Background: Sesamoid fractures result in significant pain and poor biomechanics, which can ultimately hinder athletic performance and delay return to sport. Current literature describes the utility of platelet rich plasma (PRP) in treating various musculoskeletal injuries, but there is minimal data regarding its application in sesamoid pathology.
Methods: We present three cases of sesamoid fracture in young adult athletes who were treated with PRP, administered via an ultrasound-guided dorsal injection approach.
Results: All patients experienced a clinically significant improvement in pain and were able to resume their previous activities.
Conclusions: The results provide compelling evidence for PRP as an effective yet minimally-invasive treatment for improving pain, optimizing recovery, and facilitating return to sport in athletes with sesamoid fractures. This case series also proposes a dorsal injection technique as a novel approach to administering treatment, which serves as a safe and effective alternative to plantar injection.
Athletic injuries, Sesamoid fracture, Platelet rich plasma, Dorsal injection approach, Return to sport
The hallux sesamoid complex plays an integral role in the biomechanics of the first metatarsophalangeal (MTP) joint and athletic performance. The sesamoid bones are subject to significant mechanical stresses, resulting in high-risk injuries including stress fractures [1]. Strong evidence has emerged supporting orthobiologics such as platelet rich plasma (PRP) for a variety of musculoskeletal conditions, but research regarding foot and ankle disorders is lacking [2].
To our knowledge, this study is the first of its kind to investigate the efficacy of PRP for sesamoid fractures. We describe three cases of sesamoid fracture in young adult athletes who received PRP at the first MTP joint via an ultrasound-guided dorsal injection approach (Figure 1).
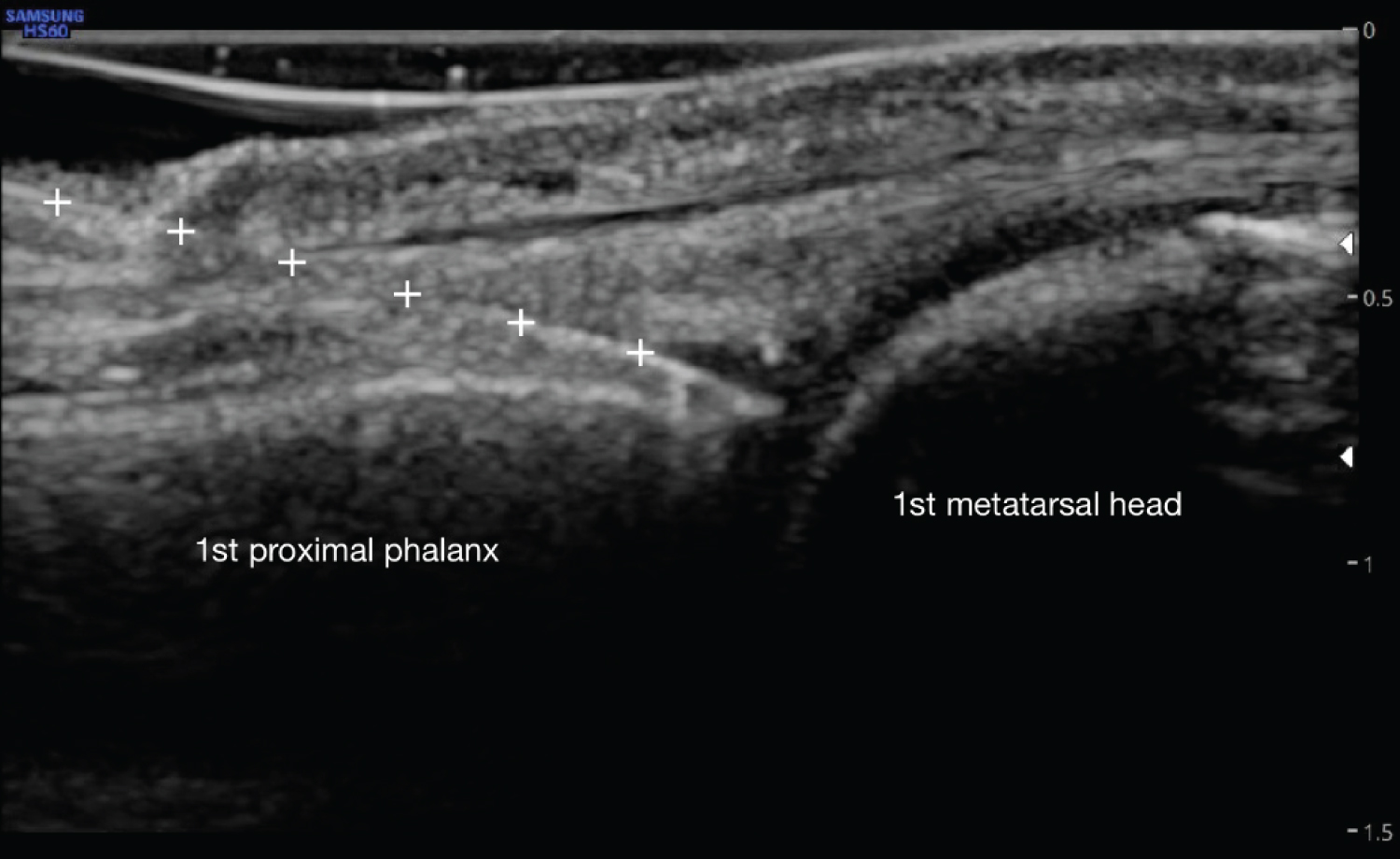 Figure 1: PRP injection to 1st MTP joint via dorsal in plane approach. White '+' signs indicate needle with tip visualized in the joint space. View Figure 1
Figure 1: PRP injection to 1st MTP joint via dorsal in plane approach. White '+' signs indicate needle with tip visualized in the joint space. View Figure 1
Instructions were provided to all patients before and after PRP injection (Figure 2).
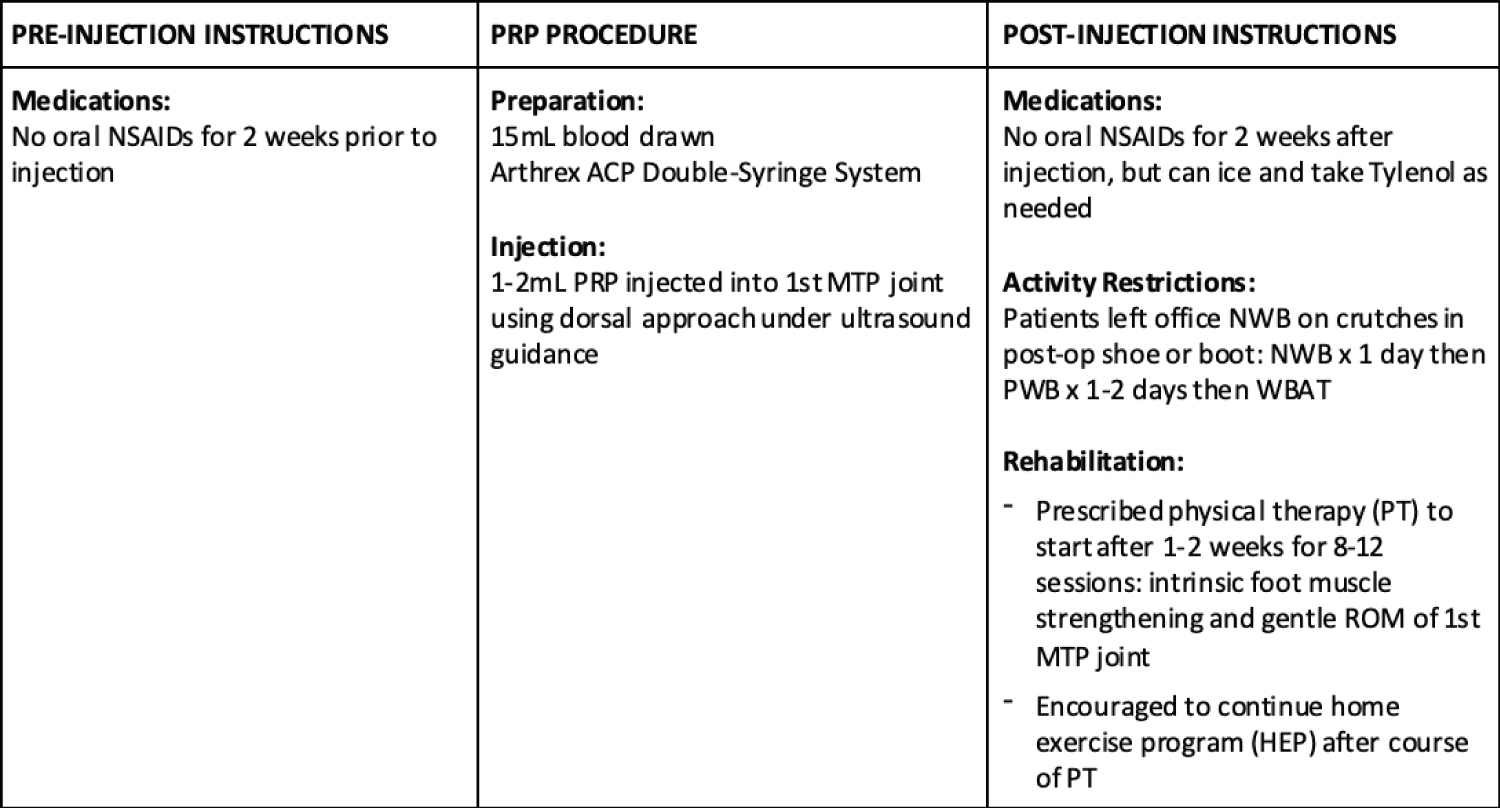 Figure 2: Patient instructions and treatment procedure. View Figure 2
Figure 2: Patient instructions and treatment procedure. View Figure 2
A 20-year-old female dancer presented with pain under her first MTP joint. Pain began eight months prior, after she dragged her toe on the ground while dancing. The pain was 7/10, exacerbated by dancing. She wore a walking boot for one month and had three rounds of shockwave therapy to no relief. Physical exam of the first MTP joint revealed pain-limited range of motion (ROM) and tenderness at the joint and flexor hallucis longus (FHL) tendon. Strength was full. X-rays revealed medial sesamoid fracture. MRI demonstrated sprains of the medial sesamoid-phalangeal and collateral ligaments of the first MTP joint, medial hallux sesamoid stress reaction, and reactive synovitis (Figure 3).
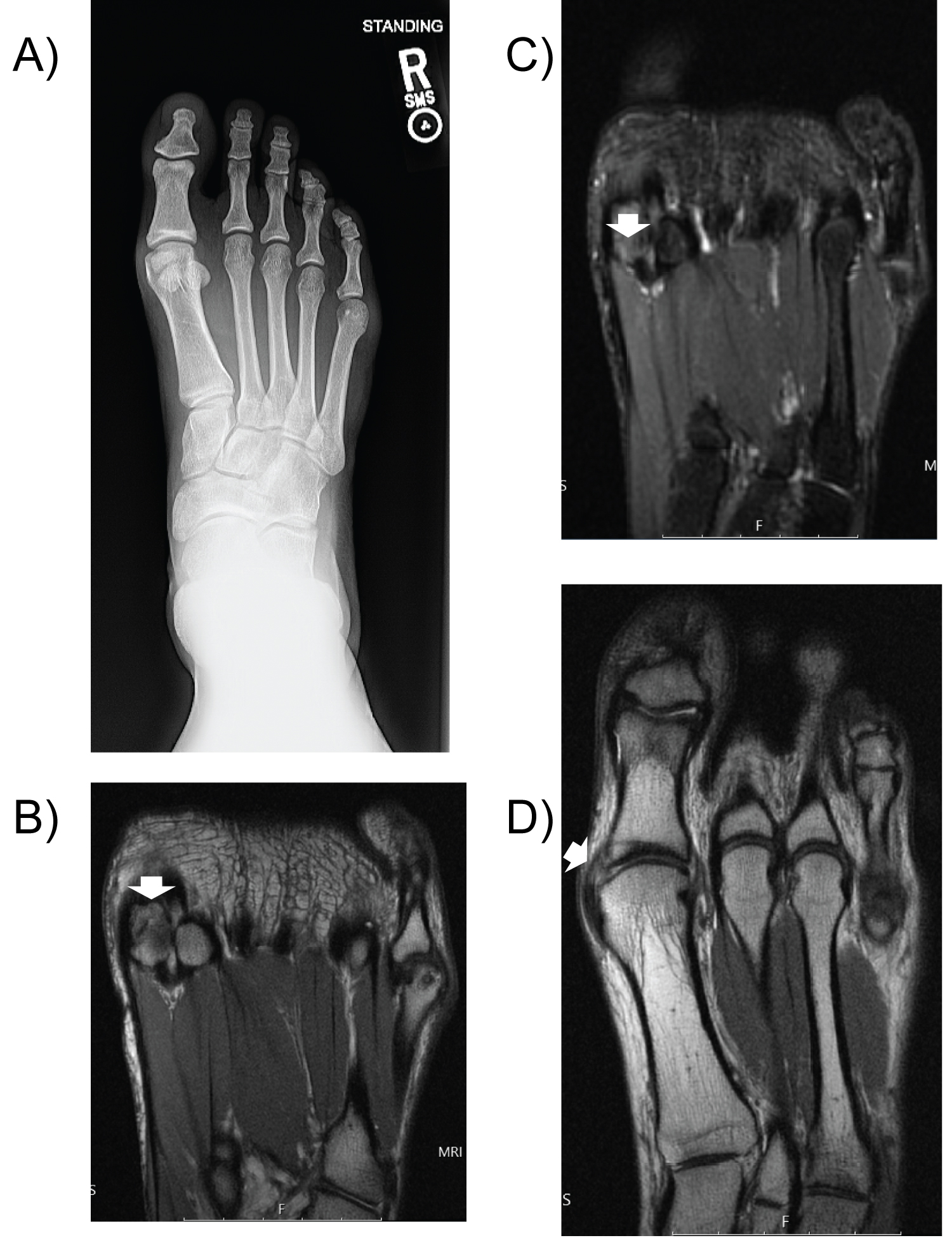 Figure 3: Case One a) X-ray AP of right foot demonstrates medial sesamoid fracture; b) MRI of right forefoot (coronal proton density sequence) demonstrates medial sesamoid fracture (arrow); c) MRI of right forefoot (coronal inversion recovery sequence) demonstrates medial sesamoid fracture with edema (arrow); d) MRI of right forefoot (coronal proton density sequence) demonstrates medial collateral ligament sprain (arrow). View Figure 3
Figure 3: Case One a) X-ray AP of right foot demonstrates medial sesamoid fracture; b) MRI of right forefoot (coronal proton density sequence) demonstrates medial sesamoid fracture (arrow); c) MRI of right forefoot (coronal inversion recovery sequence) demonstrates medial sesamoid fracture with edema (arrow); d) MRI of right forefoot (coronal proton density sequence) demonstrates medial collateral ligament sprain (arrow). View Figure 3
After PRP injection, she completed physical therapy (PT) and a regular home exercise program (HEP). At five week follow up, she reported decreased pain. She had 40-50% improvement after 10 months, followed by complete resolution of sesamoid pain by 12 months, allowing her return to dance.
A 20-year-old male runner presented with first MTP joint pain after running nine weeks prior. The pain was 7/10, exacerbated by standing and running. Pain persisted despite rest, heat/ice, NSAIDs, and immobilization in a boot for 2-3 weeks before transitioning to rocker-bottom running shoes. Exam demonstrated tenderness at the sesamoids and flexor hallucis brevis (FHB), full and painless ROM, and full strength. X-rays showed lateral sesamoid deformity. MRI revealed incomplete fracture of the lateral sesamoid and associated synovitis (Figure 4).
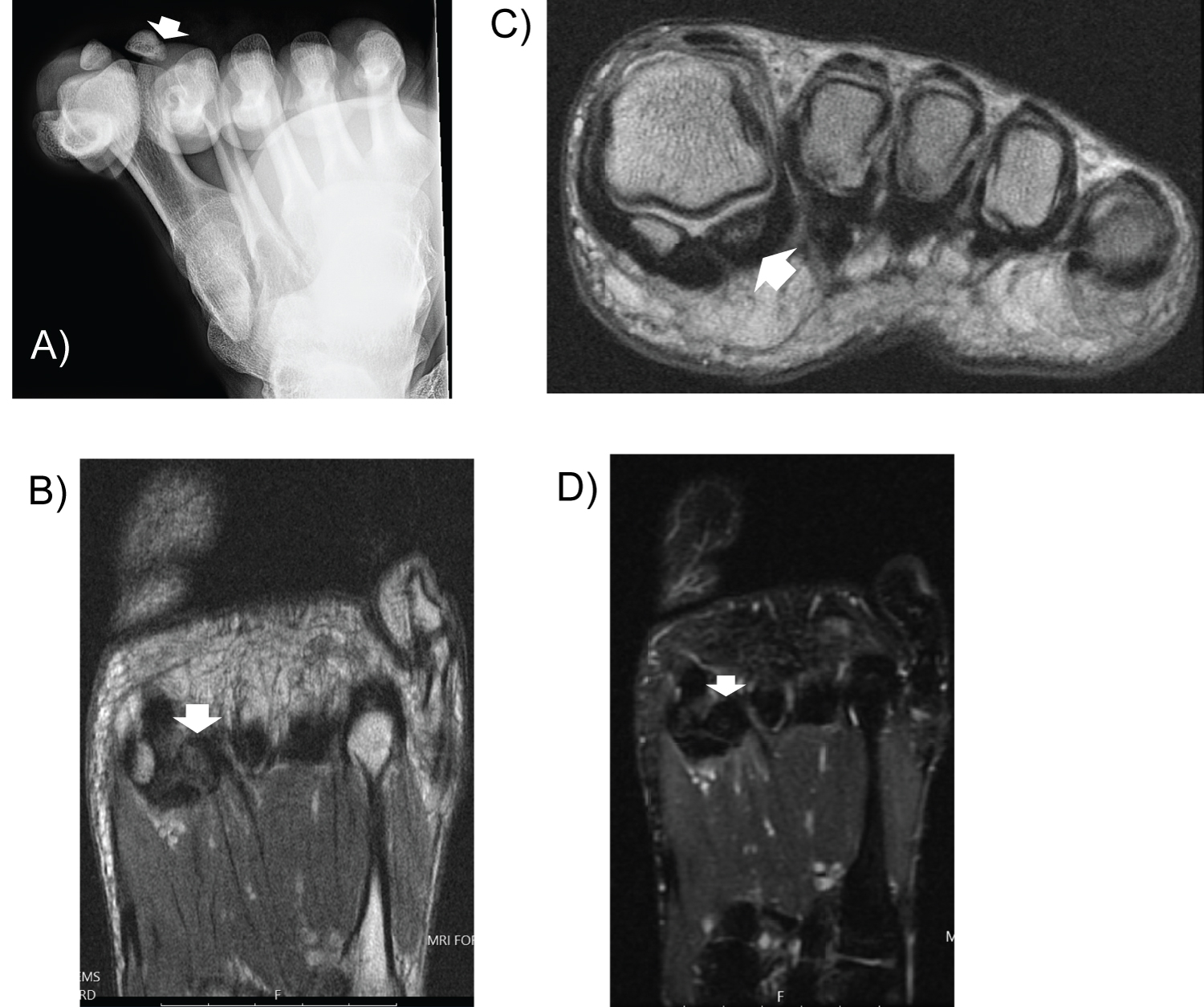 Figure 4: Case Two. a) X-rays of the right foot (sesamoid view) demonstrates cortical irregularity at lateral sesamoid (arrow). MRI of right forefoot (proton density sequence) demonstrates cortical irregularity in lateral sesamoid suspicious for nondisplaced incomplete fracture as seen on coronal (b) and axial (c) views (arrows). D) MRI of right foot (inversion recovery sequence) demonstrates trace edema within the sesamoid (arrow). View Figure 4
Figure 4: Case Two. a) X-rays of the right foot (sesamoid view) demonstrates cortical irregularity at lateral sesamoid (arrow). MRI of right forefoot (proton density sequence) demonstrates cortical irregularity in lateral sesamoid suspicious for nondisplaced incomplete fracture as seen on coronal (b) and axial (c) views (arrows). D) MRI of right foot (inversion recovery sequence) demonstrates trace edema within the sesamoid (arrow). View Figure 4
Six weeks after PRP injection, he had completed PT with consistent HEP. He reported 80% improvement in pain. At one year follow up, he endorsed 100% improvement and returned to hiking and running without pain or functional limitations.
A 19-year-old male squash player presented with first MTP joint pain that began while playing squash two years prior. The pain was rated 4/10, exacerbated by kneeling, walking, and running. He obtained custom orthotics to no relief. Exam revealed tenderness at the medial sesamoid and FHB, full and painless ROM, and full strength. MRI showed fracture of the medial sesamoid and associated synovitis (Figure 5).
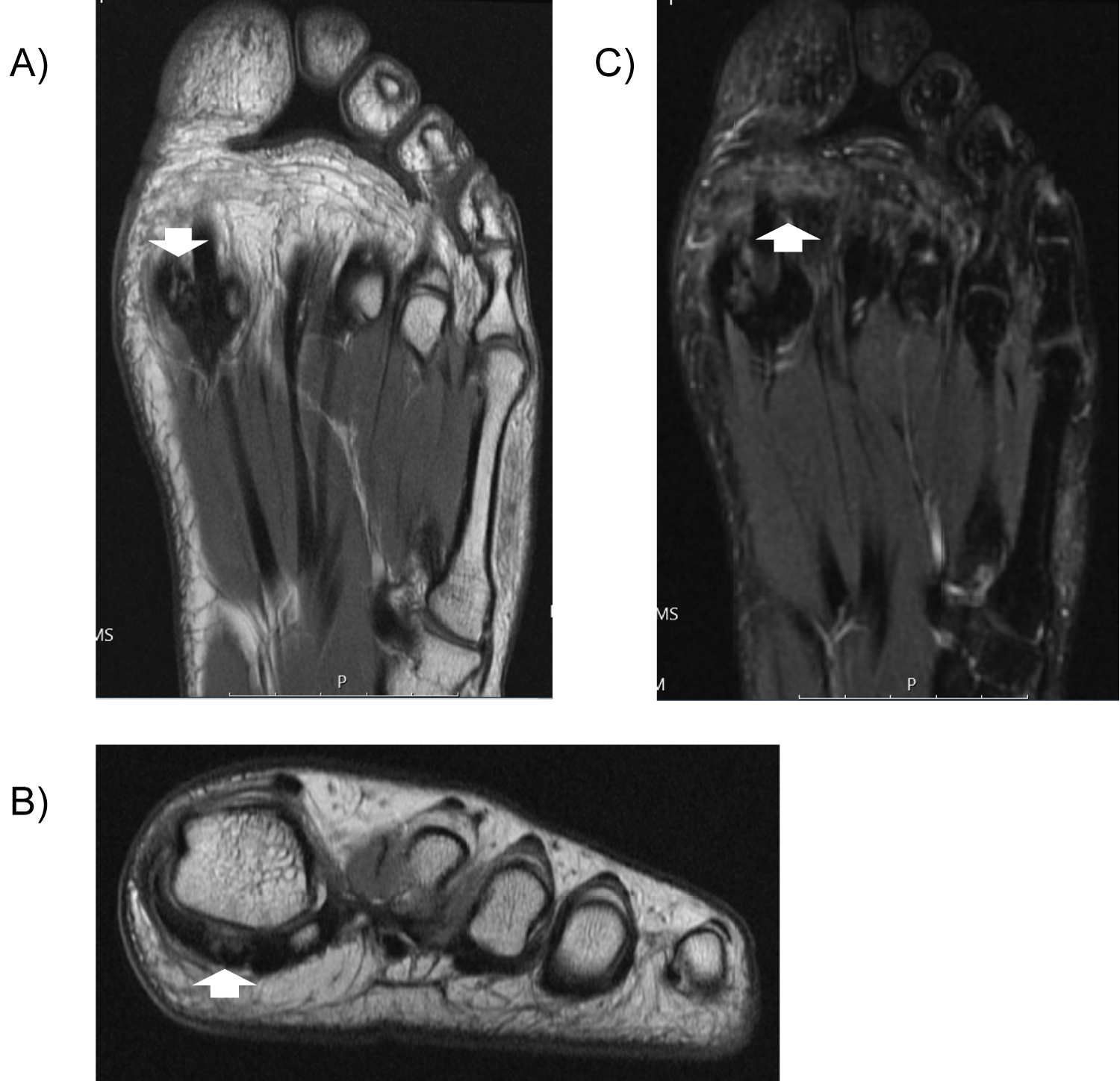 Figure 5: Case Three. MRI of the left forefoot (proton density sequence) demonstrates fracture at the medial sesamoid on coronal (a) and axial (b) views (arrows). C) MRI of the left forefoot (inversion recovery) demonstrates edema at medial sesamoid (arrow). View Figure 5
Figure 5: Case Three. MRI of the left forefoot (proton density sequence) demonstrates fracture at the medial sesamoid on coronal (a) and axial (b) views (arrows). C) MRI of the left forefoot (inversion recovery) demonstrates edema at medial sesamoid (arrow). View Figure 5
At two weeks post-injection, he reported 1/10 pain. By six month follow up, he completed PT and endorsed 60-70% improvement overall (pain-free most days but occasional monthly flares without adherence to HEP).
Sesamoid fractures are primarily found in dancers, runners, and gymnasts presenting with activity-related plantar hallux pain [3]. Standard treatment is nonoperative with rest, immobilization, and PT followed by surgical intervention if conservative treatment fails. However, studies have reported surgical complication rates up to 22% [4] and significant postoperative morbidity due to persistent pain, plantarflexion weakness, cock-up deformity, hallux misalignment, and altered joint mechanics [5]. This can have detrimental consequences on athletic performance and overall quality of life, highlighting the need for noninvasive treatment that is safe, effective, and can be implemented in a timely manner.
Although there is growing evidence for PRP in various musculoskeletal conditions, data regarding its utility in foot and ankle injuries is limited. Our literature search yielded only two systematic reviews. Vannini (2014) identified 17 studies investigating PRP in various foot and ankle pathologies, none of which included sesamoid pathology [6]. Henning (2018) further emphasized the lack of standardized PRP protocols and definitive treatment indications due to a paucity of high-quality studies [7]. Only one study has evaluated PRP in sesamoid pathology; a case series of three athletes with chronic hallux sesamoid disorders demonstrated the efficacy of leukocyte-rich PRP in facilitating return to sport following direct injection of the sesamoids under ultrasound guidance [8].
To our knowledge, our study is the first of its kind to investigate the efficacy of PRP in athletes specifically diagnosed with sesamoid fractures. Our study is unique because we used autologous conditioned plasma (ACP), which has demonstrated stronger efficacy compared to leukocyte-poor (LP) and leukocyte-rich (LR) PRP in OA [9]. Another novel aspect is our implementation of a dorsal injection technique. The direct plantar approach is most common, but has been described as technically challenging and is associated with increased discomfort and higher risk of iatrogenic tendon injury [10]. According to a cadaveric investigation by Mayo Clinic, dorsal injection of the first MTP joint accurately targets the metatarsosesamoid articulations to deliver treatment to the injured area successfully [10]. Based on these positive findings, we propose that PRP delivered via a dorsal injection approach can serve as a safe and effective alternative to plantar injection. Furthermore, this method offers a less painful injection experience and may ultimately be a preferable option for patients seeking treatment.
One limitation of this study was that we did not obtain repeat imaging studies following treatment. Given that all patients continued to experience gradual improvement in symptoms, it was not clinically necessary to have patients return to clinic for follow-up imaging. However, a future prospective cohort study could consider including post-intervention imaging to assess for radiologic evidence as an objective measure of fracture healing following treatment.
In this case-series, all patient experienced a clinically significant improvement in pain after PRP treatment, which facilitated a successful return to sport. The runner and squash player noted a substantial decrease in pain with adjunctive PT/HEP. Interestingly, the dancer initially reported less overall improvement after PRP. Of note, she was found to have associated MTP joint sprains in addition to sesamoid fracture. We suspect that a second PRP injection would have provided additional relief and enhanced recovery time.
Our results provide compelling evidence for PRP as an effective yet minimally-invasive treatment for improving pain, optimizing recovery, and facilitating return to sport in athletes with sesamoid fractures. Furthermore, our study supports utilization of a dorsal injection technique for administering PRP. A larger prospective randomized controlled trial is warranted for further investigation.