The primary aim of this study is to evaluate preoperative risk factors and postoperative outcomes in patients that underwent Charcot neuroarthropathy realignment arthrodesis, specifically in those with a fractured plantar calcaneal cortex compared to those with intact plantar calcaneal cortex, at the time of reconstructive surgery. The secondary aim was to compare the same factors in patients that underwent tibiotalocalcaneal arthrodesis with intramedullary nailing comparing if the plantar calcaneal cortex was fractured. A total of 80 patients with hind foot Charcot Neuroarthopathy were assessed with a mean follow-up of 2.23 ± 2.47 years (range 0.03 to 12.64). Bivariate analysis comparing patients with and without fractured plantar calcaneal cortices found that patients with intact calcaneal cortices had statistically higher rates of revisional surgery when compared to fractured plantar calcaneal cortices (p = 0.0264). In patients that underwent intramedullary nailing, there were no statistically significant factors between those with and without fractured plantar calcaneal cortices (p = 0.6121). The results of this study suggest that fracturing of the plantar calcaneal cortices does not have a negative effect on outcomes and should not be a contra-indication to reconstructive surgery of the lower extremity.
Ankle charcot, Calcaneal fracture, Calcaneal weight bearing surface, Intramedullary nailing, Tibiotalocalcaneal arthrodesis
Charcot deformity affects the rearfoot and ankle less often than the midfoot, but the resultant deformities are typically more severe and difficult to stabilize [1,2]. The instability in the ankle leads to a limb-threatening deformity, and surgical intervention may be necessary. The ultimate goal of treatment is to achieve a stable, plantigrade foot [3,4]. This can be very challenging as Charcot neuroarthropathy is a progressive and destructive inflammatory process with typical findings of osteopenia, osseous destruction, and periarticular fracturing [5-7]. Additionally, in patients with Charcot neuroarthropathy, bone mineral density has been demonstrated to be reduced when compared to nondiabetic controls [8-11]. This has been noted specifically in the calcaneus with chronic Charcot exhibiting a significantly lower calcaneal BMD, and acute Charcot demonstrating increased bone turnover [12,13].
When undergoing surgical intervention, arthrodesis is the treatment of choice, but achieving a solid fusion can be challenging [14]. Complications are common in patients undergoing Charcot reconstruction of the ankle and hindfoot. Complication rates have been reported to be as high as 43% in patients with diabetes who underwent TTC arthrodesis [13,15]. A recent 2021 systematic review found that CN reconstruction at the hindfoot was found to be 3.3 times more likely to undergo amputation when compared to midfoot reconstruction [16].
Furthermore, there are differing opinions on the optimal type of fixation to increase union-rate and decrease risk of complications. The options for stabilization of the Charcot ankle include internal and external fixation. Internal fixation devices include plate-screw fixation, screw/beam fixation, and retrograde intramedullary (IM) nails. External fixation is more commonly used for complicated cases such as those with wounds, osteomyelitis, deformity that cannot undergo acute correction or when there is inadequate bone mass for internal fixation [17].
It can be difficult to determine the optimal type of fixation when extensive bone loss, local metabolic dissolution, and osteopenia are present [6,18]. The primary aim of this study is to evaluate the effect of disrupted calcaneal plantar cortices on ankle Charcot neuroarthropathy surgical outcomes. The secondary aim is to evaluate the effect of disrupted calcaneal plantar cortices on ankle Charcot neuroarthropathy surgical outcomes treated with intramedullary nailing.
The study was approved by Medstar Georgetown University Hospital and the University of Maryland School of Medicine Institutional Review Board and Ethical Committee. The patients were identified using the Current Procedural Terminology (CPT) codes 20692, 28730, 28606, 28615, 28730, 28735, and 28740 queried from the records of the senior authors (CEA, CZ, JSS, JW and PJK), over the timeline of January 1, 2004, to May 1, 2020. The medical records were reviewed for demographic data, preoperative risk factors, postoperative complications, and clinical and radiographic outcomes.
Inclusion criteria included patients 18 years or older with the diagnosis of ankle Charcot neuroarthropathy who underwent Charcot realignment arthrodesis of the hindfoot or ankle. The diagnosis of ankle Charcot neuroarthropathy was identified by osseous fracturing, joint subluxation, and dislocation, in conjunction with peripheral neuropathy. Exclusion criteria included if surgical reconstruction only included soft tissue repair, exostectomy, and those with prior partial calcanectomies. Exclusion of these patients allowed for consistent evaluation post-outcomes. After the aforementioned inclusion and exclusion criteria were applied, 80 patients were identified with ankle Charcot neuroarthropathy that underwent reconstructive surgery, with a mean follow-up of 2.23 ± 2.47 years (range 0.03 to 12.64).
Demographic data collection included the following: age, body mass index (kg/m2), glycosylated hemoglobin A1 concentration (HbA1C), diabetes mellitus (DM), hypertension (HTN), gender, renal disease, chronic kidney disease (CKD defined as glomerular filtration rate < 62), end-stage renal disease (ESRD defined as glomerular filtration rate < 15), peripheral arterial disease (defined as non-palpable pulses, Doppler exam with mono- or biphasic signals, ankle brachial index < 0.9, and toe brachial index < 0.7, and/or less than three vessel run-off by angiography), and smoking history (current or former).
Pre-operative radiographs of the lower extremity were obtained as part of a standard workup for all patients for which surgical reconstruction was considered. Cross sectional imaging such as computed tomography or magnetic resonance imaging was not utilized for assessment in this study. Pre-operative lateral radiographs were independently reviewed by two physicians (AM, KM) to assess if subjectively the plantar calcaneal cortex was intact.
The cortex was defined as "intact" if the plantar aspect of the calcaneus had visible uniform bone on radiograph. The cortex was absent of fracturing and cortical dissolution (Figure 1). The cortex was deemed "not-intact" if the plantar calcaneal cortex had radiographically visible fracturing or fragmentation of the cortical bone (Figure 2). If there was discrepancy between the two independent physicians, a third physician (NC) evaluated the radiographs to determine if the plantar calcaneal cortex was intact.
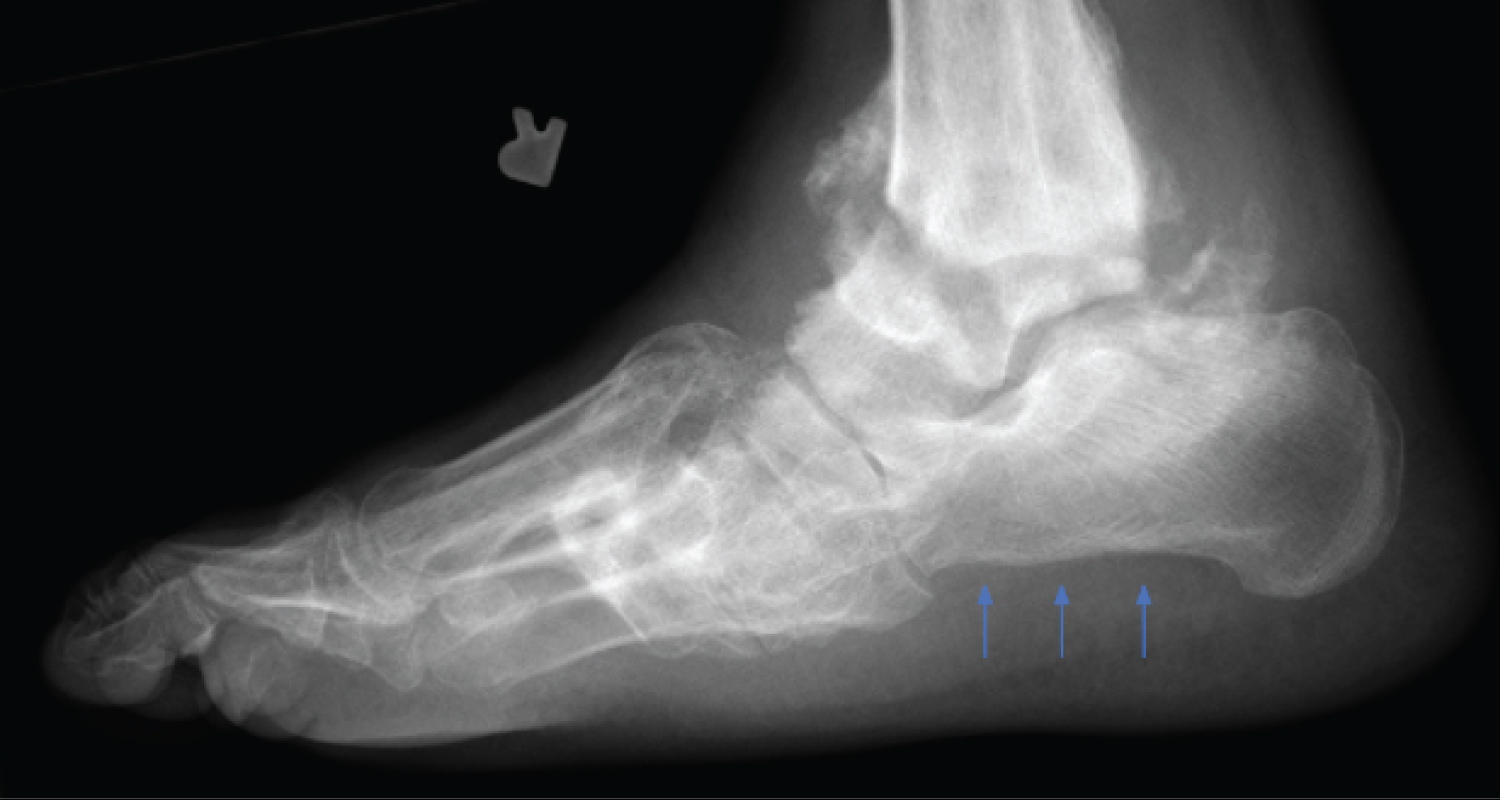 Figure 1: Example radiograph of a patient with Charcot destructive processes with an intact calcaneal cortices. Arrows indicate undisrupted plantar calcaneal cotices. View Figure 1
Figure 1: Example radiograph of a patient with Charcot destructive processes with an intact calcaneal cortices. Arrows indicate undisrupted plantar calcaneal cotices. View Figure 1
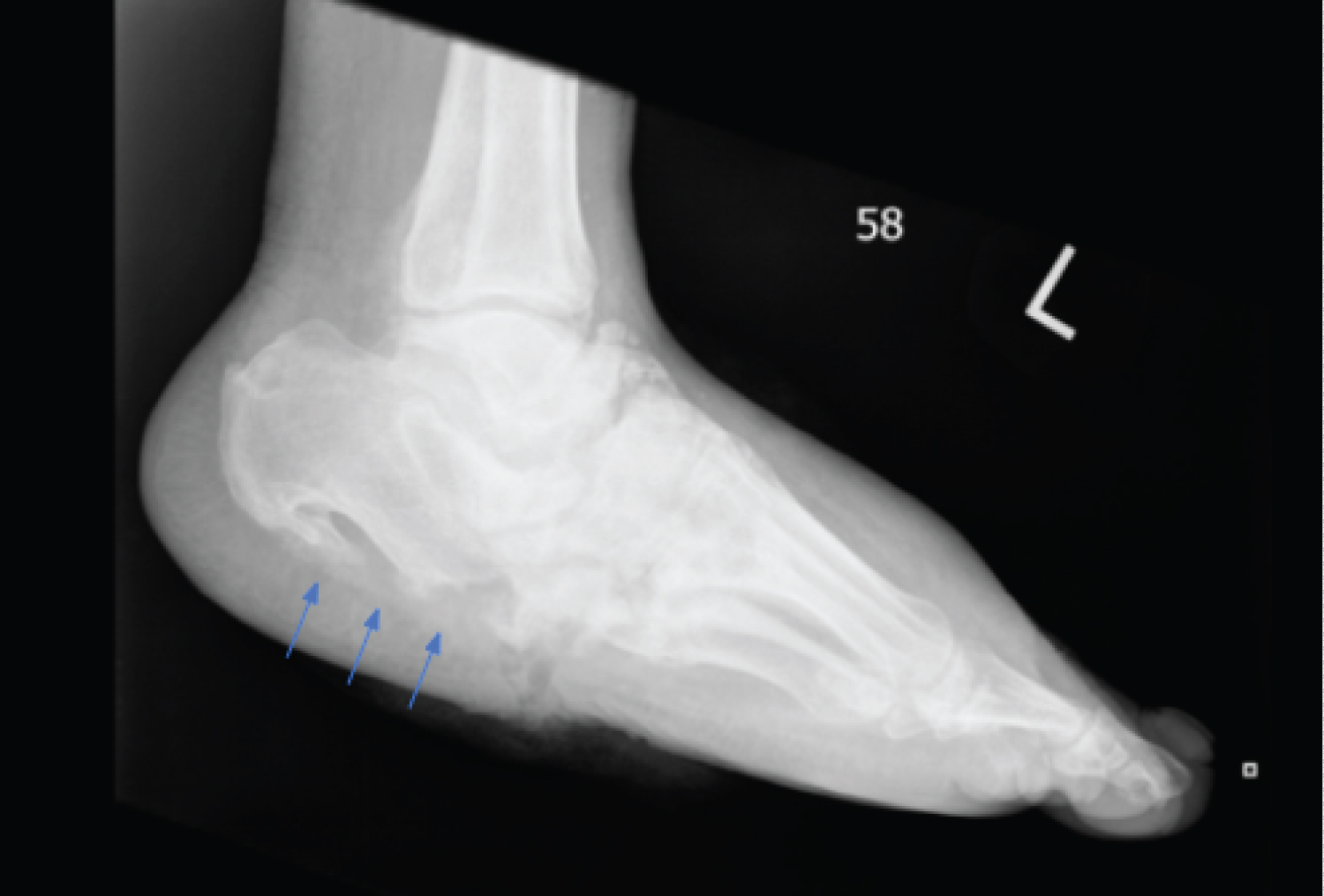 Figure 2: Example radiograph of Charcot destructive processes with a fractured calcaneal cortices. Arrows indicate disruption in plantar calcaneal cotices. View Figure 2
Figure 2: Example radiograph of Charcot destructive processes with a fractured calcaneal cortices. Arrows indicate disruption in plantar calcaneal cotices. View Figure 2
The following orthopedic hardware constructs for hindfoot fusion were identified and included: tibiotalocalcaneal arthrodesis, tibiocalcaneal arthrodesis, tibiotalar arthrodesis, and pantalar arthrodesis. The type of hardware used included solely external fixation, solely internal fixation, or a hybrid construct of internal and external fixation. External fixation consisted of a static multiplanar circular frame. Internal fixation included screws, plates, and intramedullary nails. Additionally, it was noted if adjunctive autograft or allograft was utilized. Postoperative outcomes included development of osteomyelitis (defined as culture positive bone biopsy, with or without histological corroboration), surgical site dehiscence (defined as greater than 30 days non-healing of surgical incisions), surgical site infection (defined as cellulitis, or abscess at surgical incisions), new or recurrent Charcot collapse (radiographically defined as occurring at a different site and same site as the preoperative Charcot collapse respectively), malunion/ nonunion (malunion defined as radiographic alteration in bone morphology differing from the index procedure; nonunion defined as radiographic lack of trabecular bridging at > 2 cortices across the arthrodesis site, for a duration greater than 3 months postoperatively), tibial fracture, new or recurrent ulceration (defined as occurring at a different site and same site as the preoperative ulceration respectively), the need for revisional arthrodesis, and time to revisional surgery. Preoperative wound healing and time to wound healing, progression to major lower extremity amputation and time to amputation [defined as below the knee amputation (BKA) and above the knee amputation (AKA)], and death with time to death from index procedure were assessed. The time to external fixation removal was evaluated, and if the external fixator was removed early secondary to infection or hardware failure this was noted. Other hardware complications assessed included external fixator pin tract infection, hardware breakage or failure (breakage was defined as hardware destruction necessitating removal; failure was defined as hardware breakage resulting in loss of reduction and alignment), removal of internal hardware. The above factors were evaluated using bivariate analysis to compare patients with and without plantar calcaneal cortices fracturing. Subanalysis compared outcomes in solely patients that had intramedullary nail hindfoot arthrodesis between patients with and without plantar calcaneal cortices fracturing.
Summary statistics including means, medians, standard deviations, proportions (if categorical) on all characteristics were obtained for the overall sample and by study groups. Two sample t-test ANOVA were used to examine differences in the averages of continuous variables between two groups when normality assumption was satisfied, and Wilcoxon rank sum test and Kruskal-Wallis test were used examine differences in the averages of continuous variables between two groups when normality assumption was not satisfied. Linear regression was used to examine the relationship between Survey Scores. Statistical significance is defined as p-values less than or equal to 0.05. Statistical Analysis System software version 9.4 (SAS Institute Inc., Cary, NC, USA) was used to perform the analysis.
A total of 80 patients with hindfoot Charcot neuroarthropathy were assessed with a mean follow-up of 2.23 ± 2.47 years (0.03-12.64). Demographic data for the 80 patients with ankle Charcot that underwent Charcot reconstructive surgery is on table 1. The patient mean follow-up was 2.2 ± 2.5 years (range 0.03 to 12.6). The mean age was 54.0 ± 12.3 years (range 27 to 86), with 55% (44/80) male and 45% (36/80) female patients. The mean body mass index was 35.8 ± 9.1 kg/m2 (19.0-67.0), the mean glycosylated hemoglobin A1c was 7.8 ± 2.4 (3.5-15). The prevalence of associated comorbidities was diabetes mellitus 92.5% (74), hypertension 75% (60), renal disease 36.3% (29), peripheral arterial disease 28.8% (23), and smoking history 12.5% (10).
Bivariate analysis comparing patients with and without plantar calcaneal cortices fracturing found that patients with intact calcaneal cortices had statistically significant higher rates of revisional surgery compared to fractured plantar calcaneal cortices, p = 0.0264 (Table 2). In patients that underwent intramedullary nailing, there were no statistically significant factors between those with and without fractured plantar calcaneal cortices, p = 0.6121 (Table 3).
Table 1: Demographic data of all ankle Charcot patients that underwent reconstruction. View Table 1
Table 2: Bivariate analysis in ankle Charcot patients that underwent reconstruction comparing patients with and without intact plantar calcaneal cortices. View Table 2
Table 3: Bivariate analysis in ankle Charcot patients that underwent reconstruction with intramedullary nailing for tibiotalocalcaneal arthrodesis comparing patients with and without intact plantar calcaneal cortices. View Table 3
Hindfoot and ankle Charcot realignment arthrodesis represents a challenging prognosis. To date, evidence-based medicine has been lacking in this area, and differing opinions on choice of fixation as well as technique are numerous. Typical fixation options include retrograde hindfoot arthrodesis intramedullary nail, retrograde plantar screw supplemented with an oblique screw, plate fixation, and external fixation either solely or in combination with the aforementioned internal fixation. Often, those with significant disruption of the plantar calcaneal cortex were precluded from hindfoot arthrodesis intramedullary nailing, given concern for lack of distal fixation and cortical strut. The purpose of this study is to elucidate whether fracturing of the plantar calcaneal cortex influences surgical outcomes and the outcomes of ankle Charcot reconstruction.
Charcot neuroarthropathy with ankle involvement has been associated with a high complication rate and risk for failure when compared with midfoot Charcot [3,16,19]. Choice of fixation is debated, however multiple studies have demonstrated a higher rate of union with intramedullary fixation when compared to external fixation [20,21], albeit with a higher revision and complication rate [20-22]. Within our cohort, when comparing intact plantar calcaneal cortex versus fractured, those with an intact plantar calcaneal cortex had higher rates of revisional arthrodesis (9/54 vs. 0/26, p = 0.0264). Despite the higher rate of revisional arthrodesis, there was no statistical difference between fixation constructs. Ankle Charcot was defined as the presence of joint subluxation or dislocation with associated intra-articular fragmentation and osseous dissolution. With ankle Charcot, the subluxation or dislocation involved the subtalar joint and/or the ankle joint, and the fracturing includes the talus, and/or calcaneus. In the case of non-fractured calcaneus, the remaining deformity included fractured talus. The authors suspect that the increased rates of revisional surgery seen for intact calcaneal cortices may be associated with the fact that these patients are undergoing fracturing of the talus instead of the calcaneus. Talar collapse necessitating talectomy is correlated with higher complications rates, and revisional surgery [23-26]. Pinzur, et al. demonstrated a staggering 55% rate of reoperation in patients requiring a talectomy [27]. Furthermore, there are substantially decreased rates of fusion with tibiocalcaneal arthrodesis compared to tibiotalocalcaneal arthrodesis, alluding to the importance of an intact talus. [21,28].
Despite the increased complexity of having a fractured plantar calcaneal cortex, our study demonstrated no significant difference in amputation rate, wound healing, in new Charcot breakdown, or hardware failure. Further, in patients that underwent intramedullary nailing, there were no statistically significant factors between those with and without fractured plantar calcaneal cortices.
Relative to other subcategories of Charcot reconstruction, there has been a paucity of published data regarding fixation treatment with large skeletal defects and fragmentation. Options can be restricted due to the limitation of anatomic location in addition to safe placement. Several authors have published on both internal and external fixation modalities with equivocal rates of success between the two groups [28-30]. The inherent processes of Charcot neuroarthropathy often subjugates patients to an increased risk of osteoporosis. This weak, osteoporotic bone is unable to endure strain while negatively affecting bone healing potential. Thus, our study aimed to determine whether disruption of the plantar calcaneal cortex, as previously thought, would negatively affect hindfoot fusion rates and orthopedic hardware complication rates, specifically with regards to hindfoot intramedullary nailing. IM nailing has the advantage of acting as an internal splint, designed to share the load of the bone [31]. Therefore, it was surprising that the IM nail did not fail when load sharing in an osteopenic, fractured calcaneus. Despite the plantar calcaneal cortex acting as a strut for an intramedullary nail, there were no statistically significant factors between those with and without intact plantar calcaneal cortices. This is supported by a recent systematic review by McCann, et al. that also reports no significant difference between the types of fixation used with ankle and hindfoot Charcot reconstruction when evaluating progression to limb amputation [16]. Many have published on the success of IM nails used in Charcot reconstructions, with fusion rates as high as 87% [32]. A fractured plantar calcaneal cortex should not be considered a contra-indication to intramedullary nailing when surgical planning.
There are limitations to be acknowledged within this study. The study was a retrospective review; therefore there are limitations in data collection and standardization of treatment protocols. The procedures were performed at two institutions by multiple surgeons. Treatment algorithms were at the discretion of the operating surgeon. Intraoperative factors such as orthopedic construct stability and bone strength were not quantitatively assessed for this study.
It should also be acknowledged that there was a more limited sample size of fractured cortices. 54 patients had intact calcaneal cortices while only 26 patients had fractured cortices. It can be inferred that this group is less commonly reconstructed due to osteoporotic, fragmented bone. Despite this uneven distribution between groups, our results reached significance. Furthermore, it would have been ideal to assess the plantar calcaneal cortex in more detail on a computed tomography scan, but this was not available on all patients. The goal of our study was to help with preoperative planning. A standard radiograph is more readily available to all physicians, and the calcaneal cortex can be easily evaluated.
Additionally, the Charcot reconstruction was performed at the discretion of the operating surgeon, and therefore there was not a uniform surgical approach for each patient. All patients included had ankle Charcot defined by fracturing and/or dislocation of the hindfoot complex, and the involvement of calcaneal fracturing was evaluated. However, there was a lack of distinction between fracturing (of the talus or distal tibia) and dislocation (of the subtalar or ankle joint) in the pathology involved with the ankle Charcot. Evaluating talar fracturing versus calcaneal fracturing, and the contribution of dislocation could shed light on the surgical outcomes and would be a potential future study. Post-operative care followed the standard of care in the surgeons practicing area with regard to positioning, compression, initiation and progression of mobilization and with non-weight bearing to the operative extremity for a minimum of 6 weeks, unless an external fixator designed to allow for weight bearing was utilized.
Prior to this study, intramedullary nailing was thought to be a relative contraindication in those with a fractured plantar calcaneal cortex. Despite its limitations, this investigation serves as a pilot study, and has demonstrated that those with a fractured plantar calcaneal cortex have comparable salvage results to intact plantar calcaneal cortex and should not be precluded from intramedullary nailing or Charcot hindfoot reconstruction.
John S. Steinberg, DPM, FACFAS, reports that he is a consultant for Integra LifeSciences. Jacob Wynes, DPM, MS, FACFAS reports that he is on the speaker's bureau of Smith & Nephew.
This study was supported by the University of Maryland School of Medicine Department of Orthopaedics, Jacob Wynes is the guarantor of the content of this manuscript. Alissa Mayer, DPM; Jonathan Furmanek, DPM; Kelly McKeon, DPM; Eshetu Tefera, MS; Nicole K. Cates, DPM, AACFAS: have no financial disclosures, commercial associations, or any other conditions posing a conflict of interest to report. John S. Steinberg, DPM, FACFAS, reports that he is a consultant for Integra LifeSciences. Jacob Wynes, DPM, MS, FACFAS reports that he is on the speaker's bureau of Smith & Nephew.