Chronic lateral ankle instability usually occurs in young athletes. It is caused by a rupture of the anterior talofibular ligament, better known as the anterior peroneal astragalus ligament (APAL). This lesion is associated with a rupture of the calcaneal fibular ligament or posterior calcaneal peroneal ligament (PCL) in 10 to 20% of cases and with the presence of chondral lesions of the talus and tibial dome in 75% of cases, the latter being caused by abnormal chronic joint hypermobility secondary to ligament ruptures. The study includes 26 patients who practice sports to a greater or lesser intensity. All of them had a diagnosis of "chronic lateral ankle instability", and were treated surgically in an integral manner, with a technique that is characterized by repairing all the lesions that make up this complex entity, unlike the traditional ones, which for the most part focus only on the repair of the APAL, ignoring the PCL and chondral lesions. Postoperatively, all cases were monitored closely for a minimum of two years, time during which the following was assessed: time of reinsertion to normal life, sports performance, and possible complications and sequelae that might arise. During the ankle arthroscopy, we found chronic synovitis in 100% of the cases and cartilage lesion in the talus and/or tibial dome in 75%. The reconstruction of the APAL was performed with a cadaveric semitendinosus tendon that was tunneled and fixed to the fibula with a titanium button and distally with a biodegradable screw to the talus and/or calcaneus. Our results were satisfactory, obtaining an average improvement of 21.4 points in the AOFAS classification and an integral reinsertion to sports in 95% of the cases, within a period that we consider was shorter than that seen with traditional techniques. This is because, with this technique, a permanent rigid immobilization is not used, allowing immediate rehabilitation and free ambulation after three weeks.
Athlete injuries, Chronic lateral ankle instability, Recurrent sprains, Integral anatomic repair
Worldwide, trauma is among the top three reasons for attention in emergency departments, reaching approximately 15% of the total of all care provided. Of these, ankle sprains are the number one, with an estimated 2 million injuries per year in the USA [1-3]. Of all ankle sprains, 15 to 20%, evolve into chronic post-traumatic lateral ankle instability due to their severity. There is a lack of exact figures of the problem in the literature [4-7].
This kind of injury is characteristic of young athletes, although any person in all stages of life can suffer it, usually of a lesser intensity than in athletes, who usually sustain high-energy traumas. Unfortunately, however, they are characterized in a considerable number of cases for the treatment of the first injury that is minimized [8], reintegrating individuals to their sport practice and to their daily activities in lapses ranging from one to three weeks, without close monitoring and without a thorough assessment of the severity of the lesion [9-13].
The usual outcome of an insufficient initial treatment of severe ankle injuries will be reflected in a lower sports performance and the presence of chronic pain and inflammation, with increasingly frequent recurrent sprains of greater intensity and with longer periods of pseudo-recovery, which can even prematurely end the sports career of elite prospects and with progressive deterioration in the quality of life of any patient who does not go to the specialist in a timely manner to receive a correct diagnosis and treatment of a chronic lateral ankle instability [8,14].
Typically, the history of the ailment in most cases is as follows: The athlete suffers an ankle sprain and goes to the specialist late [15,16] referring a strong ankle sprain of long evolution (4 to 6 months) which was initially treated superficially. The athlete restarts his/her sports activity prematurely by self-decision, which necessarily leads him/her to suffer a series of painful repetition sprains causing him/her to diminish his/her sports performance at first and subsequently making it impossible to lead a normal life due to pain, inflammation, and a feeling of instability.
The specialist corroborates the painful inflammation at the level of the fibular malleolus region, specifically at the anterior peroneal astragalus ligament (APAL) level, and always intentionally looking for joint pain secondary to synovitis and/or tibial or talar chondral injury. If there is an anterior drawer of more than 3 mm, posterior displacement of the tibia (giving away), accompanied by lateral yawning seen on the X-rays, the diagnosis of a syndrome of posttraumatic chronic lateral ankle instability can be made. In these cases, the evaluation of the deltoid ligament and a possible dislocation of the peroneal tendons, present in 5 to 7% as associated lesions, should not be omitted.
In this context and with the findings obtained on physical examination, the surgical repair would be fully justified. However, it is most convenient to complement the diagnosis with a magnetic resonance image (MRI) study, which will show the lesion of the APAL, more apparent in the transversal view and if there is also a rupture of the PCL, it will be better visualized in the coronal views, besides the visualization of chondral lesions of the talus or tibia, although these last ones are not always detectable by this means in all the cases [17].
Once the orthopedist makes the diagnosis, the disjunctive is presented on the surgical treatment to choose for the repair of the APAL and the PCL, when this is also injured, since there are several surgical techniques for the ligament repair. There are those that are primarily focused on the repair of the APAL, omitting in most cases the repair of the PCL, which provides much of the stability to the subtalar joint. If its repair is omitted it will eventually lead to osteoarthritis of that joint, which in an athlete will have catastrophic consequences [18]. In the same way, it is important to emphasize the need to attend the injuries of the cartilage of the talus and/or tibial soffit, secondary to chronic ligament instability producing an abnormal joint hypermobility.
From the above we may conclude that it is not functionally adequate to perform an incomplete treatment of all the existing problems, situation that is frequently observed with the usual techniques, confirming that there is no consensus on a specific procedure that may be considered as the gold standard to solve this problem in a comprehensive manner, as exemplified below [19].
Some non-anatomical techniques, such as those advocated by Evans and Watson-Jones for the repair of the APAL date from the '50s and more recently the Chrisman Snook technique in the '80s, use the tendon of the peroneus brevis to substitute the damaged anterior peroneal-talar ligament within them. The distal insertion in the fifth metatarsal is not modified, which disables a healthy muscle by sectioning it, besides that it causes an additional compression and imbalance in the sub-talar articulation. This situation is not recommended for athletes. In this regard there is a great detraction on these procedures because it is an open and complex surgery that requires a prolonged period of immobilization and rehabilitation, with immediate and long-term complications, highlighting the subtalar arthrosis and muscle imbalance and therefore leaving many athletes who do not return to their activity or reach their pre-injury performance [20-23].
The anatomical techniques such as the Bröstom and the Bröstom-Goul in the '80s, and one of the most used nowadays, consists of the direct repair of the torn APAL and the articular capsule, accompanied by a reinforcement with the extensor retinaculum. They both have the disadvantage of being open surgeries which does not strictly repair the frayed and retracted ligament, in addition to the fact that they do not take into account the plasty of the PCL or the chondral lesions, emphasizing that in a great number of cases, because they are chronic lesions and insufficient ligamentous remains are found which do not allow the desired plasty and therefore force to prolonged immobilizations and rehabilitations with a sport reincorporation greater than six months in the best of the cases. Also, literature reports a high percentage of relapses and long-term failures, also highlighting a decrease in sport performances caused by the change of direction and angulation of the extensor tendons of the foot that are modified when retracting the retinaculum, with the respective and inadequate biomechanical alterations that this represents [13,24-30].
A modification to this technique arises with the so-called "Internal brace", consisting in the addition to the Bröstrom technique a synthetic suture called fiber wire, which is fixed to the fibula in the emergence of the ligament, with two anchors to achieve an anatomical substitution of the same, with good results in the short term (no reports of long-term results were found). However, we are certain that the elasticity will never be the same. The resistance and biocompatibility of an allograft will never be the same as that obtained when the ligament is replaced by an artificial implant, so much so that all the ligament replacements with synthetic materials that were performed some years ago in the ACL did not have the desired results, and these techniques are practically abandoned nowadays [31].
On the other hand, most authors agree that arthroscopic repairs are complex procedures that only use sutures, providing imprecise blind reconstructions, are very labile and they do not afford an integral solution to the problem [25-28,32,33].
The anatomical and non-anatomical surgical techniques as well as the arthroscopic procedures currently used for the treatment of chronic lateral ankle instability are characterized by the fact that each of them can be improved, both in stability, repair of joint damage, immobilization time, early physiotherapy and above all, in early reincorporation to sports with a decrease in long-term sequelae.
For these reasons, we present the results obtained with a 100% anatomically minimally invasive technique that repairs all the damaged structures in post-traumatic chronic lateral ankle instability. We have been performing this procedure since 2013, consisting of an ankle arthroscopy in all cases, and then through a 3 cm incision on the body of the ligament, we safely perform the plasty of one or both injured ligaments [34].
This procedure does not require rigid immobilization for a long time in the postoperative period. By using a Walker type boot that allows immediate rehabilitation and assisted ambulation for two weeks and its definitive removal after three weeks in most cases, the number of complications are reduced allowing reintegration into work and sports in shorter periods than those required with the previously described techniques.
This is a clinical, retrospective, observational, cross-sectional study in 26 sports patients, operated with this technique, in the period from January 2013 to September 2018, with a two-year follow-up.
The age ranged from 19 to 60 years with an average of 30 years; 18 patients were male and 8 females. Five patients reported being high performance athletes (19%), 12 athletes with constant and regular sports routines (46%), most of them being soccer players in men and volleyball players and runners in the female sex, 5 with recreational practice of various sports (19%) and the remaining 4 (15%) referring irregular sports activity (Table 1).
Table 1: Study group by level of physical activity. View Table 1
The predominance of the injury was on the right side of the ankle with 16 cases and 10 on the left. The number of sprains ranged from 3 to 12, with an average of 5, and the age was from 4 months to 3 years before deciding on surgery.
The diagnosis of chronic lateral ankle instability was made by investigating the history of a severe ankle sprain and the initial treatment received, particularly assessing if it was insufficient, and by observing the predominance of diverse treatments such as bandages and immobilization with splints, orthoses, or circular devices that in most cases were not resolved in time and form, and usually placed in emergency services or private offices.
With reference to the clinical picture prior to surgery, 95% referred pain predominantly with sports and 80% noted permanent swelling of the affected ankle. In addition, the sprains took longer to recover from the time they recurred, gradually withdrawing them from their sporting and work activities with an increasing number of restrictions.
On physical examination, the inflammation and exquisite pain at the level of the injured APAL was corroborated. The anterior drawer and posterior displacement maneuver of the tibia was evident in 6 cases, more noticeable in those patients with lesion of both structures (APAL and PCL).
The dynamic radiographs in varus and valgus were not a reliable parameter for the decision to perform surgery, since it depends a lot on the cabinet, the technique used and the person performing the maneuver. The lateral yawning was clearly seen by fluoroscopy in three cases during the intra-operative period. On the other hand, MRI was inaccurate for the PCL lesion in 4 cases 15% and in 40% for the chondral lesion, so that we insist that the clinical criteria is the predominant to make the decision to operate, always recommending ankle arthroscopy [8,23].
For the pre- and postoperative clinical evaluation, we used the classification of the American Orthopedic Foot and Ankle Society (AOFAS) of the ankle, when evaluating the result according to an improvement in the scale score, as well as their reincorporation and sports performance in three groups: Group 1: Normal activity in their daily life with recovery and sports performance of 90 to 100%, Group 2: Normal activity in their daily life with recovery and sports performance between 70 to 90%, and Group 3, with normal daily activity, but with sports performance of less than 70%.
This technique is based on the hypothesis that a tendon, whether cadaveric or the patient's own, has a greater resistance and bioavailability similar to the injured ligament(s), with full capacity and sufficiency to adequately replace them by correctly absorbing the joint loads, a situation reliably demonstrated through more than 70 years, in which thousands of procedures have been performed with the peroneus brevis tendon without documented evidence of ruptures [8,9], in addition to the routine use of the semitendinosus tendon in the cruciate ligament plasty. Since the knee is a more demanding joint than the ankle, giving us the certainty that the proposed technique provides a high degree of safety and reliability [34-36].
The surgery consists of an ankle arthroscopy in all cases, using the usual portals, anteromedial and anterolateral, to intentionally look for the presence of chronic synovitis and/or chondral lesion, either of the talus or tibia, more specifically on the lateral corner of the joint, under the premise that chronic instability of the ankle will necessarily cause this type of lesions, which if not repaired will result in medium- or long-term sequelae, always performing the necessary synovectomy and chondroplasty with shaving and in three cases adding microfractures [22,24,29,31,33,37-42]. During the procedure, it is feasible to visualize and evaluate the ligament remains of the APAL, the presence of free bodies and the syndesmoses in case there is exceptional damage.
Once the arthroscopy is finished, the ischemia is placed and a 3 cm curved cutaneous incision is made where the body of the APAL is presumably located, taking care not to exceed it, since there is a risk of causing a lesion of the superficial peroneal nerves towards the front and sural behind the peroneal tendons. The traditional longitudinal incision can be used in case of not feeling safe with the recommended one (Figure 1). Through this incision the tunnels can be practiced, the proximal one towards the fibula and the distal one over the talus, with the advantage that, when performing the final reconstruction of the wound, this can be done in a similar way as described by Bröstrom.
 Figure 1: Skin incision.
View Figure 1
Figure 1: Skin incision.
View Figure 1
Simultaneously, the free cadaveric semitendinosus graft is prepared, with a minimum length of 16 cm and a diameter not less than 6-7 mm, which is folded on itself, and a strong suture is placed in the upper eyelet attached to a titanium button for fibular fixation. The two distal free ends are also placed with anchoring sutures that will serve as a guide and to provide the desired tension to the neo-ligament; the latter can be used together when only the APAL is injured or individually for the simultaneous repair of the PCL (Figure 2). In all cases we use platelet rich plasma taken from the patient to bathe the tendon graft and the excess is used to infiltrate the ankle joint.
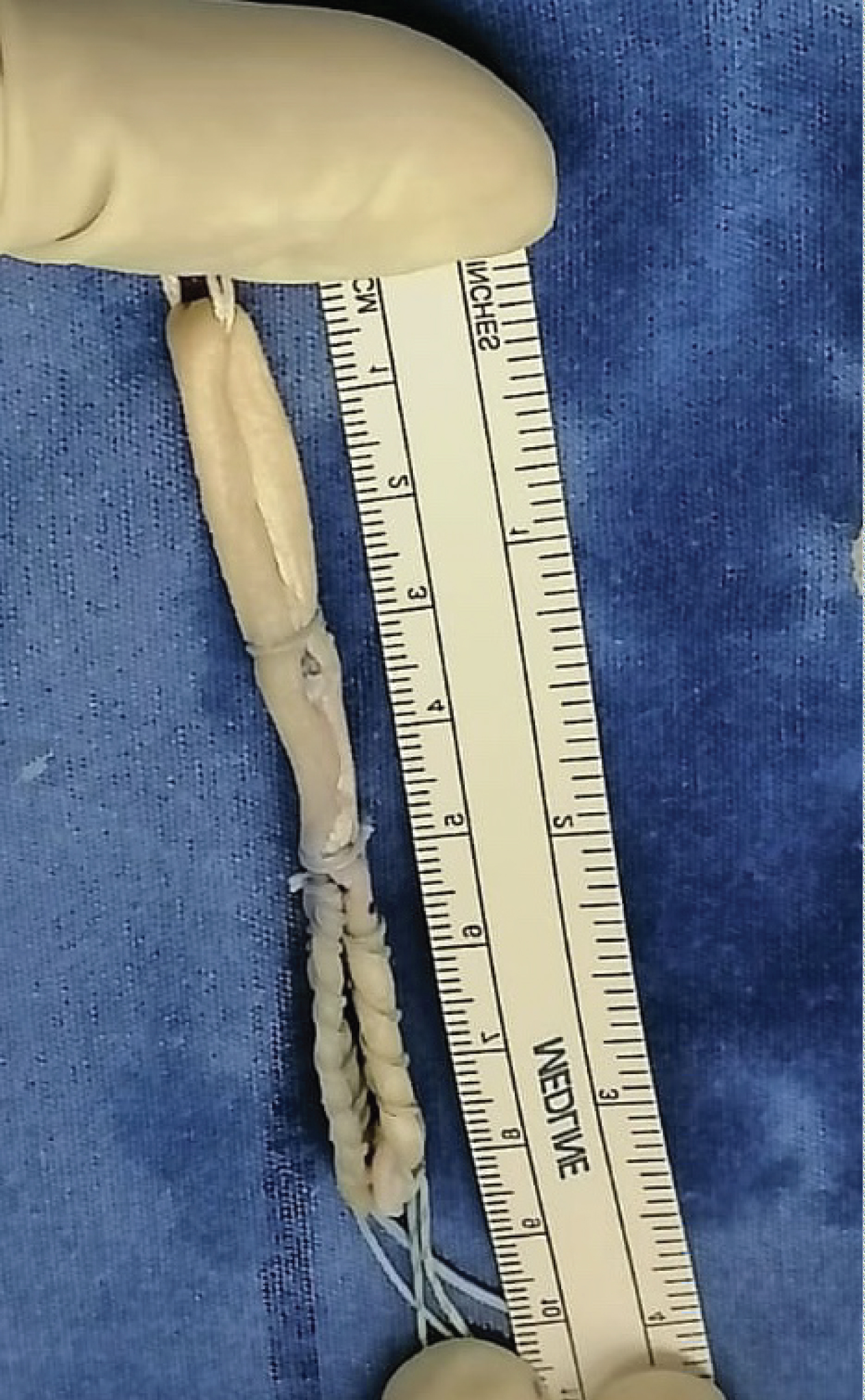 Figure 2: Graft preparation.
View Figure 2
Figure 2: Graft preparation.
View Figure 2
The proximal fixation of the allograft is performed through a fibular tunnel at the level of the APAL insertion, made with a guide that is introduced under fluoroscopic vision, from distal to proximal, with an angulation from front to back of 30 degrees and a minimum length of 3 cm. At this point, it is necessary to separate the peroneal tendons so as not to injure them with the tip of the guide as it emerges in the posterior cortex of the bone, preferably with a Hommans retractor or hemostatic forceps placed through a 0.5 cm incision. Once located, a 6 or 7 mm cannulated drill is used to make a tunnel of at least 2.5 cm long that will house the fibular portion of the free tendon. The depth of the tunnel is marked on the tendon and it is introduced by pulling the free strands up to the titanium button anchor in the posterior cortex of the fibula, in a similar way to that performed in ACL plasty with allograft.
When only the APAL is injured, the distal fixation is performed in neutral position of the ankle, directing the guide horizontally from the anatomical insertion of the ligament in the talus, crossing it from lateral to medial, to emerge 1.5 or 2 cm below the vertex of the medial malleolus. The two free ends are joined to fix them inside a tunnel of a minimum of 3 cm deep, anatomically reproducing the two fascicles that make up this ligament (Figure 3) to subsequently perform a safe tenodesis using a biodegradable screw, which guarantees a robust anatomical repair, to which a unique and valuable attribute is added, consisting in the possibility of being able to provide an adequate tension to the neo-ligament, when the sutures are pulled from the medial side of the foot manually or with the ACL tensiometer at 20 N, a situation that is impossible to perform with any of the other conventional techniques (Figure 4).
 Figure 3: Final repair of APAL both fascicles.
View Figure 3
Figure 3: Final repair of APAL both fascicles.
View Figure 3
 Figure 4: Neo-ligament tensioning and tenodesis screw placement.
View Figure 4
Figure 4: Neo-ligament tensioning and tenodesis screw placement.
View Figure 4
In case of an added injury of the PCL, the distal ends of the graft are separated, and the posterior portion will also be fixed with a biodegradable screw with distal and posterior direction in the anatomical position of the injured ligament on the calcaneus, in a tunnel of at least 3 cm in length in a similar way to the one performed in the talus, taking special care to pass the graft under the peroneal tendons [34].
In our series only 3 cases (10%) required repair of the PCL, and they were diagnosed through a meticulous examination of the ankle instead a MRI, detecting a frank anterior drawer of more than 3 mm and an evident yawning at the fluoroscopy, which is performed in the operating room, prior to the beginning of the surgery.
Then, the stability of the ankle is corroborated, and the closure is performed in the usual way with reinforcement of the capsule, as described by Bröstrom, to finish the procedure (Figure 5).
 Figure 5: X-ray view showing the surgical procedure completed.
View Figure 5
Figure 5: X-ray view showing the surgical procedure completed.
View Figure 5
Postoperative management: We use cryotherapy for a period of one week, immobilizing the joint with a Walker type boot, with partial unloading with crutches for 15 days. Since the first postoperative day the boot is removed at times to begin immediate rehabilitation. The orthosis is definitively removed after three weeks, and free walking is allowed.
Each patient underwent periodical follow-up evaluations. The progress was measured with the AOFAS classification score and with the reincorporation and performance assessment of daily and sports activities according to the three groups previously mentioned, allowing this last activity progressively from 6 weeks to four months, depending on each case.
The average AOFAS score in the preoperative period was 72.3 points out of 100 and in the postoperative period all had an average improvement of 21.4 points reaching an average score of 93.7, with a notorious decrease in pain at the end of the evaluation, with reintegration to their work and daily activities within normality in 100% of the cases at two months and for sports activities at four months on average, except for one case in which there was not a 100% recovery in relation to the previous sports performance (Figure 6).
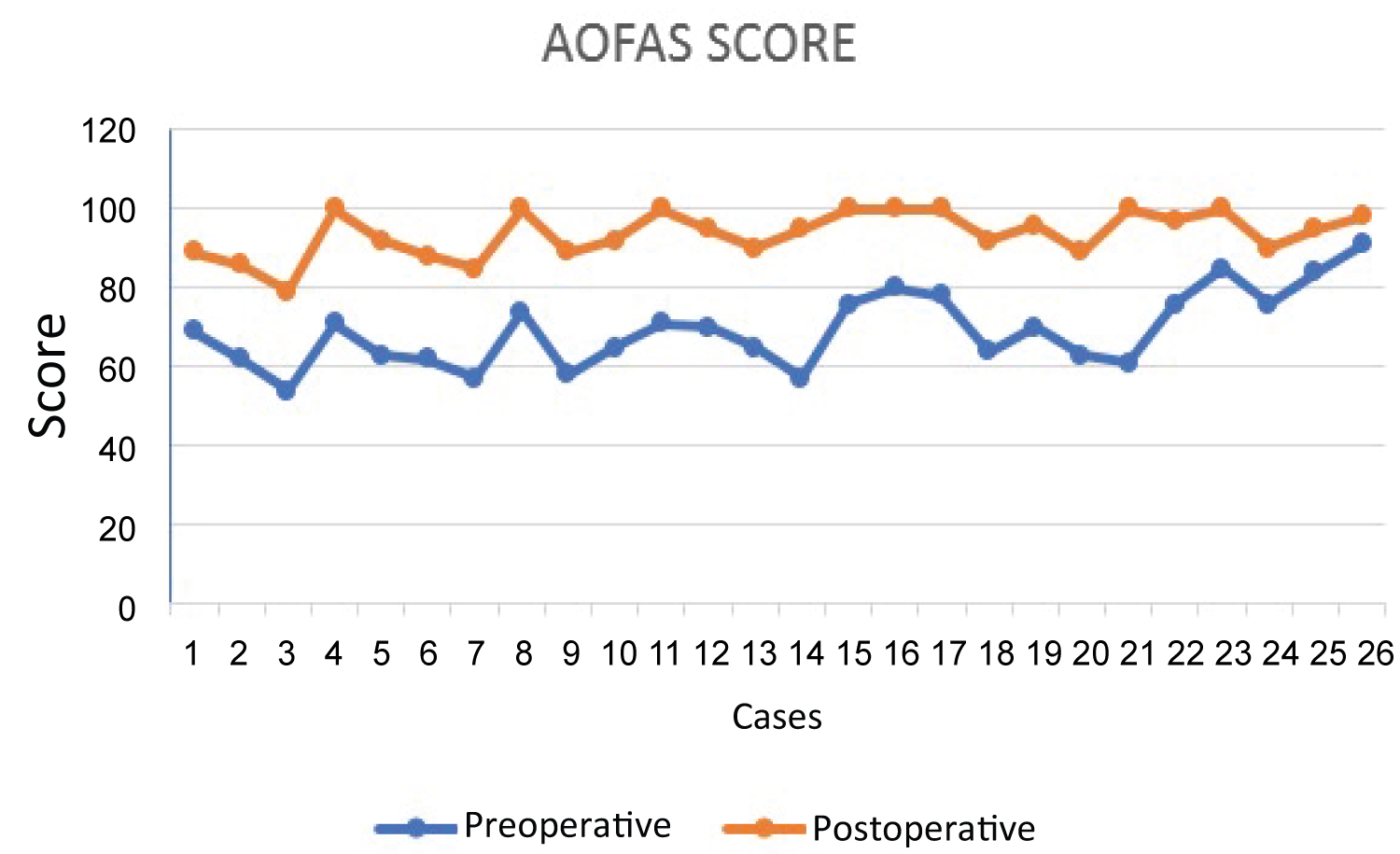 Figure 6: AOFA S score before and after surgery.
View Figure 6
Figure 6: AOFA S score before and after surgery.
View Figure 6
The high-performance athletes (marathon runner, triathlete, two soccer players and one football player) were able to resume their sports activities, noting in the first one, a 20 to 30% drop in his performance, although his daily life activities were performed normally, being considered as the only result included in Group 3, noting that he presented a chondral lesion of the talus Grade III that required microfractures. The rest of the athletes had an improvement in the AOFAS score and were included in Groups 1 and 2.
Regarding the amateur athletes with a regular and constant weekly routine the results were as follows: One gave up playing soccer by his own decision even though he did not report any discomfort when practicing it and two more spaced out their routine (Group 2). The remaining number (9 patients) resumed their life completely in all aspects (Group 1).
The group of occasional athletes were all included in Group 1 since they did not present any limitation to their usual activities (Table 2).
Table 2: Return to sports activities. View Table 2
During the arthroscopic procedure, a chondral lesion was observed in 75% of the cases, from Groups I to III in the Outerbridge classification. There was mild to severe synovitis in 100% of the cases. In all these patients a partial synovectomy and chondral repair with shaver were performed and in two cases it was complemented with microfractures [41].
Finally, we may conclude that the results were excellent in 22 patients (84.6%). In 3 cases, the outcomes were rated as good because of persistence of mild to moderate pain at the site of the intervention in 2 of them and in the other because he voluntarily suspended his sports activity (11.5%). And in another patient, the result was rated as regular, because he could not reach his previous sports performance at 100% (3.8%). It should be noted that there were no infections or wound dehiscence in the postoperative period which was explained because this is a minimally invasive procedure.
The only relevant complication occurred in the marathon runner patient who could not resume 100% of his previous sports activity and showed a 20 to 30% decrease in it. However, he did not have any functional limitations or pain while practicing minor sports activities.
During the follow-up period, there was no clinical or radiographic evidence or complaints related to subtalar arthrosis.
We consider this is a good technique because it has the advantage of being minimally invasive and anatomical, in addition to the substantive benefits it provides compared to other techniques. The safety it provides has been widely proven for many years by other authors who have used autologous or allogeneic tendon grafts [19,20].
We present a minimally invasive surgical technique that uses an autograft for the repair of chronic lateral ankle instability, following synovectomy and arthroscopic chondroplasty.
The premises for using this procedure are based on the integral correction of the elements that make up a chronic lateral ankle instability, starting with the performance of an arthroscopy in all cases, since we observed the presence of chronic synovitis in 100% of our series and chondral lesions in 75%. All these injuries were repaired during this procedure, avoiding future damage such as chronic pain and sports functional disability, both already reported in the world literature.
On the other hand, this technique recommends a minimally invasive incision of 3 cm which is wide enough to visualize both ligaments for the right and anatomical placement of the graft for the APAL plasty, with the great advantage over other techniques, that the graft can be provided with the desired tension, without omitting the plasty when the reconstruction of the PCL is necessary (ignored in most of the described techniques), having the certainty that through the years, the neo-ligament has proved to be effective enough to replace the damaged one, which is almost impossible to repair directly [8-10].
Generally, our results have been very satisfactory without any major inconveniences so far. It is an anatomical repair in which no subtalar arthrosis has been observed and the work and sports recovery is shorter compared to other techniques, since a shorter immobilization time is used in a minimally invasive anatomical technique, which translates into a lower number of complications with a solid biological repair that allows early rehabilitation and reintegration to normal life.
It is certain that we must continue with the observation of our patients to determine their long-term evolution, considering the cost of surgery versus the benefits in sports performance and the savings in recovery time, especially with regard to high-performance athletes where it could be considered as the "gold standard" for the results obtained. All this motivates us to recommend this technique as an integral, anatomical, minimally invasive procedure, with tangible results superior to several surgeries already described in the world literature for the care of these injuries that are increasingly more frequent and better diagnosed.
The authors declare not having any conflicts of interest.
There was not any external funding for the preparation of this paper.
This work was awarded 1st place in the Competition of Free Papers at the "1st International Virtual Congress of Orthopedics and Traumatology of the Mexican Federation of Colleges of Orthopedics and Traumatology AC. FEMECOT 2020".