Surgical treatment of high-load fractures in patients with osteoporosis and compromised soft tissue is challenging and often results in unsatisfactory implant fixation. We describe a case of an 80-year-old female patient with severe osteoporosis and a pre-existing knee arthroplasty. Initially, she required an external fixator following a bimalleolar ankle fracture that was followed by a peri-implant spiral tibial shaft fracture with severely compromised soft tissue condition. The patient was successfully treated with a photodynamic bone stabilization system (PBSS) (IlluminOss® System) supported by an angular stable plate as external fixator. The patient was discharged seven days later. At follow-up after six months, the patient was able to bear full weight bear without assistance and had no complaints. To our knowledge, this is the first report describing a bimalleolar ankle with a concomitant peri-implant tibial shaft fracture treated with a photodynamic bone stabilization system supported by angle stable osteosynthesis in form of external fixator.
Ankle fracture, Compromised soft tissue conditions, IlluminOss®, Knee prosthesis, Minimal invasive, Osteoporosis, Photodynamic bone stabilization system
Ankle fractures remain the third most common musculoskeletal injury in the elderly population. Surgical treatment of these fractures can be challenging due to their weaker bones, multiple comorbidities, circulatory problems, or even skin damage, which in turn interferes with normal healing [1,2]. Current treatment options for ankle fractures include simple immobilization, percutaneous wire placement, intramedullary nail fixation, and open surgical stabilization with or without the use of plates and screws, or bone grafts. The choice of treatment depends on the severity of the fracture, the degree of comminution, the loss of bone material and the soft tissue conditions [3]. In cases of severe osteoporosis and compromised soft tissue, conventional treatments are usually unsatisfactory as the bone is functionally impaired and less able to hold screws and implants, yet the compromised soft tissue creates unfavorable conditions for implant fixation [3,4]. A new approach is the photodynamic bone stabilization system (PBSS), the IlluminOss® system (IS), which received European approval in 2009 [3]. IS-PBSS is a system consisting of a light-curing resin that allows the formation of customized intramedullary implants. In this system, a monomer is placed in a thin-walled polyethylene terephthalate (PET) balloon catheter that is advanced into the medulla and then polymerized in situ by applying light of a specific wavelength [5,6]. This system represents a new treatment paradigm for the fixation and stabilization of fractures with severe osteoporosis, pathologic fractures, or other fractures with compromised soft tissue conditions, provided that the fracture involves non-weight-bearing to low-weight-bearing bones [3,7,8]. The aim of this study was to describe the clinical and radiological results after stabilization of a bimalleolar ankle fracture with an additional tibial shaft fracture with IS-PBSS, and to highlight that this minimally invasive procedure could be an alternative for surgical treatment of peri-implant fractures as well as osteoporotic ankle fractures with compromised soft tissue conditions. To our knowledge, this is the first report describing the use of the IS-PBSS system with supportive osteosynthesis in the form of an external fixator in fractures involving highly loaded bones with coexisting severe osteoporosis and compromised soft tissue conditions.
An 80-year-old female patient with severe cardiopulmonary disease (NYHA 4), end-stage renal disease, severe osteoporosis and a coexisting total knee arthroplasty fell on her side and sustained an unstable bimalleolar ankle fracture. Due to the major comorbidities and the compromised soft tissue condition, we decided to treat the fracture primarily with an external fixator. Three weeks later, the patient fell again and presented to our emergency department with severe pain in the same leg. On physical examination, the Schanz screws were loose both proximally and distally. The soft tissue conditions on the lateral and medial sides were compromised and undermined by hematoma. The radiograph showed a peri-implant long-segment spiral comminuted fracture at the tibia shaft at the level of the proximal Schanz screw. Due to the critical soft tissue condition, the severe osteoporosis, and the pre-existing knee arthroplasty which in turn limits the antegrade treatment with intramedullary nail fixation, we opted for a minimally invasive technique utilizing a photodynamic bone stabilization system (IlluminOss® system) to stabilize the fibula and tibia; temporary transverse osteosynthesis with angular stable plate and screws in the form of an external fixator was also planned to increase stability. The patient gave her written consent for surgery.
The surgical procedure was performed in the prone position under general anesthesia. The external fixator was first removed, and all Schanz screws were manually extracted given that they were very loose. We started the surgery by stabilizing the fibula. The straight awl was used to locate the optimal entry point at the tip of the fibula under fluoroscopy guidance. After opening the medullary canal, the curved awl was inserted, followed by intramedullary insertion of the elastic wire retrogradely, the position of the wire was controlled with an intraoperative fluoroscopy and the selected balloon catheter of the IlluminOss® system was then inserted. After reduction of the ankle, the balloon was inflated and filled with the monomer, then the curing process was initiated. The balloon was then removed at the bone tip. The intra-operative X-ray showed the correct position of the balloon with correct reduction. Now a second minimal skin incision was made on the tibia distally at the inner ankle tip. Same procedure was repeated with the exception that the intramedullary space was drilled to a size of 8.5, leaving a space for the balloon catheter of the IlluminOss® system to be inserted. To achieve better stability, an angular stable 4.5 Synthes plate was used as a temporary external fixator. The most proximal screw was then placed at the desired position directly under the tibia prosthesis stem, and the screws were inserted proximally and distally over the plate penetrating the IlluminOss® system. Fluoroscopy guidance in both planes shows the correct position of the intramedullary IlluminOss® and the correct position of the bicortical screws at the tibia and fibula. The wound was then closed in a routine fashion (Figure 1 and Figure 2). On the second day of surgery, partial weight bearing of 15-20 kg was started for 6 weeks. After removal of the material, the patient was gradually able to bear full weight. The patient was followed up regularly, after 6 months she reported regaining pre-traumatic mobility.
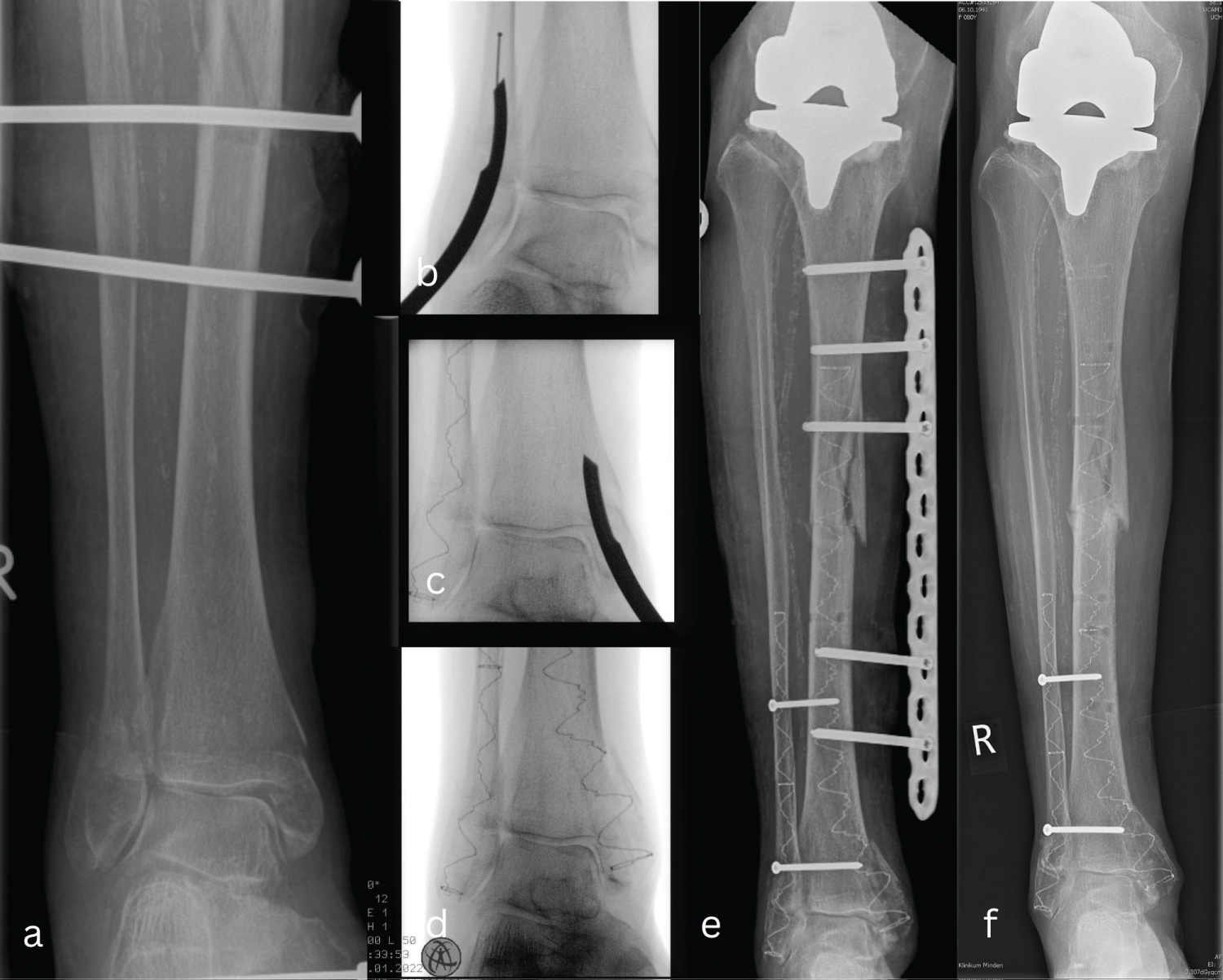 Figure 1: (a) Peri-implant tibial shaft fracture by coexisting bimalleolar ankle fracture primarily fixed with an external fixator; (b-d) Chronological steps for the minimally invasive technique with the photodynamic bone stabilization system (IlluminOss® system) to stabilize the fibula and tibia; (e) A temporary transverse osteosynthesis with angular stable plate and screws in the form of an external fixator was performed to increase stability; (f) 2 months postoperatively shows a consolidated fracture. View Figure 1
Figure 1: (a) Peri-implant tibial shaft fracture by coexisting bimalleolar ankle fracture primarily fixed with an external fixator; (b-d) Chronological steps for the minimally invasive technique with the photodynamic bone stabilization system (IlluminOss® system) to stabilize the fibula and tibia; (e) A temporary transverse osteosynthesis with angular stable plate and screws in the form of an external fixator was performed to increase stability; (f) 2 months postoperatively shows a consolidated fracture. View Figure 1
 Figure 2: (a-c) After opening the medullary canal, the curved awl was inserted followed by the insertion of the elastic wire retrogradely, after controlling the position of the wire with intraoperative fluoroscopy, the selected balloon catheter of the IlluminOss® system was then inserted. After reduction of the ankle, the balloon was inflated and filled with the monomer, then the curing process was initiated. Same procedure was done to the tibia. The intraoperative X-ray showed the correct position of the balloon with correct reduction; (d-e) After completion of the curing process, an angle-stable 4.5 Synthes plate was used as a temporary external fixator; (f) Soft tissue condition after removal of the material in 3 months. View Figure 2
Figure 2: (a-c) After opening the medullary canal, the curved awl was inserted followed by the insertion of the elastic wire retrogradely, after controlling the position of the wire with intraoperative fluoroscopy, the selected balloon catheter of the IlluminOss® system was then inserted. After reduction of the ankle, the balloon was inflated and filled with the monomer, then the curing process was initiated. Same procedure was done to the tibia. The intraoperative X-ray showed the correct position of the balloon with correct reduction; (d-e) After completion of the curing process, an angle-stable 4.5 Synthes plate was used as a temporary external fixator; (f) Soft tissue condition after removal of the material in 3 months. View Figure 2
Ankle fractures are the most common fractures of the lower extremities and are generally treated surgically. The most common treatment options for ankle fractures include simple immobilization, fixation with intramedullary nails, and open surgical stabilization with plates and screws [2-4,9].
With open reduction and internal fixation, surgical access is a major limiting factor and the use of multiple screws in weakened bone presents an additional risk [8]. In elderly patients, the postoperative complication rate after plate and screw fixation of lateral malleolar fractures was shown to be as high as 40% [5,7,8,10].
In the case of intramedullary nail fixation, although this minimally invasive technique seems to be a satisfactory method for high-risk patients, especially to avoid complications and shorten hospital stay [11], such an implant is not form-filling: The rigid metal implant exerts stress when inserted into the curved medullary cavity, which promotes undesirable dislocation of the fragments [3]. Consequently, none of the current modalities is ideal for the treatment of fragility fractures or fractures with a compromised soft tissue situation [3,7].
Recognition of these concerns led to the development of radiolucent implants such as the minimally invasive Photodynamic Bone Stabilization System (PBSS; IlluminOss® System) [3,7,8,12]. This concept has many advantages: Particularly the fact that the bone access, unlike the metal implant, does not have to be chosen exactly in the axis of the medullary cavity, but an access adapted to the soft tissue situation [3,7,8,12]. In addition, the monomer remains drillable after the curing process, which potentiates its features for additional osteosynthesis fixation, if required [13].
The PBSS system has been successfully used in the treatment of pathological osteolysis and fractures of the humerus, metacarpal and forearm fractures, as well as for stabilization of pubic bone and acetabular fractures [6,12-15]. In a randomized controlled study done by Zyskowski, et al. the outcome after osteosynthesis comparing AO technique and PBSS in distal fibula fractures showed that the use of the IlluminOss® System leads to a reduction in postoperative complications and early hospital discharge in the elderly [16]. Moreover, it´s use is of particular value for the surgical repair of osteoporotic fractures, offering improved stability and excellent clinical outcomes [14].
An additional advantage of PBSS is that its flexibility allows the balloon to be inserted into the medullary cavity through a small soft tissue and bone access when folded, thus anchoring itself in the medullary cavity and subsequently enlarging the bone-implant interface, resulting in great stability [15].
In our case, the co-existing severe osteoporosis and compromised soft tissue conditions posed a risk for plate osteosynthesis, and the concomitant ipsilateral total knee arthroplasty limited the use of anterograde intramedullary nail fixation, making IS-PBSS an ideal alternative for this particular case provided it is additionally stabilized with osteosynthesis. The choice of the angle-stable plate and screws as the external fixation concept was based on three reasons: First, the Schanz screws were already too loose after 3 weeks that they could be pulled out by hand, which in turn posed a risk for reuse; second, the Schanz screws are thicker than the angle-stable screws and could therefore weaken the IlluminOss system; third, if the external fixator were to be reused, carbon rods would have to be inserted in double rows, which would have further hindered patient mobilization.
The results of our case report suggest that a high-loaded bone can be safely stabilized with the PBSS system when supported with osteosynthesis material. Our results also show that adequate mobilization, low pain, and a low complication rate could be achieved after IS-PBSS treatment of bimalleolar ankle fractures with compromised soft tissue conditions.
The overall success of ankle fracture fixation depends on many factors, yet preservation of the soft tissue envelope must be paramount to avoid poor postoperative outcomes. IS-PBSS is a simple surgical technique that is minimally invasive and associated with rapid recovery and pain control, and therefore can be considered a valid alternative for high-load bone fractures with compromised soft tissue conditions, given that it is fixed with plating system to gain extra stability.