical improvement, with decreased pain and satisfactory healing. Plantar flexion of the operated toes was generally good. Some minor complications, such as joint stiffness and insufficient plantar flexion, were corrected with rehabilitation sessions.
Conclusion: This experimental study demonstrates that surgical reduction of an irreducible toe dislocation can be effectively fixed with a plaster splint placing the toes in syndactyly. The results were similar to those of surgical implant fixation. This is a therapeutic approach that avoids the complications associated with the use of implants and offers satisfactory anatomical and clinical results.
Dislocation, Interphalangeal, Irreducible, Plaster splint, Toe, Treatment
An irreducible interphalangeal (IP) toe dislocation is a dislocation that cannot be reduced without surgical intervention, regardless of duration. Neglected IP toe dislocations are rare injuries [1-3]. The circumstance of occurrence is a forced hyperextension or hyperflexion done directly on the toe during a trauma [4]. As the skin stabilises the joint, the hypertensive flexor tendon and plantar plate lead to dislocation [5]. Incarceration of the collateral ligament, plantar plate or flexor tendon can make the dislocation irreducible. This incarceration is either spontaneous or induced by manipulation of the initial reducer. An irreducible dislocation requires open surgical reduction [6,7]. Usually, surgical reduction uses a K-wire, screw or external fixator to fix the joint after surgery [6-9]. In this study, the surgical implant was replaced by a plaster cast. This plaster splint placed the operated toe and the adjacent toe in syndactyly. To achieve good results, a management algorithm was developed. This algorithm was based on a new classification of the different IP toe dislocations. This study aimed to describe an innovative approach to treating irreducible interphalangeal toe dislocations using a syndactyly cast splint and to evaluate the complications associated with this technique. The hypothesis was that after surgical reduction, joint fixation with a plaster cast could achieve good results with the least possible complication.
This was a prospective, descriptive, multicenter study (Abidjan in Ivory Coast, Bangui in the Central African Republic, Fez in Morocco) conducted on 13 patients including seven men and six women with a mean age of 31.6 years (Extremes: 18 and 53) between July 2019 and November 2022. The patients had consulted on average 7.06 weeks (Extremes: 4 and 13) after the trauma. Patients under 18 years of age, metacarpophalangeal dislocations, a fracture of at least one bone involved in the dislocation, and those lost to follow-up were not included. There was no open dislocation. On admission, a local and then a general clinical examination was performed. An X-ray always completed the clinical examination to visualise the dislocation. Magnetic resonance imaging (MRI) was essential to search for an incarcerated tendon, collateral ligament or plantar plate. In this study, patients were unable to afford the expensive MRI scan. The diagnosis was therefore based on an X-ray and the irreducible nature of the dislocation. Once the diagnosis was confirmed and the course of treatment explained to the patient, a paraclinical assessment was always carried out. Consent was systematically obtained before surgery. Two patients had tried an initial reduction of their dislocations at home themselves, without success.
This study established an X-ray classification to prioritize the different IP dislocations on admission. It classified IP toe dislocations into six grades of increasing severity (Table 1). The higher the grade, the more difficult the treatment and the worse the prognosis. It was a novel classification using X-ray or CT images. The design of this classification was intended to allow treatment decisions to be planned according to a precise algorithm (Figure 1). It was a different classification from that of Miki published in 1988, which described only two types of dislocation in the big toe [10].
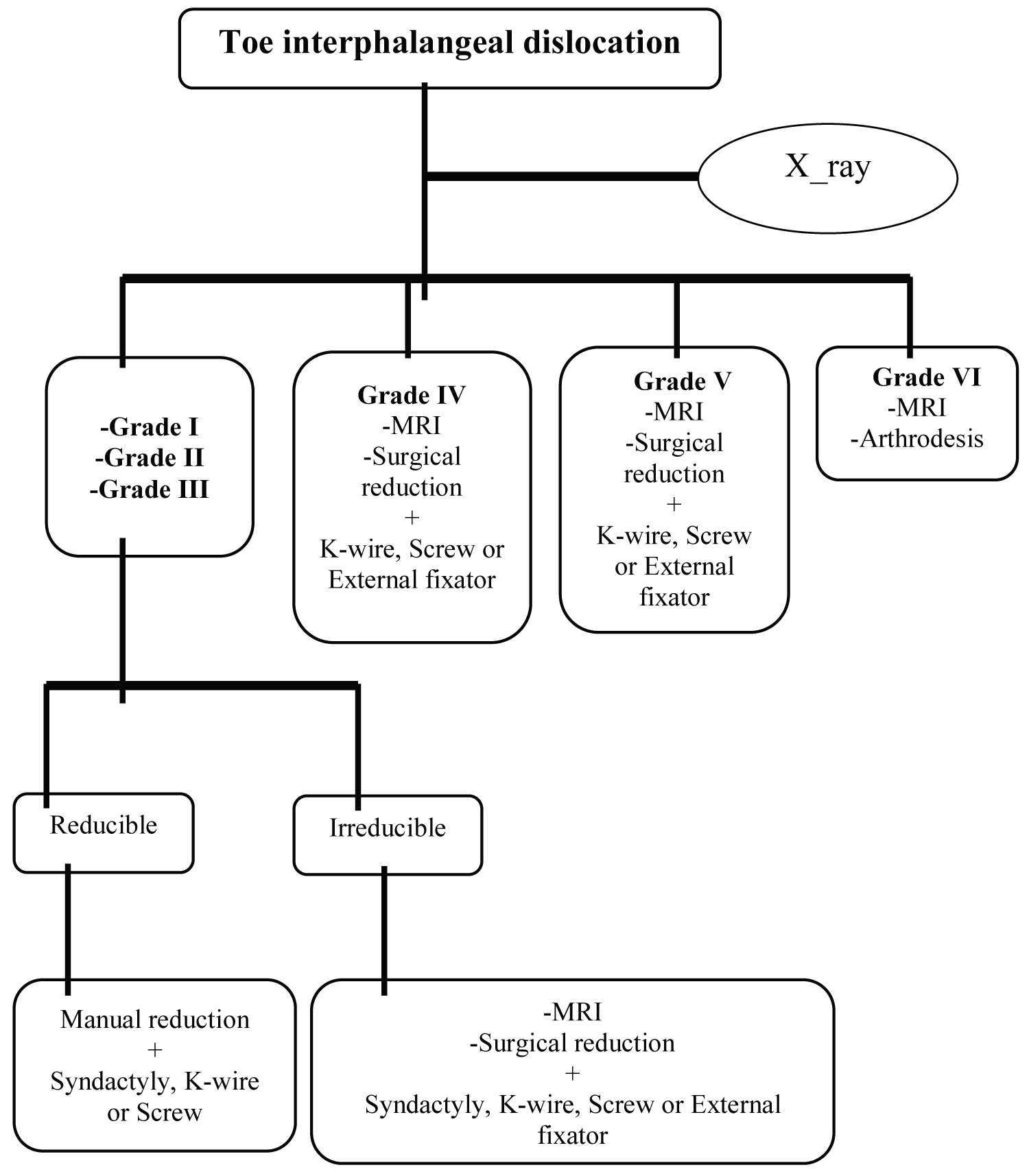 Figure 1: Algorithme de prise en charge des luxations MPT/IP des orteils
Figure 1: Algorithme de prise en charge des luxations MPT/IP des orteils
MRI: Imagerie par Résonnance Magnétique; X-ray: Radiographie.
View Figure 1
Table 1: Feigoudozoui's classification of IP toe dislocations. View Table 1
In all cases, the surgical procedure was performed under WALANT following a well-described dosage [11]. A mixture of one volume of sodium bicarbonate and nine volumes of 0.0005% Xylocaine adrenaline was injected around the dislocation, anteriorly and deeply, at a rate of 7 mL/Kg. There was a 30-minute waiting period between injection and incision. The total duration of anaesthesia was four to six hours [11].
The approach was dorsal, centered on the site of the dislocation. It exposed the joint and the incarceration perfectly (Figure 2). The incarcerated tendon, plantar plate or collateral ligament was gently disinserted. The manoeuvre of the dislocation mechanism reduced the joint surfaces. A possible ruptured plantar plate was sutured, as was the collateral ligament. Finally, after washing with saline, the skin was closed with a simple suture. The procedure ended with making a plaster splint (Figure 3). This was removable and placed at least two toes, including the operated toe, in syndactyly. The splint did not cover the ends of the toes and the surgical site. Finally, the splint should not compress the skin to preserve collateral vascularisation.
 Figure 2: (a) Dorsal approach; (b) Incarceration of the flexor tendon here indicated by the tip of the chisel.
View Figure 2
Figure 2: (a) Dorsal approach; (b) Incarceration of the flexor tendon here indicated by the tip of the chisel.
View Figure 2
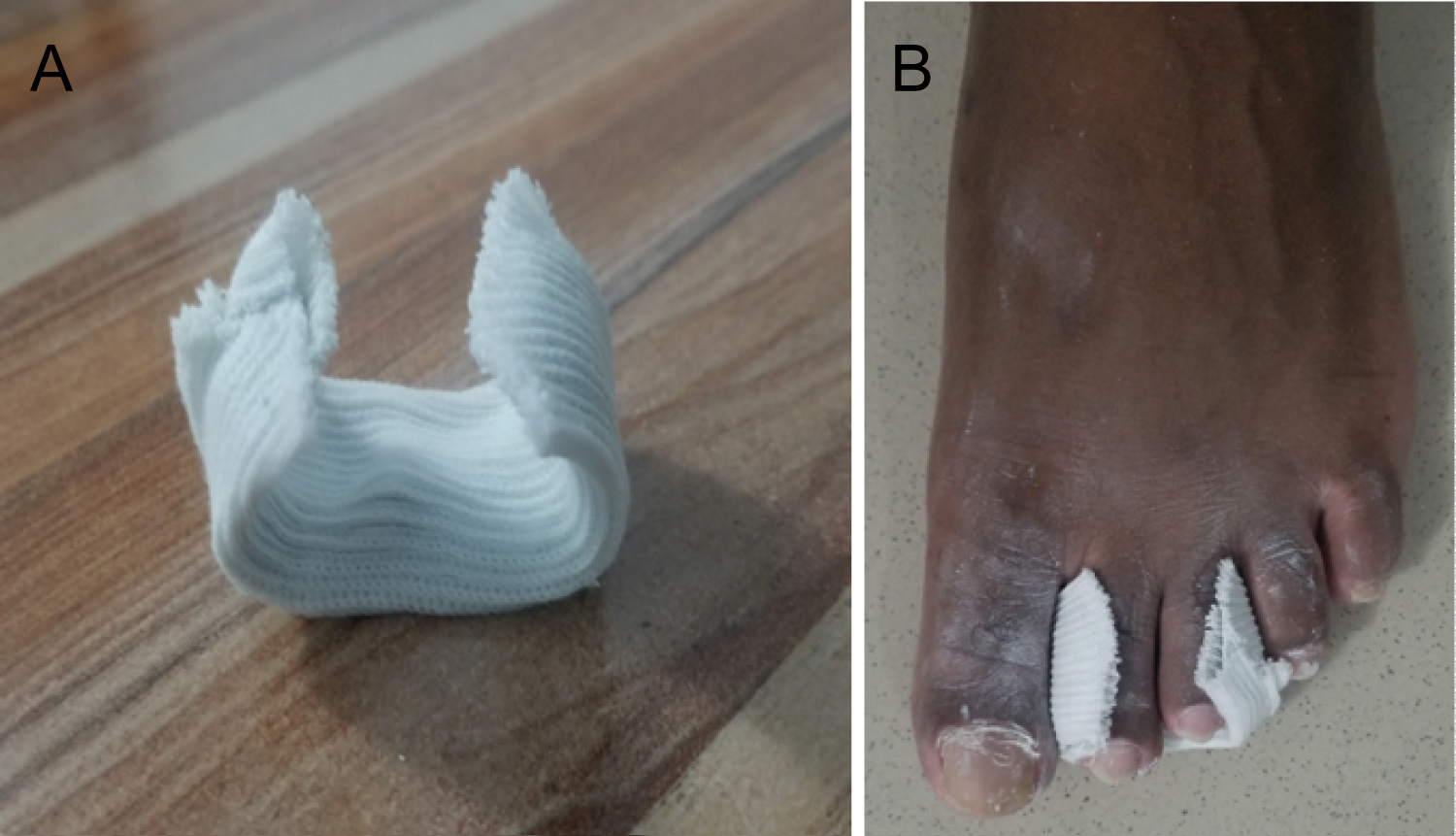 Figure 3: (a,b) The cast splint.
View Figure 3
Figure 3: (a,b) The cast splint.
View Figure 3
The patient was allowed to walk the day after the operation. Thromboembolic prevention was not necessary. Dressings were made every two days until complete healing. The stitchs were removed after two weeks. The plaster splint was permanently removed after four to six weeks. The rehabilitation sessions began the day after the final removal of the splint. Total return to work was possible in the second month after the operation. The patients were reviewed and examined once a month with X-ray control during the first three months postoperatively (Figure 4). The minimum follow-up period was six months.
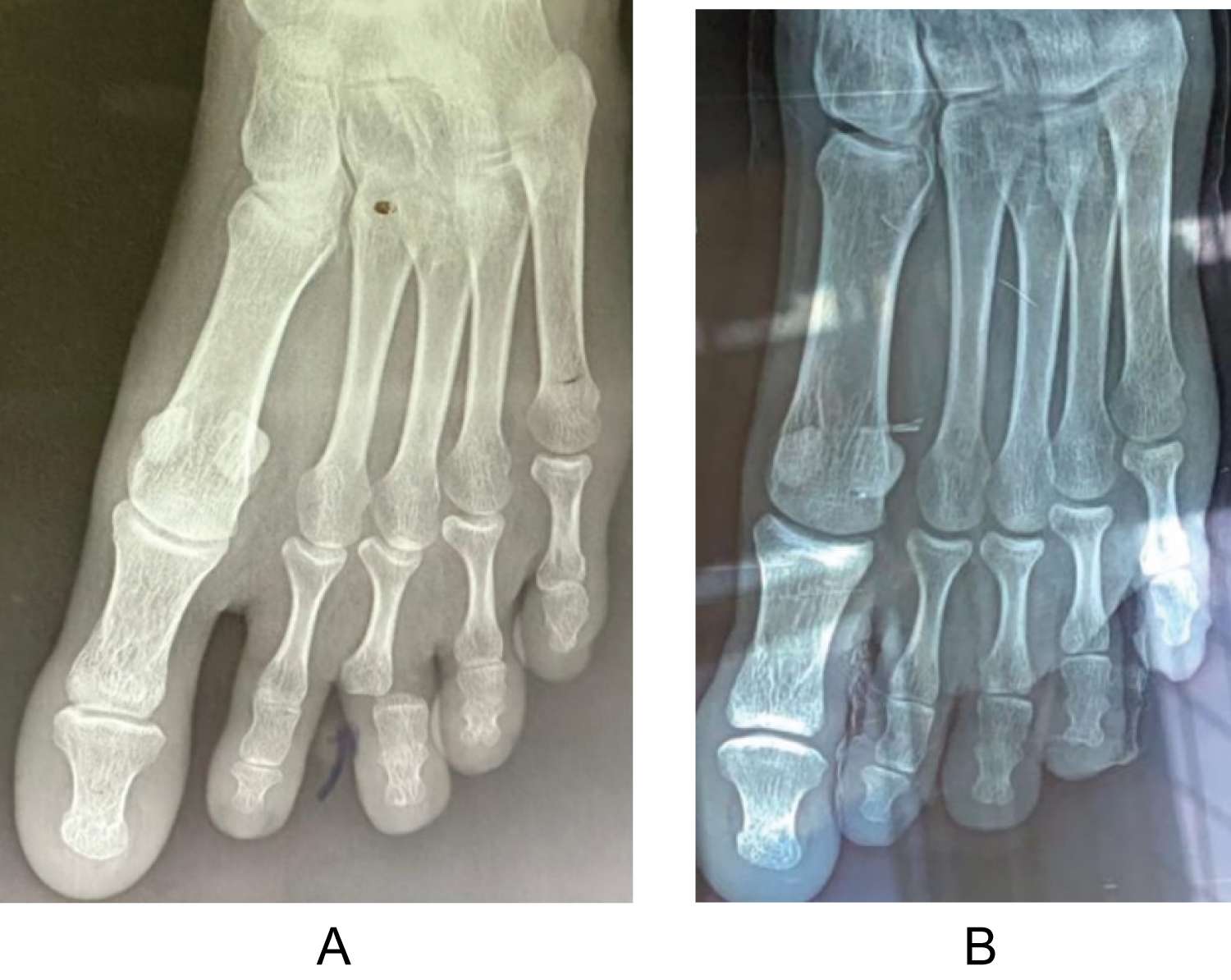 Figure 4: (a) X-ray images of the lesion and; (b) At eight weeks post-operatively.
View Figure 4
Figure 4: (a) X-ray images of the lesion and; (b) At eight weeks post-operatively.
View Figure 4
The clinical and functional results were generally good. The characteristics of the series are shown in Table 2. The information collected at the minimum 6-month follow-up examination is shown in Table 3. The fourth toe was the least affected in the series. Table 4 shows the anatomical findings at the six-month follow-up. Spontaneous recurrence was the occurrence of a new dislocation in the postoperative periods without any notion of trauma or external intervention. No dislocation had recurred. Flexion/extension movements of the toes were not considered significant in everyday life outside of certain specific jobs (driver, judoka, etc.). However, according to the study's assessment, a slight flexion/extension, especially with acceptable muscle strength, was sufficient for the result to be considered satisfactory. This was why joint amplitudes were measured during the clinical examination after six months.
Table 2: Characteristics of the series. View Table 2
Table 3: Distribution of clinical signs on admission. View Table 3
Table 4: Anatomical results at six months follow-up. View Table 4
This study's maximal medical visit delay of 13 weeks was much shorter than many others, some of which were as long as 30 years [6]. Persistent pain and functional discomfort on walking were the factors that prompted patients to consult us within a shorter time frame. The medical visit delay had no surgical impact. It did not influence the management. Irreducibility resulted from the incarceration of anatomical structure rather than the duration itself.
In our study, nine patients had initially consulted a health facility. The problem was that their dislocations were either irreducible from the outset or were caused by the initial practitioner's manipulations. The identification of incarcerated anatomical structures is usually made by magnetic resonance imaging (MRI), an expensive examination in our context. In the absence of MRI, practitioners were led to attempt manual reduction in the first instance. This highlighted the need for better diagnostic assessment to avoid incorrect manipulation and associated complications. In sum, some IP toe dislocations were iatrogenic or the result of self-reduction by the patient.
General anaesthesia is associated with peranaesthetic anaphylactic complications of varying severity [12]. Erythema, urticaria, arterial hypotension, collapse, cardiac arrest, cardiac rhythm disturbances and bronchospasm have been reported usually anaesthesia in adults [13]. Accidents such as convulsions, respiratory failure, cardiac arrest, and incidents such as headaches and arterial hypotension have been reported in the practice of spinal anaesthesia in sub-Saharan Africa [14]. Considering these complications, general anaesthesia or spinal anaesthesia could not be recommended as a first-line procedure for ambulatory surgery such as surgery of the extremities (hand and forefoot). However, some authors continued to operate on toes under general anaesthesia [15].
We opted for local anaesthesia without a tourniquet, known as WALANT. This technique has several advantages, including the absence of large material and financial resources, ease of use in a resource-limited setting, and safety for the patient [16,17]. Recent studies have demonstrated its effectiveness in extremity surgery [11]. It was a known and well-described technique, more often used successfully in extremity surgery with several advantages and almost no complications [18].
This study used a plaster cast to fix the reduction obtained after surgery, replacing surgical implants such as K-wires or screws. Surgical implants could increase the risk of osteoarticular infection, cause intraosseous pain and require re-intervention for their removal. In addition, the use of surgical implants would increase the cost of the procedure and require more materials. Plaster splints, on the other hand, would have the advantage of avoiding the complications associated with implants, being less expensive and not requiring additional materials (drill, image intensifier). This innovative approach to cast splinting has never been described in the literature. In our study, it effectively maintained the reduction of irreducible toe dislocation. By avoiding implants, the risk of osteoarticular infection could be avoided and patient comfort could be improved. In addition, the plaster cast was less expensive and its manufacture did not require the mobilisation of additional material, making it accessible in resource-limited settings.
All authors did not share the theory of using a surgical implant. Vaseenon, et al . thought that joint fixation with a K-wire was only indicated when the reduction was very unstable [6]. Some authors had fixed the reduction joint by syndactylisation but not by a cast, as in this study [19].
The clinical course of the patients was mostly good. All patients were painless by the end of the first month after surgery. This time of pain sedation was early compared to some cases where reduction fixation was done by K-wire. This was the case in the patient treated by Imao, et al. who reported persistent pain until the end of the second postoperative month [7].
Healing was satisfactory and acceptable in all cases. The most important thing was the stability of the reduction, which remained constant without any spontaneous recurrence.
Plantar flexion of the operated toes was around 45° in 10 patients at the third month and in all patients at the sixth-month clinical examination (Figure 5). The three cases where flexion was insufficient (10°-15°) were corrected by rehabilitation sessions.
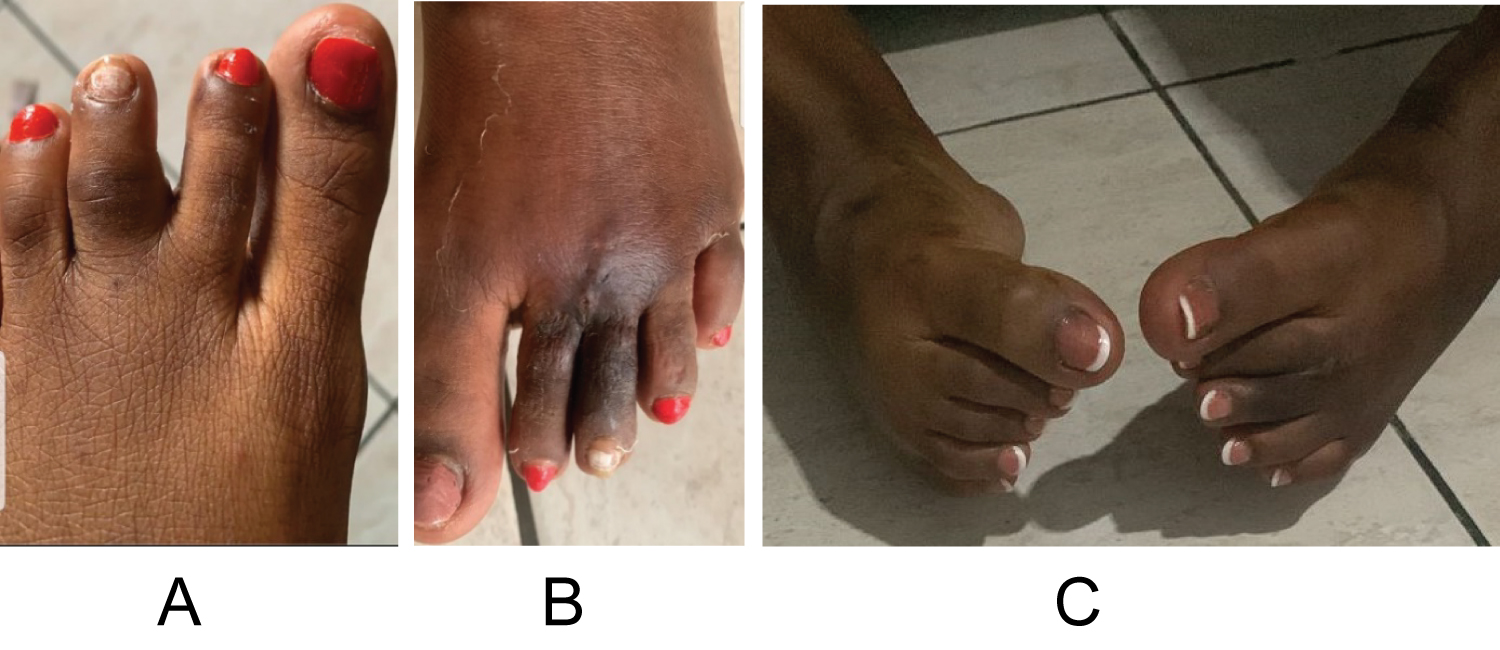 Figure 5: (a) Initial clinical aspect; (b) Skin aspect at two months follow-up; (C) Six months postoperatively, active flexion of the 3rd left toe up to 45° compared to the healthy right side.
View Figure 5
Figure 5: (a) Initial clinical aspect; (b) Skin aspect at two months follow-up; (C) Six months postoperatively, active flexion of the 3rd left toe up to 45° compared to the healthy right side.
View Figure 5
Complications were persistent mild joint stiffness in two patients and insufficient plantar flexion in three (Table 4). The patients underwent rehabilitation sessions which allowed them to correct the stiffness and achieve satisfactory flexion. It should be noted that these were complications that concerned only grade III patients who had consulted a little late. The higher the grade, the more difficult the treatment and the worse the prognosis. One toe with an irreducible interphalangeal dislocation reduced by Özdemir, et al. developed stiffness six months post-op [3]. In the literature, complications were generally very few.
This experimental study showed that surgical reduction of an irreducible toe dislocation could be effectively fixed with a plaster splint placing the toes in syndactyly. This treatment approach had advantages over surgical implants, such as preventing infection and intraosseous pain, improved affordability, and ease of placement. The results were the same as with K-wire, screw or external fixator. It was an affordable alternative for practitioners in resource-limited situations. Our classification was in preliminary testing in this study. It allowed us to prioritize dislocations to orientate their treatment better. The same was true for the management algorithm. It is important to note that our classification and management algorithm effectively guided the treatment of these dislocations. These results can serve as a basis for further studies and guide clinical practice in resource-limited settings.
Hermann Victoire Feigoudozoui and all co-authors declare that they have no conflict of interest.
No funding was received for the purposes of performing this study.