Design developments improved outcomes of total ankle replacement (TAR), but the ankle remains difficult to replace with a prosthesis. The aim of this study is to evaluate short-term results of the Cadence Total Ankle System.
Eleven TARs were retrospectively evaluated for intraoperative complications, short-term postoperative complications, clinical outcomes and radiological outcomes.
Nine intraoperative complications occurred in 7 patients and eight short-term post-operative complications occurred in 5 patients. In total 54.5% of the patients were very satisfied with their TAR with preservation of range of motion (ROM) and clinical and radiological alignment. The pain in the first few postoperative days was mild.
This non-designer case series with our first 11 Cadence TARs shows a high complication rate, which could be caused by factors such as learning curve. However, clinical outcomes are encouraging.
Total ankle replacement, Cadence total ankle system, Complications, Radiological alignment
Total ankle replacement (TAR) is one of the surgical treatment options for end-stage ankle osteoarthritis and is gaining popularity since design developments provides improved results. However, despite design developments TAR survivorship is still low compared to total hip and total knee replacement with ten-year survivor rate ranging from 71% to 94% [1-4]. This may be caused by several factors including the ankle joint being difficult to mimic in a prosthesis due to movement in three planes, the constant moving rotational axis in the talus during dorsiflexion-plantarflexion movement, and tibia bone strength rapidly decreasing below the surface [5,6]. Also, the population undergoing TAR is relatively young and ankle osteoarthritis is mostly of secondary origin (i.e. posttraumatic) [3-6].
Furthermore, preoperative coronal plane deformities, common in lateral ligament instability and posttraumatic osteoarthritis, can be challenging to correct. Correction of these deformities is important since it influences the prosthesis survivorship. It can be corrected with techniques such as hindfoot arthrodesis, medial malleolar osteotomy or soft tissue balancing [7,8].
Additionally, TAR is a challenging procedure with a steep learning curve which influences survivorship and complication rates [3,9-12]. Complications associated with TAR are intraoperative malleolus fractures, tendon or nerve lacerations, heterotopic ossification, delayed wound healing, infection, and aseptic loosening [3,4,9-20].
There are still additional developments in TAR designs. The Cadence Total Ankle System (Integra LifeSciences, Plainsboro, NJ) is a relative new ankle prosthesis introduced in 2016 [21]. To our knowledge, there are no published outcomes of the Cadence ankle prosthesis yet. Our hospital is the first in the Netherlands to use the Cadence prosthesis. Therefore, the aim of this study is to evaluate the short-term outcome of the Cadence Total Ankle System in terms of complications, clinical and radiological outcomes.
All 11 patients receiving a TAR procedure, mostly due to primary end-stage ankle osteoarthritis, utilizing the Cadence Total Ankle System between October 2017 and April 2019 in a single Dutch orthopaedic surgery department were included for the retrospective analysis. Mean age at surgery was 68.7 years (Table 1). Ten patients had 14 different procedures previous to TAR surgery, mostly triple arthrodesis for correction of varus (n = 3) or valgus (n = 6) ankle malalignment. The mean follow-up was 10.8 months (Table 1). Internal review board approval was obtained (ACLU # 2019.0032).
Table 1: Patients characteristics (n = 11). View Table 1
The Cadence Total Ankle System (Figure 1) is a fixed-bearing prosthesis with left and right specific components. The prosthesis is suitable for both primary and revision TAR and can be performed either cemented or cementless. The tibial component consists of titanium alloy and the talus component of cobalt chrome alloy. The insert consists of highly cross-linked ultra-high molecular weight polyethylene (UHMWPE) and comes in three shapes: Neutral, anterior-biased and posterior-biased. The wide sizing range should improve adaptation to individual patient anatomy [22].
 Figure 1: Cadence total ankle system.
View Figure 1
Figure 1: Cadence total ankle system.
View Figure 1
All procedures were cementless and were performed in accordance to manufacturer [22] by two surgeons (D.A.V., P.A.N.) with previous experience in TAR surgery. All additional procedures during TAR surgery, reoperations other than revision and revision procedures were registered. Revision was defined as replacement of any component of the implant, including the insert, or removal of the prosthesis and conversion to arthrodesis. Postoperative care consisted of a non-weight bearing short leg cast for two weeks followed by a weight bearing short leg cast for four to six weeks. Follow-up appointments took place at two and six weeks, three and six months and one year.
Intraoperative bone fractures and nerve or tendon laceration were scored as intraoperative complications and thromboembolism, delayed wound healing, infection and heterotopic ossification (HO) as short-term postoperative complications. Delayed wound healing was defined as a wound not closed at the two weeks post-operative appointment and was considered minor if non-operative treatment was necessary and major if surgical treatment was indicated. Infection was considered as superficial if oral antibiotic treatment was necessary, and as deep if intravenous antibiotic therapy and/or surgical treatment was necessary. HO was scored on post-operative radiographs in anterior-posterior (AP) and lateral view and was defined as any new osseous formation in either the medial, lateral, anterior or posterior gutter of the ankle [15].
Clinical outcomes were pain, ROM, clinical ankle alignment and patient satisfaction. Pain was scored on an 11-point pain Numeric Rating Scale (NRS) in which 0 represents no pain and 10 represents the worst pain imaginable and was obtained verbally in the postoperative period. ROM and ankle alignment were clinically determined during physical examination preoperatively and 3-6 months postoperatively. Patient satisfaction was collected from patient records and was scored as three levels: Very satisfied, moderately satisfied or unsatisfied.
Radiological outcomes were analysed using preoperative and postoperative radiographs in AP and lateral view. Tibial coronal alignment was determined with the medial distal tibial angle (MDTA) and tibial sagittal alignment was determined on the lateral radiograph with the anterior distal tibial angle (ADTA) (Figure 2). The ideal MDTA and ADTA is 90° with a range of 5° [13]. Tibiotalar alignment was determined as the angle between the mechanical axis of the tibia and a line tangential to the talar dome or talar prosthesis component (Figure 3). The ideal angle is 90° with a range of 5° [23]. The talar alignment was determined as the anteroposterior position of the talus in relation to the longitudinal axis of the tibia (Figure 4). When distance x was positive the talus is positioned anteriorly, when distance x was negative the talus is positioned posteriorly [20].
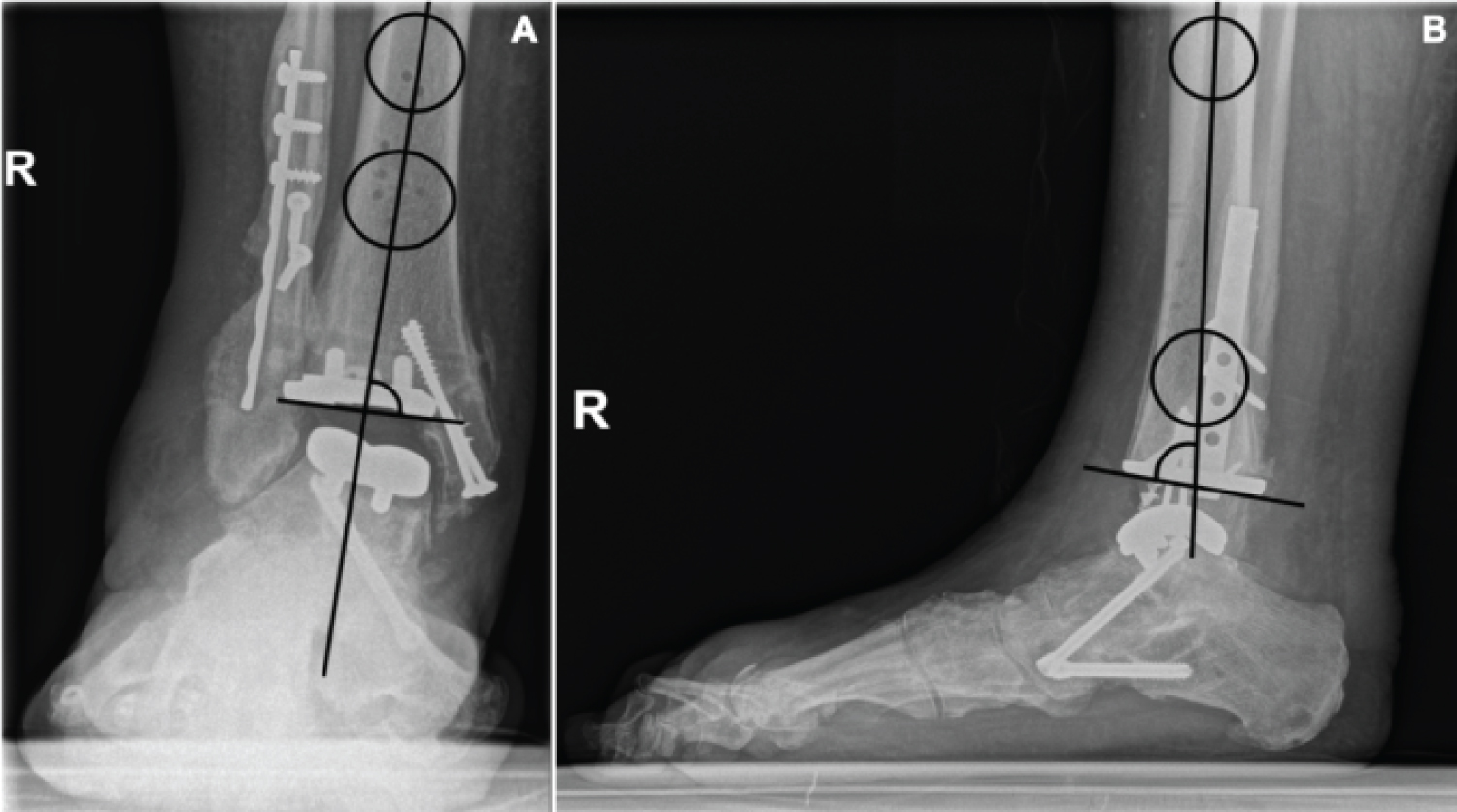 Figure 2: Tibial alignment measured with the angle between the mechanical axis of the tibia and, in the postoperative situation, the tibia component: (A) The medial distal tibial angle (MDTA) and; (B) the anterior distal tibial angle (ADTA).
View Figure 2
Figure 2: Tibial alignment measured with the angle between the mechanical axis of the tibia and, in the postoperative situation, the tibia component: (A) The medial distal tibial angle (MDTA) and; (B) the anterior distal tibial angle (ADTA).
View Figure 2
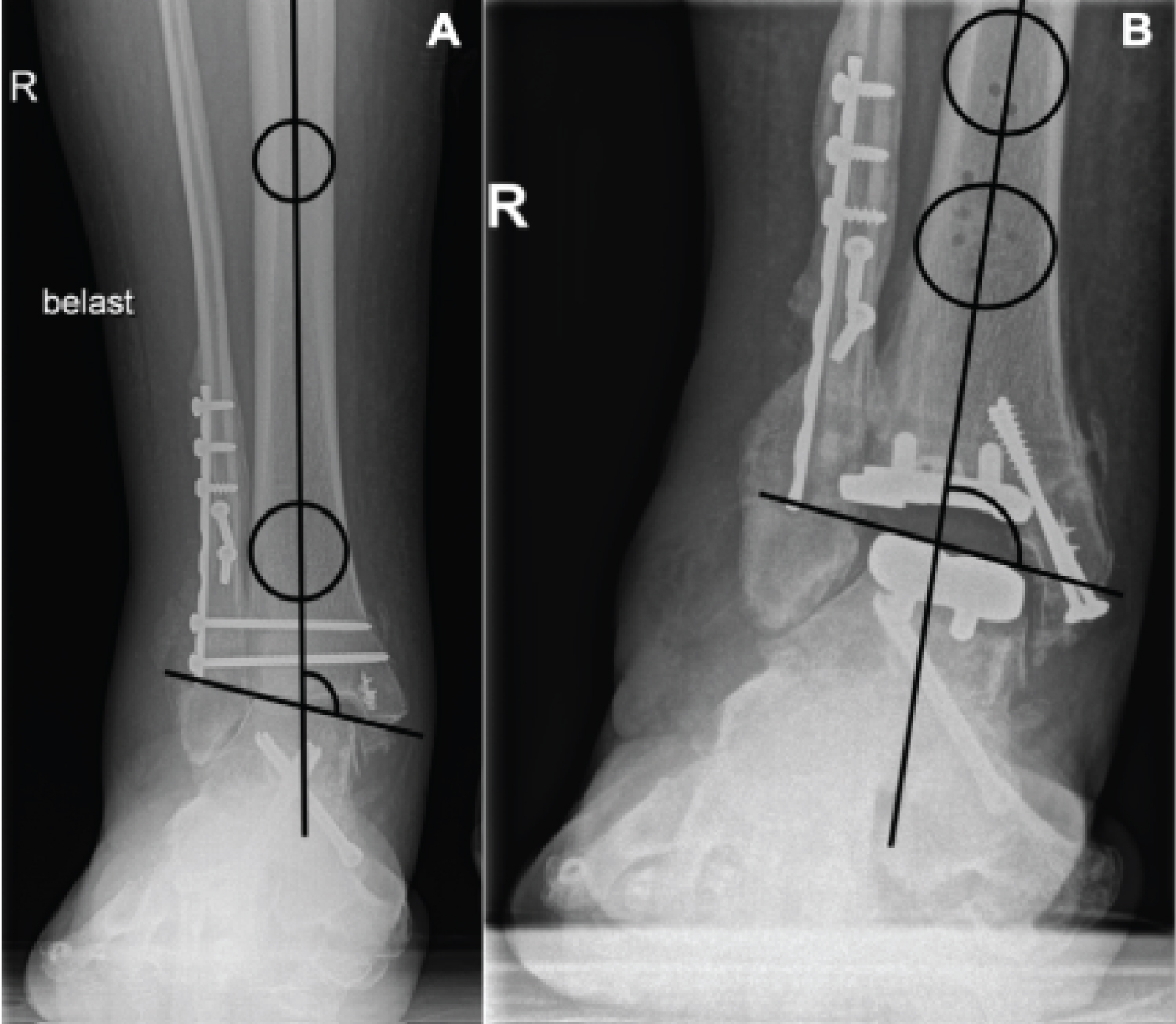 Figure 3: (A) Tibiotalar alignment measured with the angle between the mechanical axis of the tibia and a line tangential to the talar dome in pre-operative setting and; (B) The talar component in postoperative setting.
View Figure 3
Figure 3: (A) Tibiotalar alignment measured with the angle between the mechanical axis of the tibia and a line tangential to the talar dome in pre-operative setting and; (B) The talar component in postoperative setting.
View Figure 3
 Figure 4: Anteroposterior position of the talus determined with distance x, the distance between the centre of a circle on the talus component in relation to the longitudinal axis of the tibia.
View Figure 4
Figure 4: Anteroposterior position of the talus determined with distance x, the distance between the centre of a circle on the talus component in relation to the longitudinal axis of the tibia.
View Figure 4
Data was analysed using SPSS version 26.0 (released 2019. Armonk, NY: IBM). Continuous data are presented as means with standard deviations (SD) or as medians with interquartile and categorical data as frequencies with accompanying proportions. The Wilcoxon Singed Ranks tests were used to compare pre- and postoperative outcomes. Results were considered significant if p < 0.5.
During TAR surgery nine patients had 13 additional procedures, most commonly percutaneous Achilles tendon lengthening and osteosynthesis for intraoperative malleolar fractures (Table 2). All patients were discharged one or two days postoperatively. Five patients underwent a total of seven reoperations other than revision (Table 2).
Table 2: Surgery data. View Table 2
Nine intraoperative complications occurred in seven patients (63.6%). Six patients had a total of seven intraoperative fractures (Table 3). Five medial malleolar fractures were treated with internal fixation (ORIF) during TAR surgery (Table 2) and three patients had prolonged cast therapy. Two patients had an intraoperative injury of the superficial peroneal nerve (Table 3). One patient recovered completely.
Table 3: Intraoperative and short-term postoperative complications. View Table 3
Five patients (45.5%) suffered eight short-term postoperative complications (Table 3). In three cases a superficial wound infection occurred which was treated with oral antibiotic treatment with good results in all cases. HO occurred in five cases, all located anteriorly (Figure 5).
 Figure 5: Heterotopic ossification (HO) in the anterior gutter in one of the patients.
View Figure 5
Figure 5: Heterotopic ossification (HO) in the anterior gutter in one of the patients.
View Figure 5
The first days there was mild postoperative pain (Table 4). Preoperative ROM ranged from 5° to 50° with a mean of 26.7 ± 3.4 and ranged postoperatively from 10° to 35° with a mean of 22.5 ± 7.6. The total ROM and clinical ankle alignment did not change (Table 4). Preoperatively valgus malalignment was most common.
Table 4: Clinical outcomes. View Table 4
Six patients (54.5%) stated to be satisfied, four patients (36.4%) were moderately satisfied with their TAR despite their complications (Table 3). Two patients noticed a clicking sound in their ankle. One patient (9.1%) stated to be unsatisfied due to difficulties walking longer distances.
The preoperative MDTA ranged from 83.8° to 100.3° with nine ankles in the normal range between 85° and 95°. One ankle had a varus malalignment of 1.1° and one ankle had a valgus malalignment of 5.3°. Postoperatively the MDTA ranged from 82.9° to 96.5° with nine ankles in the normal range. The preoperative varus and valgus deformity were corrected to normal range. Two ankles gained a postoperative deformity, one varus malalignment of 2.1° and one valgus malalignment of 1.5°.
The ADTA ranged preoperatively from 81.1° to 105.2° with three ankles in the normal range between 85° and 95°. The mean deformity in the other eight patients was 3.8° ± 2.8°. Postoperatively the ADTA ranged from 82.9° to 96.5° with five ankles in the normal range. The mean deformity in the other six patients was 3.5° ± 2.3°. There was no significant difference in preoperative and postoperative MDTA and ADTA (Table 5).
Table 5: Radiological outcomes. View Table 5
Preoperatively the tibiotalar alignment ranged from 68.5° to 100.2° with four ankles in the normal range between 85° and 95°. Five ankles had a varus deformity with a mean of 7.6° ± 7.3° and two ankles had a valgus deformity of 0.6° and 5.2° degrees. The postoperative tibiotalar alignment ranged from 81.5° to 106.2° with seven ankles in the normal range. Two ankles had a valgus malalignment of 4.1° and 11.2°, and two ankles had a varus malalignment of 0.7° and 3.5°.
The mean preoperative talar alignment ranged between 0.9 mm to 12.8 mm and was translated anteriorly in all cases. The mean postoperative talar alignment ranged from 0.8 mm to 15.1 mm and was translated anteriorly in all cases. There was no significant difference in preoperative and postoperative tibiotalar and talar alignment (Table 5).
This study evaluated the short-term outcomes of the Cadence total ankle prosthesis in terms of complications, clinical outcomes and radiological outcomes.
In total nine intraoperative complications (81.8%) occurred in seven patients and eight postoperative complications (72.7%) occurred in five patients. Compared to the available evidence this is a high complication rate. Reported overall complication rates for TAR are between 14.3% and 40% [2,9,10,12,14,16,19,23], with reported intraoperative complication rates between 3% and 16% and postoperative complication rates between 13.5% and 19% [1,3,11,13,20,24,25]. Despite the high complication rates in this study most patients were satisfied with their ankle replacement. Most complications had no lasting effect, one patient had permanent nerve injury.
With the first patients, and in a small cohort, introducing a new prosthesis could lead to higher complication rates because of the surgeons learning curve with the new prosthesis design [9-11]. In a similar patient group, Nery, et al. reported 10 complications in 8 patients in a case series with their first 10 HINTEGRA TAR's [26]. Lee, et al. reported a complication rate of 60% in their first 25 cases which decreased to 20% in the following 25 cases [9].
Further, heterogeneity in complication reported makes it hard to compare complication rates. Complications are categorized as intraoperative and postoperative [1,3,11,13,20,25], as minor and major [18,19,26], as high grade, medium grade, and low grade [2,10,23], or are not classified at all [2,9,12,14,16]. A further issue is heterogeneity in which events are counted as complications, for example HO is sometimes mentioned as complication and sometimes as radiological outcome. It is also important to note that survival data is influenced by surgeon designer studies [3]. This could also affect complication rates. Likewise, database studies could have lower complication rates since only complications wherefore surgical intervention is needed are registered.
In this case series there was a high rate of reoperations other than revision (63.6%). This could be caused by the removal of osteosynthesis material in 50% of the medial malleolar fractures. In literature reoperation procedures vary between 2.9% and 26% [1,2,9,10,13,14,20,23-25]. In this study there were no revisions, which varies between 2.1% and 22.0% in other studies [1,10,11,13,14,20,23-25]. However, the follow-up of the current study was rather short.
Clinical evaluation showed no significant difference in pain score between the first postoperative day and the day of discharge. It should be noted that some patients were discharged on the first postoperative day. We had no preoperative pain scores to compare to and, due to the short-term follow-up in this study, no long-term pain scores. It has been shown that TAR significantly decreases pain scores on the long term [3,16,18,20,25,26].
There was no significant difference in ROM as opposed to other studies [3,19,20,25,26]. There even was a decrease in postoperative plantar flexion, although not significantly, which could be caused by an outlier score in the preoperative clinical measurement of 50°. Further, triple arthrodesis could affect postoperative ROM. Kim, et al. found in their study no significant difference in ROM after TAR in combination with hindfoot arthrodesis [8]. Since the majority of patients in this study underwent triple arthrodesis, this could possibly affect postoperative ROM.
The mean postoperative MDTA of 89.2° found in this study is comparable to other studies [9,10,15,20,24]. The mean ADTA was 90.5° with a mean deformity of 3.5° in six ankles. Literature is conflicting on the ideal ADTA. Some studies report an ideal angle of 90° [10,13,15] and other studies report an ideal angle of 85° [2,9,20]. The mean postoperative tibiotalar angle of 90.1° is comparable to other studies, with a reported mean angle of 88.5° and mean deformity of 1.6° and 3° [2,10,23]. The mean talar alignment of 7.3 mm was in all cases translated anteriorly, which was also found by Choi, et al. and Mann, et al. [2,20]. Mangegold, et al. and Barg, et al. found a more equal distribution in talar alignment, with normal and posterior translations as well [15,27].
It should be noted that not all radiographs in this study were weight bearing. Non-weight bearing radiographs could influence radiological alignment. Another factor complicating comparison of the results to other studies is the wide variety in alignment measurements and how they are reported (as mean angle, as mean deformity, or as mean varus deformity).
This study has several limitations. Firstly, it is a retrospective study. This means not all data was complete, there were no patient reported outcome measurements (PROMs) available as clinical outcome, there was no preoperative pain score and not all patients had weight bearing radiographs. Secondly, the surgeon learning curve that could be associated with a new prosthesis is of high impact in a small patient group. Another limitation is the short-term follow-up since we focused on intraoperative and short-term postoperative complications, which made it impossible to evaluate some important long-term complications such as cyst formation and radiolucency.
The short-term results of our first eleven Cadence total ankle prostheses showed a high complication rate. More research on this new prosthesis is necessary. Clinical outcomes are encouraging and show low postoperative pain scores, a preservation of ROM, and a good clinical alignment. Radiological alignment was in most cases within normal range. Most importantly, most patients were satisfied with their new ankle.
We believe this case series with the results of our first patients with the Cadence total ankle prosthesis is important as they are the first result of this new prosthesis and they are outcomes by non-designers. These outcomes are important for other surgeons to learn from and to compare their own outcomes too.
The authors want to thank Marjolein Schager for providing language help.
The authors declare that there is no conflict of interest.