Hallux valgus (HV) is a common deformity of the forefoot in which a deviation of the first metatarsophalangeal joint arises. HV has been described to be characterized by a number of structural factors including radiographic angles, metatarsal length, metatarsal head shape, sesamoid position, first metatarsocuneiform joint flexibility and pes planus [1-5]. The etiology is not fully resolved. However, HV is associated with gender, age and family history. Moreover, it is limited to shoe-wearing cultures and dependent on footwear in adolescence and adulthood [6,7].
Pathophysiologically, hyperlaxity in the first tarsometatarsal joint, hypermobility of metatarsal bone and muscle imbalance contribute to the emergence of hallux valgus deformity [8,9]. Though, the clinical evidence of tarsometatarsal joint hyperlaxity is difficult. In severe forms hypermobility of the metatarsal bone can lead to a dislocation or even to a luxation in the metatarsophalangeal joint [10]. Cadaveric studies indicate that first ray mobility can be reduced by a proximal crescentic osteotomy and distal soft tissue reconstruction (DSTR) without tarsometatarsal fusion [11,12].
Patients suffer from manifold symptoms including pain in the bunion area, lack of space for the other toes due to the deviation of great toe leading to transfer metatarsalgia and pseudo bursitis. On radiographs an increase of the intermetatarsal angle and a deviation of first ray alignment can be observed [2,7,11].
Multiple treatment algorithms including distinct surgical procedures such as Scarf or Chevron type of osteotomies , arthrodesis or soft tissue techniques have been published during the last decades [13,14].
Within these, the Lapidus arthrodesis (LA) represents a surgical option for treatment of moderate and severe hallux valgus deformity in the setting of a hypermobile first ray [15-18]. LA involves fusion of first tarsometatarsal (TMT1) joint with an additional distal bony and soft tissue procedure [19-23]. Non-union rates of LA are reported with up to 12% in the literature [8,10,12].
The purpose of this retrospective study was to reveal the clinical and radiographic outcomes in two patient cohorts being treated with two modifications of interfragmentary screw placement in the LA. The issue was how much hard-ware and how much stability is necessary in LA in terms of union rates. Another focus was on determination of shortening of the first ray after LA.
Between 2011 and 2013 a total of 62 patients (64 feet) suffering from mild to severe hallux valgus deformity were treated surgically using the Lapidus procedure.
All patients had failed conservative treatment (physiotherapy, orthosis) and showed none or mild degenerative changes in the metatarsophalangeal joint on standard x-rays (Kellgren-Lawrence grades I and II).
Exclusion criteria were previous trauma and surgery of the affected foot, severe degenerative changes in the metatarsophalangeal joint (Kellgren-Lawrence grades III and IV) and foot malformations in childhood.
Prior to surgery all individuals were positioned supine on the operating table with a cushion under the ipsilateral buttocks and a calf tourniquet was used for hemostasis. The skin was incised on the medial aspect of the first ray reaching from the metatarsophalangeal joint to the medial cuneiform. The TMT1-joint capsule was incised on the medial side and a partial release of the anterior tibial tendon fibres at the first metatarsal base was obtained protecting the main insertion of the tendon at the medial cuneiform. To expose the tarsometatarsal joint space a Hintermann distractor was inserted. The cartilage of the first metatarsal base was resected using an oscillating saw. The metatarsal was held in correction and an appropriate amount of cartilage and bone was resected at the medial cuneiform to obtain an orthograde and slightly plantar flexed TMT1 arthrodesis. The bony surfaces were then reduced and maintained by temporary applied 1.6 mm K-wires. Proper alignment was checked radio graphically. In all patients, a plantar plate (Plantar Lapidus Plating System, DARCO®, Wright Medical, Memphis, TN) served for internal fixation of the LA.
In the first cohort an additional extraplate screw (EPS) (DARCO® Wright Medical, Memphis, TN) placed prior to the plantar plate was applied to obtain compression of the arthrodesis gap. Crossing the arthrodesis the screw was directed from the dorsomedial aspect of the first metatarsal base into the medioplantar region of the medial cuneiform.
In the second cohort the distal non-locking screw of the plantar plate was placed across the arthrodesis gap to obtain compression (intraplate screw, IPS). To ensure proper plate and screw positioning biplane radiographs were performed (Figure 1 EPS and Figure 2 IPS).
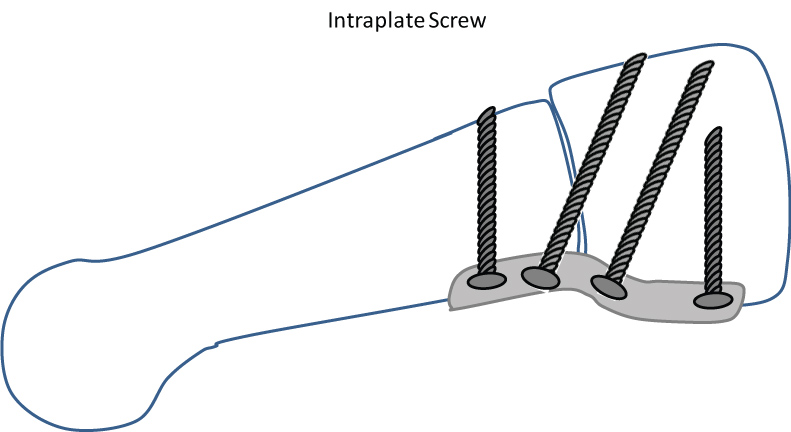 Figure 1: Modified Lapidus arthrodesis with plantar plate.The distal non-locking screw is placed retrograde across the osteotomy gap [20]. View Figure 1
Figure 1: Modified Lapidus arthrodesis with plantar plate.The distal non-locking screw is placed retrograde across the osteotomy gap [20]. View Figure 1
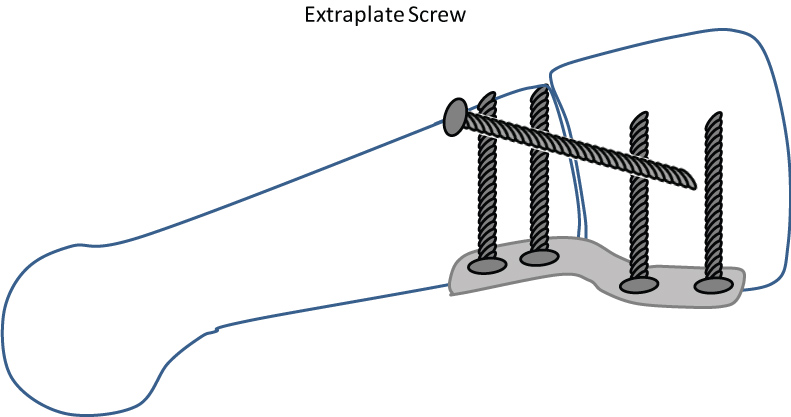 Figure 2: Modified Lapidus arthrodesis with plantar plate and extraplate compression screw [11,20,23]. View Figure 2
Figure 2: Modified Lapidus arthrodesis with plantar plate and extraplate compression screw [11,20,23]. View Figure 2
Furthermore, a distal soft tissue procedure was added in all cases. At the medial side after skin incision neurovascular structures were explored. After t-shaped capsular incision bunion was removed under protection of sesamoid slide bearing. The medial metatarsosesamoid ligament and medial collateral ligament were explored and capsular plication was done.
At the lateral side the skin was incised in first interdigital space. The adductor hallucis aponeurosis was intersected and a tenotomy at the basis of proximal phalanx was performed. The capsule was released at the upper edge of lateral sesamoid bone until full adjustment of sesamoidal subluxation is attained.
An Akin-osteotomy was additionally performed if signs of hallux valgus interphalangeus were present. A modified Chevron osteotomy was carried out in cases with incongruity of the first metatarsophalangeal joint indicated by an increased distal metatatarsal articular angle.
Active and passive mobilization started one day after surgery using a forefoot relief shoe orthosis for a total of 6 weeks. To promote soft-tissue healing patients were requested to keep to partial weight bearing with 20 kg on crutches for 2 weeks postoperatively followed by transition to full weight bearing. Patients were encouraged to do active ankle exercises in the supine position to aid in reduction of soft-tissue swelling. Six weeks after surgery bone healing was checked radio graphically in standard planes and full-weight bearing was recommended.
There were no significant differences in demographic data between the cohorts (Table1).
The study was reviewed by the local Ethics Committee (study number 17-7441-BO) and informed consent was obtained from all individual participants included in the study.
Outcome and patient satisfaction were evaluated using the AOFAS and FADI scores as well as weight bearing dorsoplantar and lateral radiographs of the affected foot. Furthermore, tangential radiographs of the sesamoid bones were taken.
The Intermetatarsal Angle (IMA), Hallux Valgus Angle (HVA) and Tibial Sesamoid Position (TSP) were evaluated. The length of the first ray was measured with a modification of the Hardy and Clapham's method. Their method is based on the measurement of the distance between two arcs created from a line between calcaneocuboid joint and medial tuberosity of navicular crossing that of second metatarsal line to the apex of first and second metatarsals [24]. Due to different magnification factors in the x-rays we did not only determine the absolute values, but for comparative purposes we so created a quotient of the absolute values to obtain comparable data.
In order to prevent accidental and systematic errors, radiographic evaluation was performed by two blinded surgeons on a single day and repeated in a random order. Non-union was defined as lesser than 3 cortical bridges on anteroposterior and lateral radiographs 6 months after surgery.
Summary statistics of the data were expressed as mean ± SD. The Shapiro-Wilk test was used to test for normal distribution. The paired Student's t-test was used for comparison of the normal distribution of pre- and postoperative means and the Wilcoxon signed-rank test for non-normal distribution. The comparisons with p-values < 0.05 were considered to be significant. The software SPSS 19 (SPSS Inc. Headquarters, Chicago, Illinois, USA) was used to carry out the statistical computations.
Of the 62 patients treated with a LA 30 individuals (32 feet) were available for a complete follow-up. Moreover, 17 were available only for telephone interview, whereas 15 were lost for follow-up.
The IPS-group consisted of 12 patients available for clinical and radiographic follow-up. The EPS group was composed of 20 patients available for clinical and radiographic follow-up. 15 patients were only available for telephone interview.
The first metatarsal bone was additionally adjusted by a modified Chevron osteotomy in 7of 32 cases (22%). An Akin osteotomy was performed in 12 of 32 cases (38%). To correct dactyl malalignments Weil osteotomies were carried out in one or more lesser toes in 20 of 32 cases (63%).
The average follow-up was 42.5 ± 21.9 (29-74) months. There was no significant difference in the follow-up period (p = 0.19) between the two cohorts.
The mean scores being surveyed prior and after surgery are presented in table 1. In all scores the patients achieved a significant (p < 0.001) improvement after surgery (Table 2).
Table 1: Demographic data of both cohorts; BMI = Body mass index. Male. View Table 1
Table 2: Scores prior and after surgery. View Table 2
On the basis of complete documentation radiographic analysis was performed in 32 cases before and after surgery. The mean intermetatarsal angle changed from 18.8° preoperative to 8.3° after surgery (p < 0.001). The hallux valgus angle was reduced from 43.5° to 18.3° on average (p < 0.001). Concerning radiographic improvements in intermetatarsal and hallux valgus angle no differences between the IPS-or EPS-cohort could be observed (p = 0.66 and p = 0.59) (Table 3).
Table 3: Radiographic angles for IPS and EPS; 1st IMA = first intermetatarsal angle, HVA = Hallux valgus angle. View Table 3
A bunion recurrence was found in 5 (16%) cases (EPS = 3; IPS = 2). Radiographic signs of ostearthritis in metatarsophalangeal joint exacerbated in 4 (13%) (EPS = 3; IPS = 1) cases. The tibial sesamoid bone position improved from 5.3 ± 1.3 to 3.6 ± 1.5 on average according to the classification of Hardy and Clapham (EPS: 5.5 ± 1.4 to 3.9 ± 1.6; IPS: 4.8 ± 1.4 to 2.9 ± 1.2; p = 0.67) .There was a significant shortening of the first ray after surgery from 1.04 to 1.01 (p < 0.01). No significant difference in first ray shorting could be observed comparing the EPS and IPS cohorts (EPS: 1.05 ± 0.03 to 1.02 ± 0.03; IPS: 1.04 ± 0.03 to 1.02 ± 0.03; p = 0.58).
Revision surgery was necessary in 2 cases due to nonunion of the Lapidus-Arthrodesis (6%). There was one nonunion case in each cohort meaning a nonunion rate of 8% (1 of 12) in the IPS group and 5% (1/20) in the EPS group (p = 0.57).
Since its first description, many modifications of the Lapidus arthrodesis (LA) have been developed to improve its results [14]. The Lapidus procedure is well-established and patient satisfaction is reported to be high [25]. Yet, LA is connoted with high non-union rates. In the past crossed screw fixation has been outlined to be a reliable technique for fusion of the tarsometatarsal joint [10,15,26,27].
In recent years cadaveric studies demonstrated non-uniform results. Roth, et al. (2014) showed that plantar plate fixation created a stronger and stiffer construct than intramedullar fixation [28]. On the contrary, Baxter, et al. claimed that traditional, lagged cross-screws provide greater stability compared to a dorsally placed compression plate [25]. Garas, et al. stated that the addition of a lag screw to plate osteosynthesis extends the maintenance of compression in tarsometatarsal arthrodesis [29]. Recent studies demonstrate that the plantar plate position is superior to the dorsomedial position [15-18,30].
First clinical studies report on suitable stability and an acceptable level of complications of combined plate and intramedullary fixation [31,32].
The topic of fixation technique in arthrodesis and trauma has been subject of debate for a long time. The current data situation is inconsistent. There are reports presenting divergent views about intra and extramedullary fixation concerning non-union rates and clinical outcome [33-36].
We compare two modifications of the Lapidus procedure based on the same study design. Finally, we introduce a new modification of the LA.
We compare two methods to fuse the first tarsometatarsal joint. The first method includes a combination of intra- and extrameduallary osteosynthesis via plantar plate and single lag screw. The other method consists of plantar plate osteosynthesis. One screw was placed retrograde and interfragmentary.
The question about the optimal fixation technique in Lapidus procedure still remains unclear and under investigation. The primary criterion is the creation of maximum initial stability. Failing that, micro movements can result in pseudarthrosis. In addition, surgeons intend to use as little foreign material as possible. This is because foreign material may harm local blood supply of the bone and increases infection rate. In addition, economic aspects required consideration.
In the majority of our patients union of TMT-1-arthrodesis could be achieved without any complications. Nevertheless, in 6% (2/32) symptomatic pseudarthrosis occurred and revision surgery was indicated. The non-union rates observed are comparable to the rates reported in literature quoted between 5 and 12% [8,10,12,15,37]. Comparing the two modifications (IPS and EPS) of the LA no difference in union-rates could be observed. Regardless of the surgical technique applied we have found significant shortening of the first ray postoperatively without any significant differences between the two groups.
From this point of view there is space for improvement of our technique. The application of cancellous autologous bone grafts might help to reduce non-union rates and reduce the amount of postoperative shortening of the first ray. Bone graft is a frequently used technique in foot and ankle surgery. Due to high complication rates in ipsilateral iliac crest as donor site, there is an increasing evidence to harvest cancellous bone graft from ipsilateral tibia or calcaneus [38,39]. Mani, et al. underlined the benefits of bone grafting to reduce non-union rates [10].
Clinical and radiographic outcome as well as complication rates of the two surgical modifications (EPS and IPS) showed no significant differences. Thus we conclude that there is no benefit of an extraplate lag screw in LA. Plantar plating with an intraplate compression screw seems to provide enough compression on the surfaces and stability for the arthrodesis. However, further studies with higher case numbers have to be conducted to clarify the role of the interfragmentary lag screw.
We have to concede that our study has some limitations. The main limitation is the small number of patients and the loss of follow-up of a large percentage of patients. 15 patients were only available for telephone interview. 10 patients were lost for follow-up and 5 patients died from diseases not related to the Lapidus surgery prior to follow-up.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval and consent to participate: The study was reviewed by the local Ethics Committee (study number 17-7441-BO) and informed consent was obtained from all individual participants included in the study.
All patients consented to publish personal data in an anonymised form.
All patient-related data were collected by file research from the archives of the Department of Orthopaedics and Trauma Surgery, University of Duisburg-Essen.
None of the authors had competing interests.
All authors insured that they substantially contributed to the article and that they are in agreement with form and contents of the manuscript.