We report a rare complication following a common operation, of an intramedullary tibial nail migrating through the posterior cortex of the tibia to sit within the deep posterior compartment of the lower leg, presenting 10 years after index procedure. Follow-up radiographs one year post-operatively confirmed union and an intramedullary position of the nail. After locking bolt removal, due to prominence, the patient re-presented 10 years later with FHL irritation and radiographs confirmed the nail had migrated to sit outside the tibial canal. Although rare, this case report highlights the need to be critical in the confirmation of union, as an un-united fracture can lead to micromotion and ultimately nail protrusion.
Diaphyseal tibial fractures are the most common long bone injury, with an incidence of 16.9 per 100,000 per year [1]. Males between 10 and 20 have the highest frequency of injury, with the most common mechanisms of injury being sporting activities and road traffic collisions [2]. Whilst these fractures can be managed with a cast, modern treatment for displaced diaphyseal fractures commonly utilizes antegrade, reamed intramedullary nails. These are load sharing devices which sit within the medullary canal of the tibia, resisting compressive, bending and torsional forces [3]. Fracture union is achieved through a relative stability principle, preserving fracture callus and allowing bony union with preservation of length, alignment and rotation. Proximal and distal locking bolts can increase the stability of the construct, in particular resistance to torsion, but risk delaying healing of distracted fractures, iatrogenic injury to neuromuscular structures and pain [4,5]. Screws can be removed 1-2 years following primary fixation following fracture union.
There has been a reported case of distal migration of a Küntscher tibial nail related to micromotion and subsequent bony erosion of the nail 16 years later [6]. This phenomena has been seen in the femur, again a stainless steel, slotted Küntscher nail with no locking screws [7,8]. However to our knowledge there have been no documented cases of migration of a reamed, locked, modern design titanium tibial nail following locking bolt removal.
A 20 year old man suffered a closed, oblique fracture of his right tibial diaphysis at the junction of the middle and distal third with an associated fibula fracture whilst playing football (Figure 1). His tibia was stabilised with an antegrade, reamed, intramedullary nail and proximal and distal bolts, on a planned trauma list. The position on intraoperative fluoroscopy and post-operative radiographs show an appropriate reduction and position of the nail (Figure 2). Immediate weight bearing as pain allows was commenced post-operatively and after clinical and radiographic union, was permitted to return to sport and work as a crane driver.
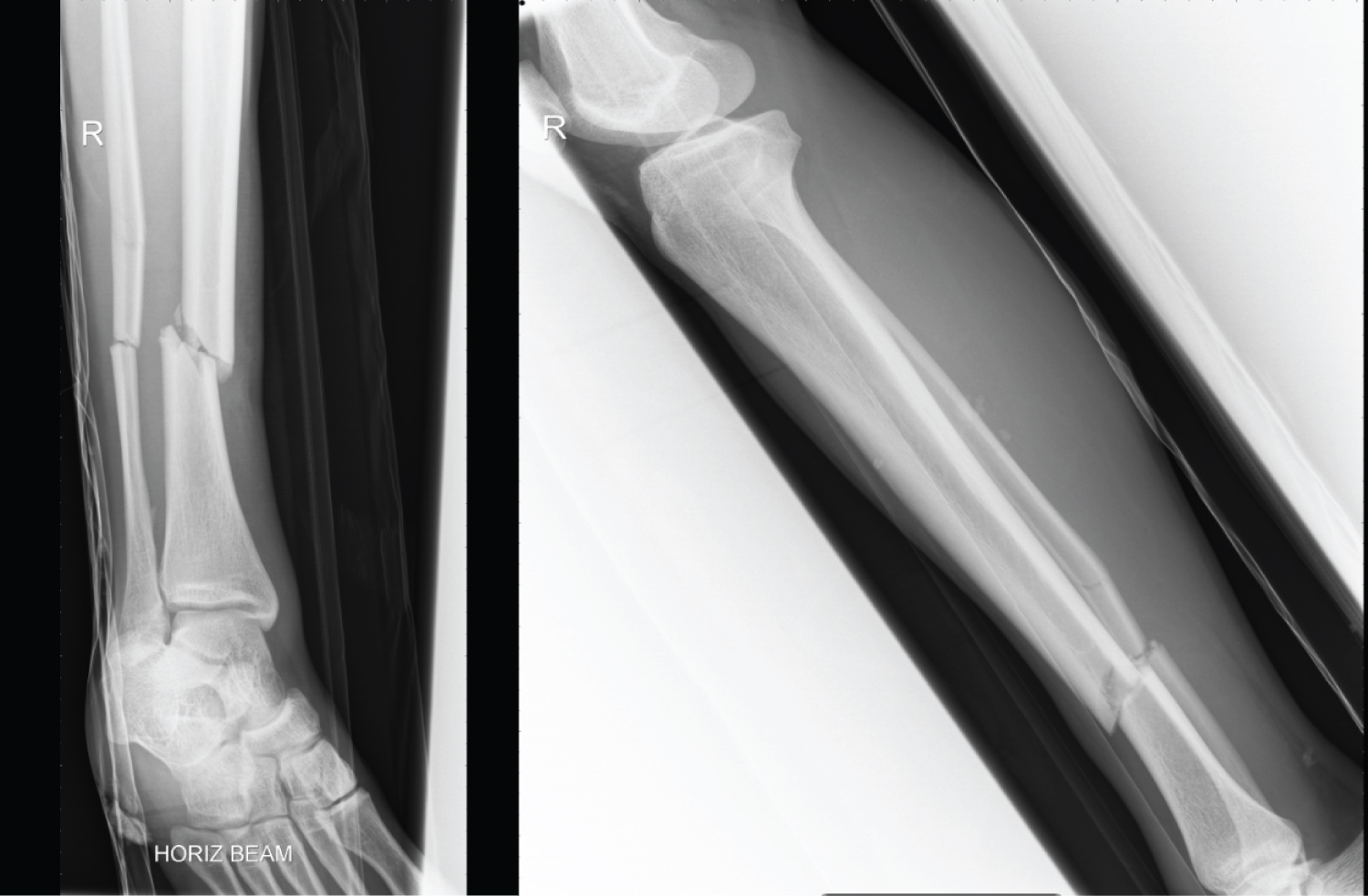 Figure 1: AP + Lateral X-ray prior to surgical intervention. View Figure 1
Figure 1: AP + Lateral X-ray prior to surgical intervention. View Figure 1
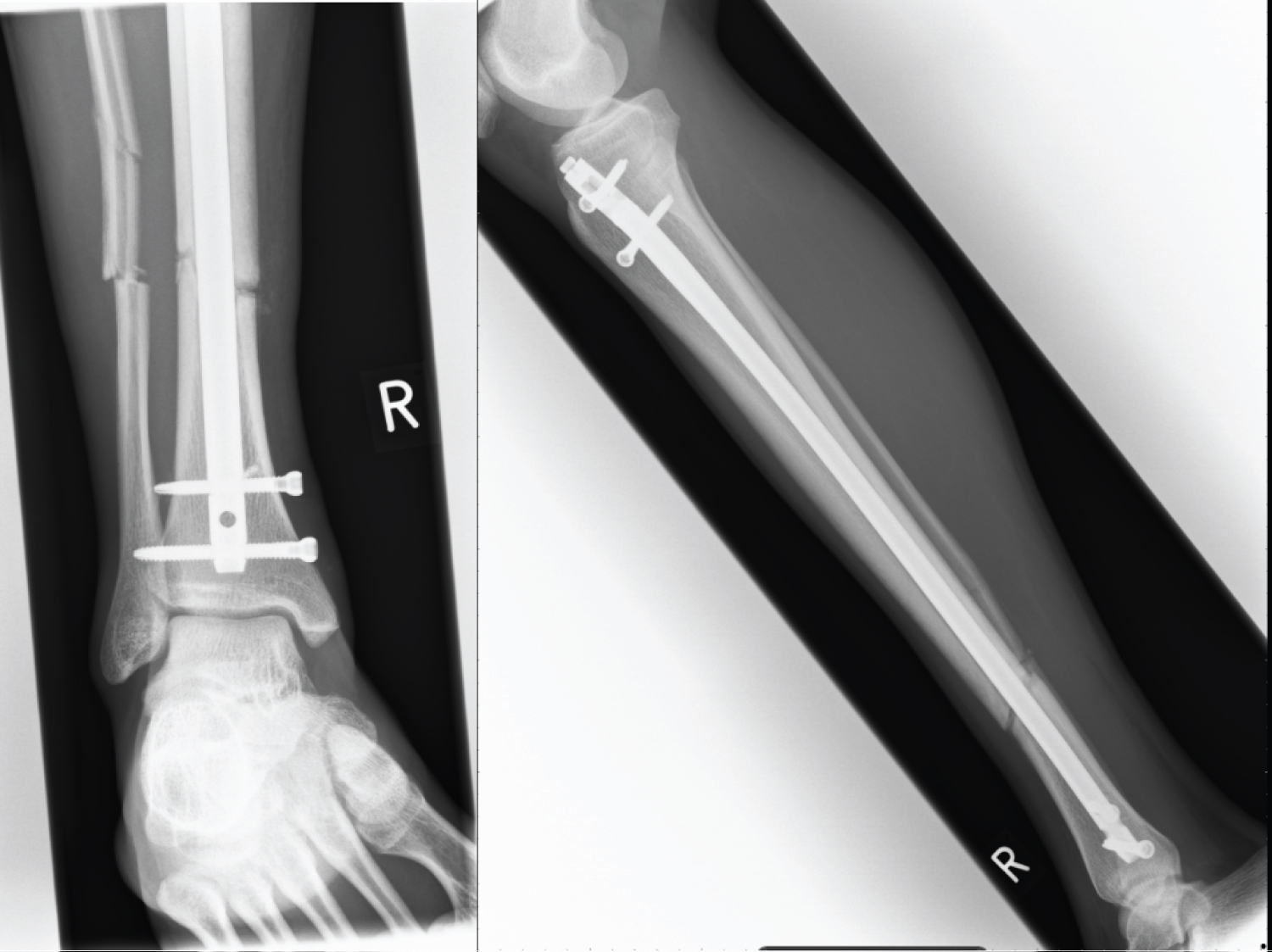 Figure 2: AP + Lateral X-ray 4 weeks post ORIF. View Figure 2
Figure 2: AP + Lateral X-ray 4 weeks post ORIF. View Figure 2
1 year post-operatively the prominence of the distal locking bolts caused pain when kicking a football and he was duly listed for removal of the distal bolts only 12 months post-operatively (Figure 3). Following recovery from bolt removal, a gradual return to football was allowed. Over the subsequent 12 years the patient suffering an insidious onset progression of pain in the distal tibial, particularly in the morning and whilst playing sport, prompting referral through to the orthopaedic services for follow-up 13 years post-operatively.
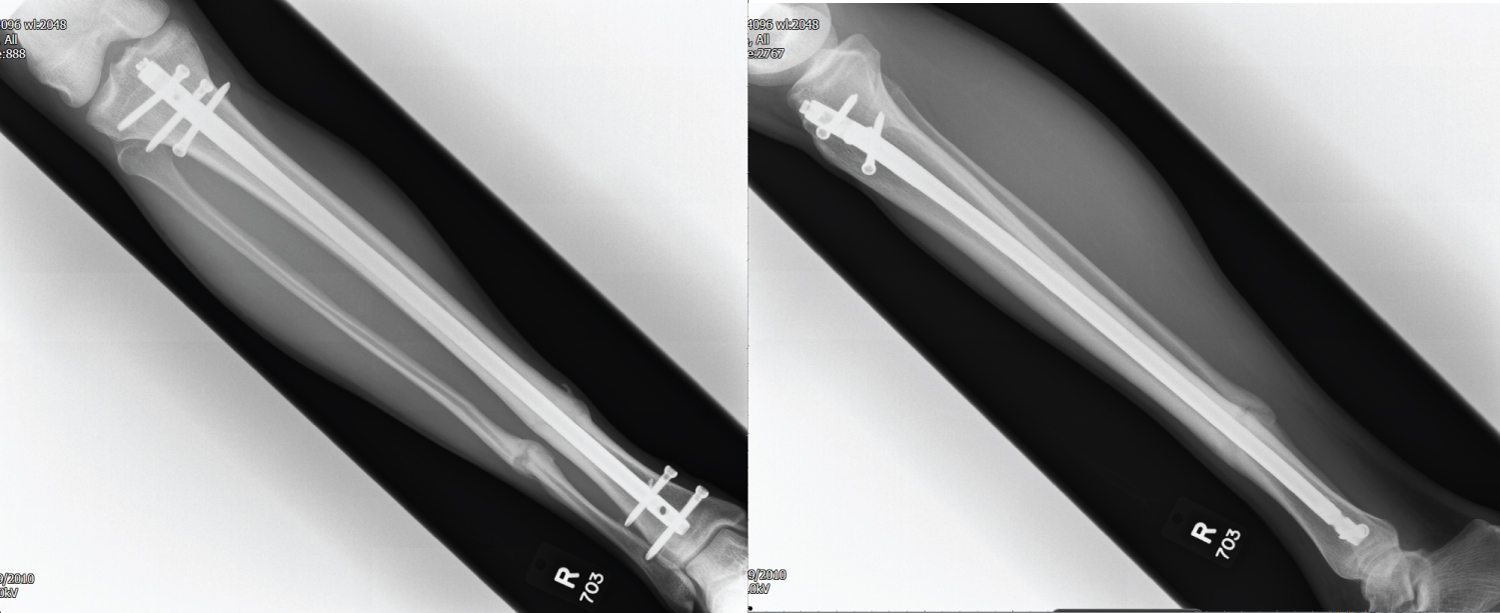 Figure 3: AP + Lateral X-ray 9 months post ORIF prior to distal screw removal. View Figure 3
Figure 3: AP + Lateral X-ray 9 months post ORIF prior to distal screw removal. View Figure 3
On review, the patient's wounds had healed and there was no evidence of infection or swelling and the fracture site remained non tender with no evidence of motion or erythema. Mildly reduced dorsiflexion and an antalgic gait remained the only positive findings on examination. Radiographs taken following clinical review demonstrated distal nail protrusion into the deep posterior compartment posteriorly, with appropriately sited proximal nail with two bi-cortical bolts in-situ (Figure 4). Blood tests to investigate for infection, Bone profile and an ESR returned within normal limits, other than an elevated ALP suggesting higher than normal bone turnover. A CT scan confirmed migration through the posterior cortex distally abutting the belly of flexor hallucis longus (Figure 5).
 Figure 4: AP + Lateral X-ray showing distal protrusion of IM nail 10 years post distal locking screw removal. View Figure 4
Figure 4: AP + Lateral X-ray showing distal protrusion of IM nail 10 years post distal locking screw removal. View Figure 4
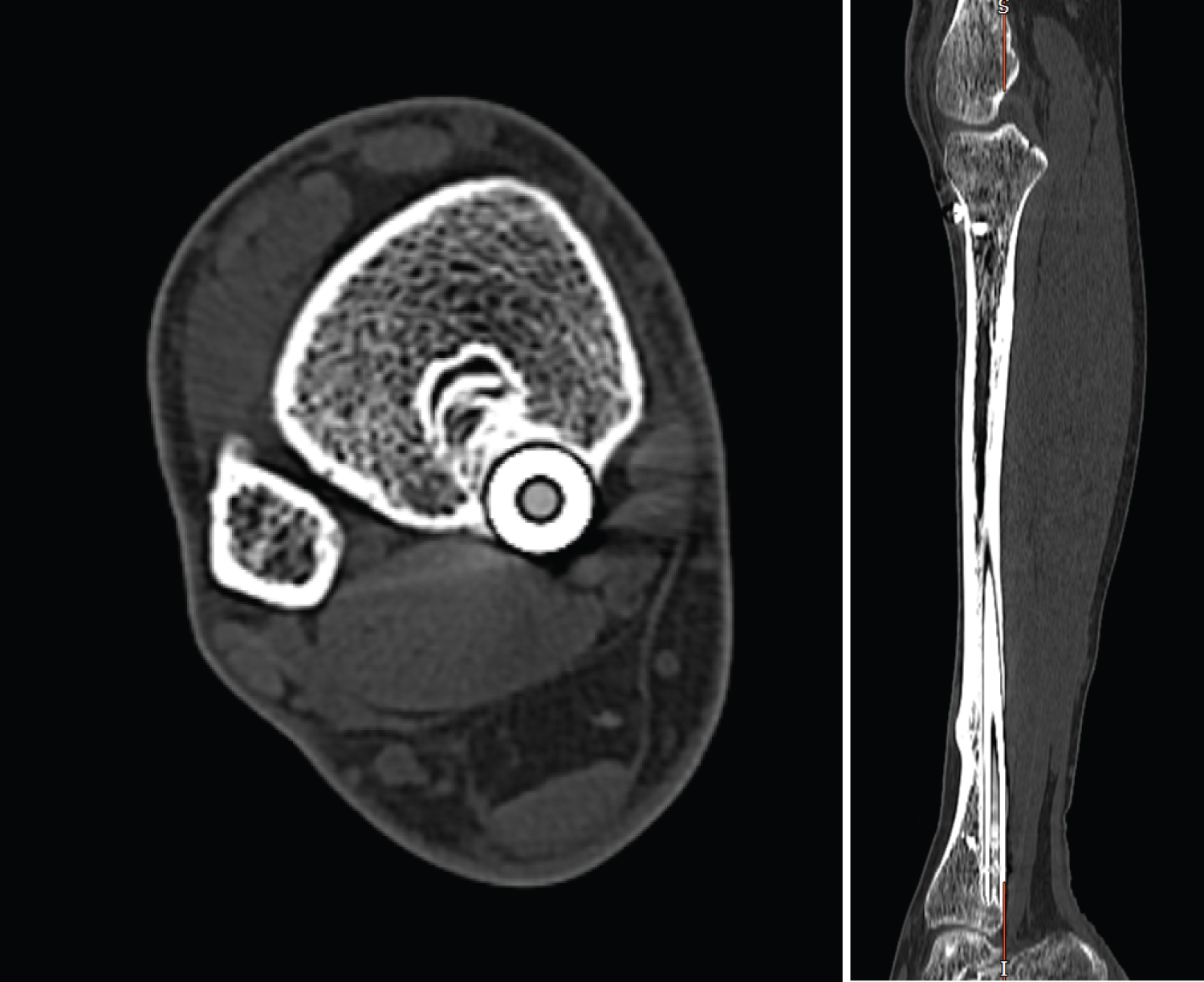 Figure 5: CT Axial and Sagittal view showing distal protrusion of IM nail 10 years post distal locking screw removal. View Figure 5
Figure 5: CT Axial and Sagittal view showing distal protrusion of IM nail 10 years post distal locking screw removal. View Figure 5
In the six weeks between initial presentation of pain and results of CT scan, the patient was advised to reduce activity and refrain from football. This resulted in his symptoms largely settling and functionality returning close to his baseline. Surgical intervention to remove the nail was discussed, but the patient felt in the absence of symptoms he was not prepared to accept the risks involved and time involved post-operatively with activity modification to allow the bone to consolidate. Therefore a shared decision was made to continue observation and proceed for removal if symptoms returned.
This case describes a rare complication from a commonly utilized method of stabilizing a diaphyseal tibial fracture. Migration of Küntscher nails secondary to wrong sized nails, fixation with faulty technique, osteoporosis and infection have been reported [9,10]. However these problems have largely been admonished by the introduction of locking bolts.
In our case, the initial nail position was appropriate and that follow up x-rays 7 months later shows suitable healing and intramedullary nail position. The distal locking screws were removed at 12 months. It may well be that despite the absence of pain and confirmed bridging callus in all four cortices on follow-up radiographs there was not yet rigid union. Therefore by removing the distal locking bolts this allowed micromotion of the nail within the tibia, permitting re-modelling around the sites of stress and eventual protrusion of the nail into the deep posterior compartment. The working length in modern nail designs with proximal and distal locking bolts was therefore reduced after distal locking bolt removal. Given the patients young age, lack of comorbidities and active lifestyle it is unlikely to result from systemic patient related factors or disuse osteoporosis.
Therefore this complication could potentially be prevented by waiting for removal of locking bolts until a minimum duration of 18 months following tibial nail insertion or if symptoms require earlier removal, then the use of three-dimensional imaging such as a CT scan should be used.
Migration of a tibial nail is a rare complication. It is recommended that is considering locking bolt removal prior to 18 months following insertion of the nail, then a CT scan be performed to confirm bony union to offer adequate stability.