Necrotizing fasciitis (NF) is a severe, life-threatening soft tissue infection characterized by rapidly spreading necrosis of fascia and subcutaneous tissue with fulminant course and rapid fatal evolution. We present the case of a 12-year-old girl who presented with edema and redness of the left feet without any traumatic event. 48-hours later, her symptoms worsened, and sepsis developed. After a diagnosis of NF was established, surgery was immediately performed followed by plastic reconstruction. This review aims to improve understanding of the diagnosis, pathophysiology, and surgical management of this life-threatening infection, particularly in children.
Children, Early diagnosis, Necrotizing fasciitis, Surgical debridement, Superficial fasciitis
Necrotizing fasciitis (NF) is a severe form of soft tissue infection that spreads rapidly from the subcutaneous tissue and results in necrosis of the fascia and surrounding soft tissue [1]. NF is rare in children and neonates and has been reported to occur at a rate of 0.08 per 100,000 children [2]. It progresses rapidly and can lead to septic shock, organ failure, and death if not diagnosed early and treated radically [1]. We therefore summarize our experience with a 12-year-old girl with an aggressive NF of unknown origin to emphasize the paramount importance of its early suspicion and diagnosis.
A 12-year-old girl presented to her primary care physician with spontaneous pain and swelling in her left foot without a traumatic event or any skin insult. After physical examination, the patient was discharged with conservative treatment. Over the next 48 hours, she experienced increasing pain, redness, and severe swelling of the left foot accompanied by fever of 40 degrees, subsequently she was referred to our emergency department for further treatment.
On arrival, the child was somnolent, had a fever of 40 °C, was tachycardic and tachypneic. The left foot was severely tense and swollen with blue discoloration of the lateral dorsum with blistering and necrotic tissue measuring approximately 3 × 10 cm (Figure 1). Crepitation, Severe tenderness, and paresthesia were also noted at the dorsum of the lower leg and the foot. Blood work was obtained for laboratory workup and results showed a WBC of 10.58, CRP of 331 mg/L (normal 0.5 mg/L), procalcitonin of 3.52, and prothrombin time of 65%. Intravenous antibiotic therapy with cefuroxime, clindamycin and Metronidazole was initiated. Based on the clinical scenario of a rapidly progressing ascending cellulitis, necrotizing fasciitis was highly suspected, so the patient was immediately transferred to the operating room for surgical debridement. The patient subsequently underwent aggressive surgical incision and drainage. The entire necrotic tissues including skin and subcutaneous tissues were debrided until healthy margins were macroscopically seen (Figure 2). The retinaculum of the ankle was preserved to ensure approximation of the tendons to the underlying bone. Thorough irrigation of the incision sites was then followed using normal sterile saline with pulse lavage. Both aerobic and anaerobic deep soft tissue cultures were obtained, which were later found to be positive for group A β-hemolytic streptococci. After obtaining the Antibiogram, a change in the antibiotic regimen to meropenem and clindamycin was withheld.
 Figure 1: blistering and necrotic tissue measuring approximately 3 × 10 cm. View Figure 1
Figure 1: blistering and necrotic tissue measuring approximately 3 × 10 cm. View Figure 1
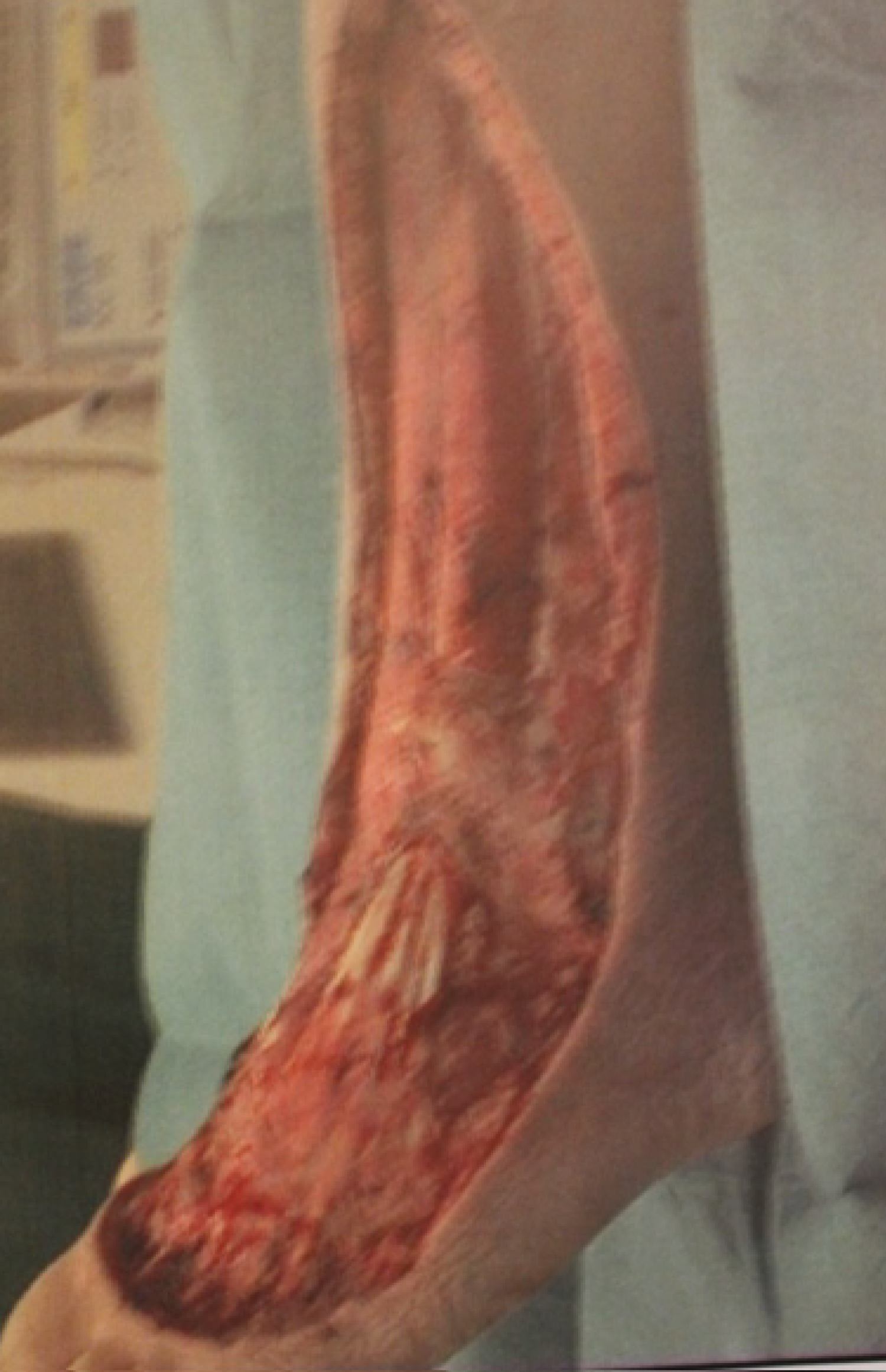 Figure 2: Local finding after wound debridement. View Figure 2
Figure 2: Local finding after wound debridement. View Figure 2
On the second day, second-look surgery with further debridement was performed. A negative pressure therapy device (Wound VAC) was applied on the fourth day postoperative and continuously maintained at 75 mmHg for 25 days. Dressing changes with negative pressure therapy were performed 3 times per week. Thirty days after the initial surgical treatment, the patient returned to the operating room for a split-thickness skin grafting: An approximately 10 cm split-thickness skin graft was harvested from the anterolateral aspect of the ipsilateral thigh with a dermatome, which covered the lateral dorsum of the foot as well as the defect in the proximal lower leg (Figure 3). By the fifth postoperative day, the primary split-thickness skin graft was completely ingrown on the entire left lower leg, ankle, and foot, with no signs of infection. The patient was seen weekly for dressing changes. At 60 days after the initial surgical treatment, the graft was 100% incorporated and fully recovered. A follow-up examination 10 years after the incident revealed a healed skin graft over the dorsum of the foot with preserved retinaculum and tendon function with full range of motion of the toes (Figure 4). The patient, however, reports paresthesia over the area of the graft to the dorsum of the toes. The patient is currently a soccer player, apart from the cosmetic appearance of the foot, she is satisfied with the overall situation of her left foot.
 Figure 3: plastic reconstruction with an approximately 10 cm split-thickness skin graft covering the lateral dorsum of the foot and proximal lower leg. View Figure 3
Figure 3: plastic reconstruction with an approximately 10 cm split-thickness skin graft covering the lateral dorsum of the foot and proximal lower leg. View Figure 3
 Figure 4: The follow-up examination after 10 years shows a healed skin graft with normal physiological function of the foot. View Figure 4
Figure 4: The follow-up examination after 10 years shows a healed skin graft with normal physiological function of the foot. View Figure 4
Necrotizing fasciitis is a severe multisystem disease with prominent cutaneous features that can be life-threatening if diagnosis and treatment are delayed. Inadequate treatment of NF can lead to severe morbidity and can be fatal [2]. Mortality due to sepsis, disseminated intravascular coagulation (DIC), or organ failure has been reported most frequently, especially when there is more than 48 hours between the onset of symptoms and surgical treatment [3-5]. β-hemolytic streptococci can also be the trigger of streptococcal toxic shock syndrome (STSS) with the above symptoms, which occurs in about 50% of cases in the course of NF and can lead to circulatory instability and multiple organ failure [6]. NF is more common in patients with chronic diseases, following varicella infection, and in patients who have recently undergone surgery or trauma [7,8].
Necrotizing fasciitis in children is often misdiagnosed as a simple soft tissue infection such as cellulitis, leading to a delay in treatment [2,9]. Clues suggestive of necrotizing fasciitis rather than cellulitis include severe pain out of proportion to skin findings, which is not always easy to assess in children, rapidly spreading edema, bullae formation, presence of skin discoloration, paresthesia, and necrotic tissue formation [4,10,11]. Other helpful parameters include marked leukocytosis, an elevated creatinine kinase level, and thrombocytopenia, the latter of which is considered highly specific for distinguishing necrotizing fasciitis from cellulitis [2,9], although the patient in our case had a normal platelet level during her hospitalization.
Usually, minor skin injuries or a traumatic injury are the etiological point of NF [3]. In our patients, no traumatic event or skin insult were reported. Unlike in adults, NF in the pediatric population is usually a monomicrobial infection. In addition to Streptococcus and Staphylococcus, which are the most common bacterial genera, Pseudomonas aeruginosa was the third most common single pathogen reported [1,1,9,12,13]. In our case, Group A beta-hemolytic streptococci (GAS) was isolated. The initial antibiotic must cover a broad spectrum against Gram-positive and Gram-negative aerobes and anaerobes. Rationalization of antibiotic therapy may be possible once microbiologic culture results are available [13]. Moreover, Treatment with clindamycin reduce the probability of hospital mortality by 89% in patients with NF as it is considered a potent suppressor of bacterial toxin production [12,14].
Early and comprehensive surgical debridement is a widely accepted clinical approach and the mainstay of effective treatment because it offers the best chance of survival in children and neonates [2]. The goals of surgical intervention should include a full-thickness incision down to the muscle fascia to removal of all necrotic tissues, including muscle, fascia, and skin, to control aggressive disease progression and the continuous release of bacterial toxins [5,14]. The retinaculum of the ankle functions as a pulley system and is an important source of neurological receptors responsible for balance and proprioception [10]. In our case, preservation of the retinacula provided an additional supportive role in the stabilization of the long tendons of the ankle.
The wound should be frequently re-examined both at the bedside and in the operating room [5]. Early coverage of large wounds with split thickness skin grafting (STSG) prevents wound infections, reduces protein loss, and helps maintain a positive nitrogen balance [5]. In our case, split-thickness skin grafting was performed 30 days after the initial surgery and regular wound care along with intravenous antibiotics to ensure a hostile tissue for the transplant.
Necrotizing fasciitis usually presents as rapidly spreading erythema, swelling, and significant pain. Early recognition is complicated by the difficulty in distinguishing it from other less serious soft tissue infections such as cellulitis, which presents with similar findings of redness, swelling, and pain. Although NF is very rare in children, it should be considered in a rapidly deteriorating child. In addition to broad-spectrum antibiotics, an aggressive surgical approach may be required, despite the risk of a disfiguring defect, to adequately clear the infection and provide the best chance of survival.