A biomechanical foot orthosis is commonly used for the management of lower extremity injuries that are related to flexible flat feet. The purpose of this study was to document the effect of a maximal arch supination stabilization (MASS) orthosis on foot motion in individuals with flexible flat feet who experience lower extremity exertional pain.
30 subjects with flexible flat feet and lower extremity exertional pain received a pair of custom orthoses. Intersegmental foot kinematics were recorded during normal overland walking in 2 footwear conditions - a sandal with an orthosis (SWO) and a sandal without an orthosis (SW). Six different dependent variables were assessed simultaneously to determine the effect of each condition. A multivariate analysis of variance (MANOVA) was used to assess the multiple dependent variables simultaneously with a level of statistical significance set at 0.05. Survey data was collected twelve months after data collection to assess exertional pain symptoms and how often the subjects were wearing their orthoses.
A significant difference was not found between conditions for any of the kinematic measurements of the left and right feet. The majority of the sample population experienced at least some degree of improvement with respect to their lower extremity exertional pain symptoms.
The MASS orthosis did not influence the joint kinematics of the forefoot, medial longitudinal arch deformation, or the first ray kinematics during normal overland walking. However, survey results indicate that the MASS orthosis is clinically effective in reducing lower extremity exertional pain of a non-traumatic origin.
Orthosis, Biomechanics, First Ray, Hypermobile
MASS: Maximal Arch Supination Stabilization; SW: Sandal Walking; SWO: Sandal Walking with Orthosis; MLA: Medial Longitudinal Arch
Low arches or flat feet are associated with an increased risk of injury among physically active people, and it is widely believed that this foot type tends to be more flexible than other foot types allowing for a disproportionate amount of pronation during the gait cycle [1,2]. Flexible flat feet have been theorized to impact the movement and muscular activity patterns of the lower leg, predisposing such individuals to lower extremity musculoskeletal injuries [3-5].
Excessive pronation at the subtalar and the transverse tarsal joint is believed to be associated with a flexible flat foot [6,7]. This foot type has been suggested to be a contributive factor in the loss of ligamentous and osseous stability, necessitating increased muscular activity in the lower leg and foot to maintain that stability [8]. Additionally, this lack of stability may cause an increase in the magnitude of the stress and shear forces that are transmitted to the soft connective tissues. Excessive pronation is the etiological variable most commonly linked to overuse injuries [4,5]. The subsequent increase in muscular activity and transmitted forces associated with excessive pronation can ultimately lead to muscle fatigue, which is associated with a variety of overuse injuries of the lower extremity [5,9]. A biomechanical foot orthosis is commonly used for the management of lower extremity injuries that are related to excessive pronation or flexible flat feet [8,10].
Increasingly, foot orthoses have been successfully used as an adjunct treatment for symptoms that are secondary to increased foot flexibility. One study revealed that of 465 podiatric patients reporting various pathologies, 62% acknowledged complete resolution of their chief complaint after orthotic treatment while an additional 33% gained partial resolution [11]. Similarly, in a retrospective study with both temporary soft orthoses and permanent rigid orthoses, 96% of patients experienced pain relief, while 70% were able to return to previous levels of activity [11-13].
The use of foot orthoses in the treatment of abnormal foot biomechanics has been extensively described in the literature, and those interventions can be grouped into two categories - accommodative or corrective. Regardless of the orthotic prescription, it is difficult to judge the scientific merit of the recommendations that have been generated by previous studies due to the conflicting results of those studies [1,7,11,14].
Although the theoretical basis for the efficacy of an orthosis has been well developed (improved alignment and motion control), the evidence supporting this theory is conflicting and the scientific basis for its use in the treatment of lower extremity pathologies has been questioned [4,10]. Some of the uncertainty has been attributed to the conflicting results found in the literature documenting the biomechanical effect of an orthosis on the lower extremity and the foot. The inconsistent findings regarding the effectiveness of a biomechanical foot orthoses and how it alters the kinematics of the lower extremity could be attributed to varying study methodologies and designs. These differences can include small sample size, asymptomatic participants, in-adequate break in periods, non-standardized footwear, and differences in the types of orthoses used. This combination of variables may help to explain some of the disparity in the lower extremity kinematics documented in the literature [15].
The purpose of this investigation was to document the effect of the MASS orthosis on the forefoot, medial longitudinal arch (MLA), and first ray kinematics of individuals with flexible flat feet and lower extremity exertional pain. We hypothesized that a MASS orthosis would decrease the extent of angular motion of the segments of the foot as well as the deformation of the MLA.
This study compared the stance phase mechanics of individuals with lower extremity exertional pain with flexible flat feet during normal overland walking in a modified conventional TEVA sandal and in the same sandal with a customized MASS orthosis. The MASS orthosis is a custom calibrated orthosis that is meant to deliver a corrective force to the MLA of the foot, which, theoretically, will lower the head of the first metatarsal.
A convenience sample of 40 subjects was screened for participation in this study. The sample was comprised of students, faculty and staff from a major New England university. Thirty-one met the inclusion criteria for the study. One participant was lost due to their inability to follow-up for the data collection portion of the study. The 30 individuals (25 women) who completed the study ranged in age from 20 to 49 years (Table 1) and exhibited various complaints of foot, heel, leg, and knee pain. Fourteen of the subjects identified medial or lateral knee pain as their lower extremity symptom. Eleven of the subjects reported foot or heel pain; while the remaining five subjects complained of shin pain (Table 2). Informed consent and a medical history were obtained from each participant prior to taking any measurements. Individuals were excluded if they had sustained any lower extremity fractures or injuries to the capsular or ligamentous structures of the lower leg or foot within the past 12 months.
Table 1: Statistics of subjects participating in the study. View Table 1
Table 2: Lower extremity pathologies reported by participating subjects. View Table 2
Individuals were included in the study if they had a navicular drop greater than or equal to 10 mm bilaterally, [2,16] and if they had at least 60° of frontal forefoot to rearfoot passive range of motion (as determined by the Gib test) [17] in both feet. This movement was measured via visual estimation (Figure 1). At the time of this study, the Gib test was utilized by the manufacturer as a screening measure necessary for the fabrication and calibration of the orthosis. However, due to the subjective nature and less than adequate reliability of the test, the navicular drop test was also used by the investigators to define a subject's inclusion into the study (Table 3).
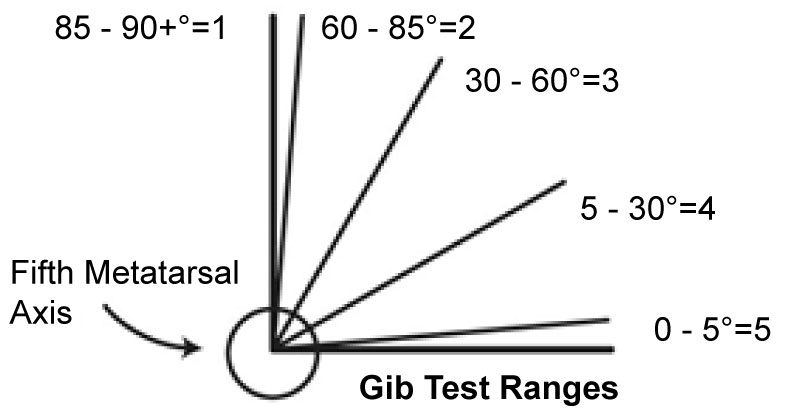 Figure 1: Gib test ranges.
View Figure 1
Figure 1: Gib test ranges.
View Figure 1
Table 3: Descriptive statistics regarding navicular drop of all subjects participating in the study. View Table 3
Upon completion of the structural evaluation, participants were casted for a pair of custom MASS orthoses. The primary investigator was certified in the casting technique, and casted each subject for their orthoses. Casts were obtained according to the standardized casting procedures of the orthosis manufacturer. This sequential process entailed a gait referenced non-weight bearing foam box casting, which captured the maximal amount of arch that one can comfortably achieve at midstance with the heel and forefoot in full contact with the ground (Figure 2).
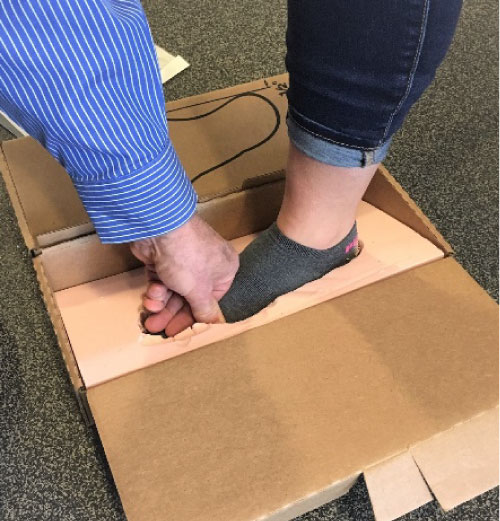 Figure 2: Subject's foot in the final stage of casting.
View Figure 2
Figure 2: Subject's foot in the final stage of casting.
View Figure 2
There were three points of contact that were used as a reference within the cast - the center of the calcaneus, and the centers of the heads of the first and fifth metatarsals. The depth of the cast at these points was measured with a ballpoint pen and then visually assessed to confirm equal depth at each point. Once accomplished, the casts and orthosis prescription were shipped to the manufacturer and an orthosis dispensing visit was scheduled approximately two weeks later.
At the second visit, proper fit of the orthosis was verified by the primary investigator, and the study participants were instructed on their break-in and use. The subjects used their own footwear during the break-in period and could take part in normal activities. The only activity that was restricted prior to the actual data collection was competitive and recreational running with the orthosis in the shoe. A third visit was scheduled six weeks after the second visit for the sole purpose of data collection. The orthosis featured a semi-rigid thermoplastic heel cup extending to the base of the metatarsals with a full length, 1/8-inch-thick perforated ethylene vinyl acetate top cover (Figure 3).
 Figure 3: Orthosis with perforated EVA top cover.
View Figure 3
Figure 3: Orthosis with perforated EVA top cover.
View Figure 3
At the end of the six-week accommodation period, all participants attended a data collection session. At this session, retro-reflective markers were placed on the lower extremities, and feet over specific bony landmarks. Figure 4 represents the marker placement, while Table 4 provides the specific details of the marker set as they relate to the corresponding anatomical landmarks.
 Figure 4: Retroreflective markers, sandal and orthosis that were utilized in the study.
View Figure 4
Figure 4: Retroreflective markers, sandal and orthosis that were utilized in the study.
View Figure 4
Table 4: Anatomical landmarks of the AI DuPont multi-segment foot model set. View Table 4
Using a commercially available software package (Cortex, Motion Analysis Corporation, Santa Rosa, CA), the marker displacement coordinates were obtained, and low pass filtered using a 4th order Butterworth filter with a 10 Hz cutoff. Using the filtered data, kinematic model, and a commercially available software package (Foot 3D, Motion Analysis Corporation, Santa Rosa, CA), the footfall event data and three-dimensional kinematics of the rearfoot, forefoot, and two-dimensional kinematics of the first ray were obtained using a Euler decomposition method. For full details of the kinematic model and the procedure used to obtain the three-dimensional angular displacements please see Appendix 1A.
Using an eight-camera video system sampling at a rate of 240 Hz, the three-dimensional position of the retro reflective markers were recorded while the participants walked over level ground at a self-selected walking speed under one of two footwear conditions. The footwear conditions consisted of walking in a sandal (SW) and walking in a sandal with the orthosis (SWO). The orthosis was secured to the sandal with two-sided tape. A modified Teva® sandal was used for the walking trials (Figure 5a and Figure 5b). The sandal foot bed was flat allowing the orthosis to sit on it without any need for accommodation. To allow for full visibility of the foot markers, the sandals were modified by removing the manufacturer supplied straps, apart from the anchoring straps, and replacing them with 1/2-inch Velcro.
 Figure 5a: Modified teva sandal (medial view).
View Figure 5a
Figure 5a: Modified teva sandal (medial view).
View Figure 5a
 Figure 5b: Modified teva sandal with orthosis (medial view).
View Figure 5b
Figure 5b: Modified teva sandal with orthosis (medial view).
View Figure 5b
A walking trial consisted of the participant walking continuously at a self-selected walking speed within the laboratory setting, making wide-angle turns at each end of the room. Twelve trials of video data were collected for each participant (six trials in each footwear condition). Everyone walked in the SW condition first, followed by walking in the SWO condition.
Twelve months after attending their last data collection session, each subject completed a survey to determine the status of their exertional pain symptoms (assessed using a Likert scale), and how often they were wearing their orthoses.
The marker position data were used to obtain three-dimensional kinematics of the rearfoot, forefoot, and first ray, as well as the dynamic arch index, during each of the walking trials. Dynamic arch index was defined as the vertical distance to the navicular marker from the floor, divided by the distance from the inferior calcaneal marker to the first metatarsal marker. The stance phase of the walking trials was extracted, and time normalized to 100 frames (1 and 100 representing heel strike and toe off, respectively). The maximum value of the rearfoot, forefoot, and first ray angles and dynamic arch index of five stance phases for each footwear condition were obtained. Heel strike, midstance, and toe off were the three phases of stance that were analyzed for this study.
To determine the effect of condition (orthosis versus no orthosis) six dependent variables were simultaneously analyzed: Maximum sagittal, frontal, and transverse plane forefoot angle; maximum sagittal and transverse plane first ray angle; and maximum sagittal plane displacement of the medial longitudinal arch (arch index). A multivariate analysis of variance (MANOVA) was used to assess the multiple dependent variables in a simultaneous manner. The level of statistical significance was set at 0.05.
No significant differences were noted between conditions for the maximum values for either lower extremity for any of the dependent variables, including the arch index.
The survey data revealed that 80% of the sample population experienced at least some degree of improvement with respect to their lower extremity exertional pain; while 33% of those participants reported a complete resolution of their symptoms (Table 5 and Table 6). Of the ten participants who said their symptoms had resolved - six had experienced foot pain, two had experienced knee pain, and two had experienced shin pain. Of the eight participants who said their symptoms were significantly better - five had experienced knee pain, while the remaining three had experienced foot pain.
Table 5: Survey results regarding subjects' lower extremity exertional symptoms after twelve months. View Table 5
Table 6: Survey results regarding subjects' wear schedule of their orthoses after twelve months. View Table 6
The goal of a custom foot orthosis prescription is variable, with the orthosis fabrication based on the specific needs of the patient. The MASS orthosis used in this study is generally prescribed for patients with flexible flat feet and abnormal pronation. Its specific goal is to restore normal and pain free ambulation, allow the foot to accommodate to all ground reaction forces, and, lastly, to provide adequate stability for propulsion.
The manufacturer of this orthosis theorizes that for the MASS orthosis to be effective it must be able to impose adequate mechanical control over the tarsus of the foot with its primary emphasis placed on the calcaneus and talus. This orthosis provides its support along the entire plantar surface of the MLA of the foot. Theoretically, the full contact of the orthosis with the MLA will slow down the medial talar velocity during the stance phase of gait, thus giving mechanical advantage to the orthosis.
The primary claim of the MASS orthosis is that its high arch design can impact planter flexion/dorsiflexion of the first ray of a flexible flat foot. Purportedly, this will maximize the "windlass" mechanics of the MLA by maximally tightening the plantar aponeurosis, thus restoring the height of the arch and facilitating the windlass mechanism of the foot [18,19].
Based on the results from this investigation, the maximum first ray kinematic value is not effected. These findings are in agreement with Nawoczenski and Ludewig's findings of a lack of an orthotic effect on first ray movement during the stance phase of the gait cycle [20]. Nawoczenski and Ludewig compared a forefoot posted orthosis to the same orthosis utilized in this investigation and failed to find a significant effect on first ray or hallux motion [20]. The lack of an orthosis effect on first ray kinematics in Nawoczenski and Ludewig's and our study does not support the manufacturer's claim of the high arch design's ability to influence the mechanics of the first ray.
There are several potential reasons that exist for the lack of a significant difference between conditions (SW and SWO) in this investigation as well as other studies. The use of asymptomatic populations, non-custom made orthoses, inadequate break-in periods, and small sample sizes are just some of the reasons that exist that can contribute to the lack of a significant effect.
Inadequate break-in periods or the use of non-custom orthoses may cause individuals to alter their movement patterns to avoid unfamiliar or inappropriate sensory inputs intended by the orthosis. This may also be the case for asymptomatic individuals who are receiving inappropriate sensory information from an orthosis that is constructed to create a biomechanical modification [21]. The use of a small sample size may also be problematic given the degree of variability that is encountered in intersegmental foot kinematics within and between subjects. However, this investigation addressed those issues by allowing an adequate accommodation period thus minimizing the effect of abnormal sensory input on the foot. Furthermore, an adequate sample size was recruited allowing for the detection of a clinically meaningful orthosis effect, and to account for the degree of foot motion variability.
However, the issue of adequate subject selection and the ability to classify the participant's foot as meeting the inclusion criteria was questioned. The multifactorial movement of the foot increases the difficulty of categorizing a participant's foot, and this could have contributed to the insignificant results of this investigation.
Even though there was a lack of a significant effect of an orthosis on foot kinematics, the survey data appears to indicate that a MASS orthosis may be able to reduce exertional pain experienced by our subjects. Given the lack of a significant effect on motion control of the foot and the survey findings regarding the reduction in exertional pain - the choice of which orthosis to use, if one is prescribed, should take into account the ability of the orthosis to reduce a patient's painful symptoms.
There were two main limitations associated with this study that potentially affected the results and the subsequent interpretation of the findings. In the absence of a control group, the contributions of any placebo effect to the findings really cannot be explained in any detail. Secondly, the lack of a baseline motion assessment did not allow the investigators an opportunity to monitor and assess the impact of the orthosis on foot kinematics.
This study examined the effectiveness of a clinically recommended orthosis on the joint kinematics of flexible flat feet during normal self-paced overland walking. Given our results, the use of this orthosis does not appear to influence the sagittal, frontal, or transverse plane joint kinematics of the forefoot, medial longitudinal arch, or the first ray. However, based on the follow-up survey data, it appears that the MASS orthosis is clinically effective in reducing lower extremity exertional pain of non-traumatic origin.
The orthoses for this investigation were provided free of charge by Sole Supports, Inc., Lyles, TN.
Both Dr. Elliott and Dr. Garbalosa were equal contributors to this research investigation.