Introduction: Most anesthesiologists use the thoracic epidural, with a 0.75% incidence of accidental perforation. However, they are reluctant to consider higher levels for spinal anesthesia because of the possibility of direct spinal cord injury. The main objective of this retrospective study was to evaluate the incidence of paresthesia and neurological complications, as well as cardiocirculatory changes after thoracic spinal anesthesia.
Methods: We conducted a retrospective audit, between January 2007 and December 2019. We reviewed the record sheets of patients who experienced paresthesia for thoracic spinal anesthesia with two types of needles of the same gauge, isobaric and hyperbaric 0.5% bupivacaine and puncture in the sitting or left lateral position, and median and paramedian insertion.
Results: Paresthesias occurred in 5.9% of patients. 41 patients experienced a paresthesia with cut needle compared with 43 patients with pencil point, without statistical difference. All paresthesias were transient, and lasted a maximum of three days. No sequelae neurologic were observed in all patients during this study. Bradycardia occurred in 3.1% of the patients and hypotension in 13.2% of the patients, easily corrected by the use of atropine and vasopressor.
Conclusion: All 84 paresthesias observed in this study were associated with free flow of CSF when the stylet was removed from the needles. An association was not found between the type of the spinal needle and the incidence of paresthesias. This study with 1,406 patients showed that thoracic spinal anesthesia is safe and without neurological sequelae, with a puncture between T8 and T11.
Paresthesia, Anesthesia, Subaracnoid, Needles, Thoracic spinal anesthesia
Thoracic spinal anesthesia was used at the beginning of the early 20th century to perform surgeries in the neck, mouth and chest, showing that the middle thoracic region is more difficult to access in relation to high and low thoracic level [1]. Four studies on epidural anesthesia showed that in 1,071 patients [2], 4,185 patients [3], 1,240 patients [4] and 113 patients [5] there were 50 (0.75%) accidental perforations of the spinal dura mater and no neurological sequelae. Probably, there should be an anatomical explanation for the absence of any neurological damage [6-8] (Figure 1).
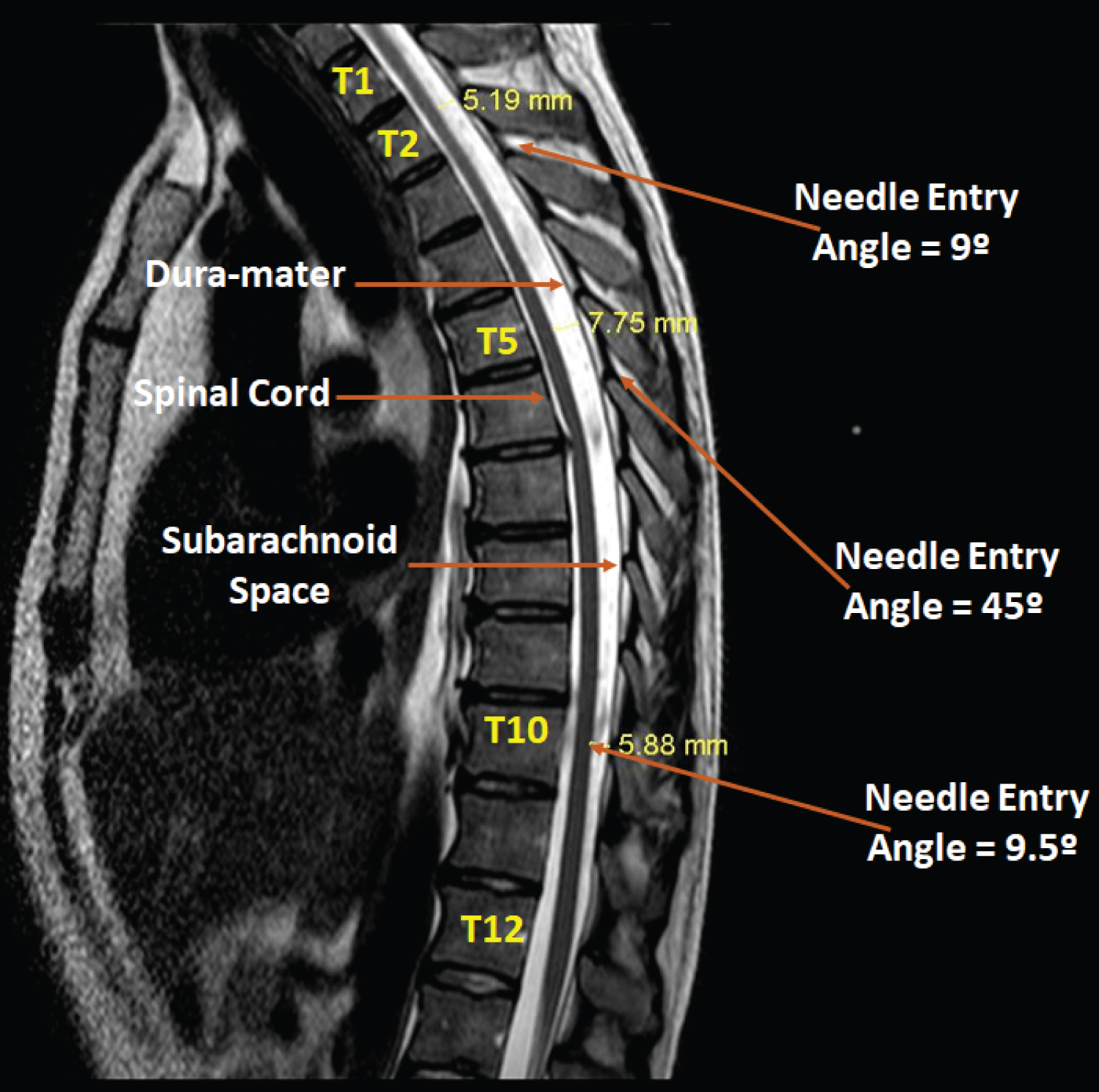 Figure 1: Magnetic resonance imaging of the spinal column.
View Figure 1
Figure 1: Magnetic resonance imaging of the spinal column.
View Figure 1
Studying a prospective single-blind study for low thoracic spinal anesthesia (T10-T11) in 300 patients undergoing elective surgery using pencil point needle and cut point needle, in the sitting or lateral decubitus position, showed that paresthesias occurred in 20/300 (6.6%) of patients, with no significant difference between needles [9]. This study showed that all paresthesias were transient, and no neurological deficits occurred in the thoracic puncture.
Laparoscopic cholecystectomy was compared using 15 mg and lumbar puncture with 7.5 mg of 0.5% hyperbaric bupivacaine plus 20 μg of fentanyl and thoracic puncture in 140 patients, showing that the low dose in thoracic spinal anesthesia has the advantage that it can be performed in ambulatory patients because of the earlier recovery of sensory and motor function and earlier discharge [10]. No neurological complications occurred when the thoracic puncture was performed.
Later in a prospective 636 patients of different types of surgery showed that thoracic spinal anesthesia with low doses of local anesthetic decreases the latency time, motor block and cardiovascular changes [11]. Paresthesia occurred in 39/636 (6.1%) patients with no difference between cut and pencil point needles, and similarly, the paresthesias were all transient without neurological sequelae.
In a recent narrative review on the role of thoracic spinal anesthesia in the 21st, the authors conclude that it is a technique not yet fully evaluated with a small spectrum of clinical indications, requiring further well-designed studies [12]. Aiming to perform opioid-free anesthesia, segmental surgery thoracic spinal anesthesia and sedation for breast and axillary was performed in four patients, showing that it is an alternative to general anesthesia, but requiring larger prospective studies [13].
Thus, a retrospective study in all patients undergoing thoracic spinal anesthesia was carried out in order to verify the incidence of neurological (paresthesia and neurological sequelae) and cardiocirculatory (bradycardia and hypotension) complications in various types of surgeries with different needles (cut and pencil point), with puncture between T8 and T11, in the sitting or lateral decubitus position, with insertion of the median or paramedian needle, and different solution of 0.5% bupivacaine (isobaric and hyperbaric).
The study was approved by the Ethics Committee (Number 5684/2009) and was a retrospective study carried out in several hospitals, where thoracic spinal anesthesia was performed between January 2007 and December 2019, all thoracic spinal anesthesia were recorded in an Excel spreadsheet for further study. Due to the fact that the study was retrospective, the Free and Informed Consent Term was released. The patients also were informed about risk of thoracic spinal anesthesia. All patients were classified as American Society of Anesthesiologists (ASA) Physical Status 1 and 2 and had no contra-indications to spinal anesthesia. Anthropometric data were collected as age, weight, height and sex.
Exclusion criteria were patients with previous thoracic spine surgery, patients with infection at the puncture site, clotting disorders, neurological disease, history of headache, hypersensitivity to amide local anesthetics, and refusal by the patient or family after a detailed explanation by the anesthesiologist.
All patients over 18 years of age who should receive spinal anesthesia for laparoscopic abdominal surgeries, herniorrhaphies, urological, gynecological and orthopedic surgeries were included in this study. This retrospective study of patients undergoing thoracic spinal anesthesia evaluated the following parameters: needle types, needle insertion, puncture position (sitting or lateral decubitus), thoracic puncture level, presence of cerebrospinal fluid (CSF) in the needle hub, type of anesthetic, latency, motor block, incidence of bradycardia and hypotension, paresthesia (duration) and neurological complications.
The pre-anesthetic evaluation was performed in all patients by the anesthesiologists of the service. All patients had fasting abbreviated from 2 to 4 hours after using 200 ml of maltodextrin. In the operating room (OR) all patients received peripheral venous access with a 20G or 18G catheter in the hand or forearm for infusion of Ringer's Lactate solution and administration of medication during the procedure. Monitoring consisted of electrocardiogram, pulse oximetry and non-invasive blood pressure was monitored. All patients received 3 L/min of oxygen through a nasal cannula. Before thoracic puncture with needles, patients received intravenously 1 μg/kg fentanyl and 1 mg midazolam. In femur fracture patients who had pain, inguinal plexus block was performed with HNS 12 neurostimulator with 2% lidocaine with 20 ml epinephrine and 20 ml 0.5% levobupivacaine. In patients where the block was not performed, 0.15/kg mg of dextroketamine was administered intravenously for placement in the puncture position.
After asepsis and skin antisepsis with 0.5% alcoholic chlorhexidine, the patients were placed in lateral decubitus or sitting position and the puncture was performed through the median or paramedian route, in the thoracic interspaces with a Quincke 27G or Whitacre 27G needle with a introducer. The presence of paresthesia, the appearance of cerebrospinal fluid and after injection of isobaric or hyperbaric bupivacaine in the dose depending on the type of surgery and the surgical team were evaluated.
Several types of surgeries were included in the study. All orthopedic surgeries were performed with 0.5% isobaric bupivacaine and the others with hyperbaric bupivacaine. In laparoscopic cholecystectomy surgeries, 20 μg of fentanyl and some gynecological and urological surgeries 80 mg of morphine were include. In the laparoscopy and gynecological surgery groups after spinal puncture and local anesthetic injection, all patients were placed in a 5-10° Trendelenburg position until the sensory level (tested for prick at 1-minute intervals) was reached T4. In orthopedic surgery patients after isobaric 0.5% bupivacaine injection, all patients were placed in 5-10° Trendelenburg position for 5 to 10 minutes, so that the blockage remains below T10. In patients undergoing herniorrhaphy or urological surgery after anesthesia injection of hyperbaric local anesthetic solutions the patients were placed in the supine position. In patients where anesthesia failed after thoracic injection, a new puncture was performed in the lumbar region and the patient would be excluded from the study.
The tip of the pencil-point and cut-point needles were evaluated to verify the length to enter the subarachnoid space, which allowed the appearance of CSF in the needle (Figure 2).
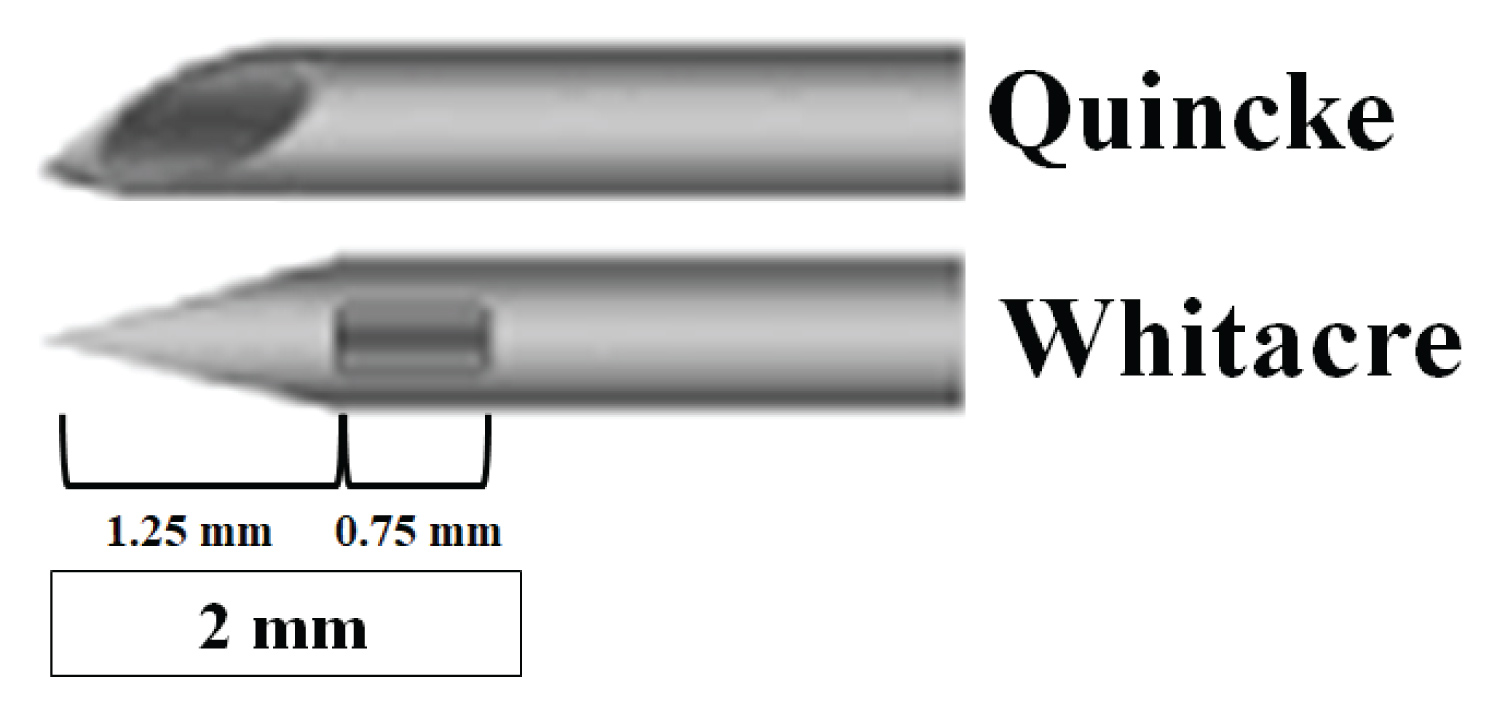 Figure 2: Evaluation of measurements in mm of the Whitacre needle tip. The Quincke needle tip is already the entry of the CSF.
View Figure 2
Figure 2: Evaluation of measurements in mm of the Whitacre needle tip. The Quincke needle tip is already the entry of the CSF.
View Figure 2
For comparison between groups was used Chi-square test (X2) and Fisher's exact test. To associate the dose with the motor block was used contingency coefficient. The level of significance throughout the study was 5%.
One thousand four hundred and six patients were studied and no patients were excluded (Figure 3). All patients developed spinal anesthesia, and there was no chest puncture failure. Demographic data are listed in Table 1. The surgeries performed and their quantities were: orthopedic (674 patients), laparoscopic cholecystectomy (505 patients), herniorraphy (130 patients), urologic (56 patients) and gynecologic (41 patients), making a total of 1,406 cases. The doses of both bupivacaine (isobaric and hyperbaric) used are in Table 2.
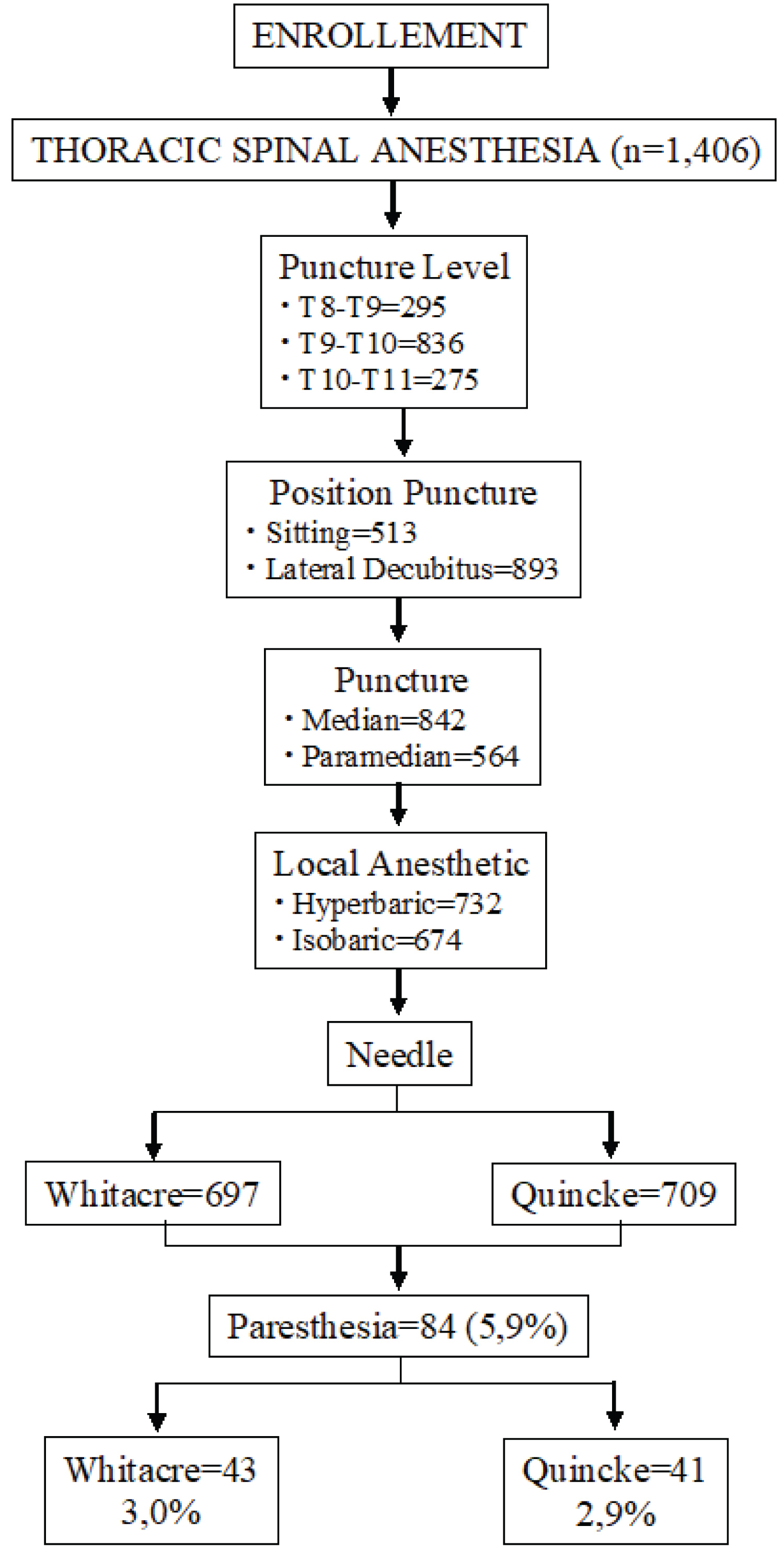 Figure 3: Consort flow diagram.
View Figure 3
Figure 3: Consort flow diagram.
View Figure 3
Table 1: Demographic data (m ± DP). View Table 1
Table 2: Doses of bupivacaine used in all patients. View Table 2
In all 1,406 patients, CSF appeared and the 1st drop was allowed to needle hub to confirm its correct positioning. Likewise, at the end of the injection, another drop was allowed to drip to confirm that the needle remained in the thoracic subarachnoid space.
The onset of sensory block ranged from 0:36 to 1:44 minutes, with a mean of 0:57 ± 0:00 minutes. Neither the dose nor the isobaric or hyperbaric solution of 0.5% bupivacaine affected the onset of sensory block. Addition of fentanyl to 0.5% hyperbaric bupivacaine solution did not change the onset of sensory block (0:57 ± 0:10 minutes).
Bradycardia occurred in 44 (3.1%) patients, 21 with hyperbaric and 23 with isobaric of 0.5% bupivacaine. Using Fisher's exact test showed that there is no significant association with the local anesthetic solution (p-value of 0.6461). Bradycardia occurred at all three punctured levels, and with all five doses used. Using the Chi-square test suggests that there is no significant association between bradycardia and puncture levels (p-value of 0.5633), and also in relation to the doses used (p-value equal to 0.471).
Hypotension occurred in 186 (13.2%) of the patients, 104 with the hyperbaric solution and 82 with the isobaric solution of 0.5% bupivacaine, with no correlation with the local anesthetic solution (p-value of 0.2707). Hypotension occurred at all three punctured levels, with the highest incidence at the T9-T10 level. There is a not correlation with the level of puncture and the incidence of hypotension. Hypotension occurred with all five doses used, without a significant correlation (p-value of 0.6481).
Forty-five patients (3.2%) did not present any degree of motor block in the lower limbs. Grade 1 motor blockade was observed in 424 (30.2%) patients, grade 2 motor blockade was observed in 466 (33.2%) of patients and grade 3 motor blockades was observed in 471 (33.4%) patients. The Chi-square test suggests a significant association between motor block and dose (p-value of 0.0000). The degree of association was the contingency coefficient, with a value equal to 0.701. In addition, the Chi-square test suggests a significant association between motor block and puncture level (p-value of 0.0000). The degree of association was the contingency coefficient, with a value equal to 0.23.
Paresthesia was observed in 84 (5.9%) of the thoracic punctures, 41 (2.9%) with the cut point needle and 43 (3.0%) with the pencil-point needle, with no significant difference. The duration of the pain complaint after paresthesia in the thoracic puncture was observed in six patients on the 1st postoperative day, three on the 3rd day and none on the 7th day of evaluation. In this way, all paresthesias were transient and without residual sequelae.
Studying the puncture position, it was observed that paresthesia occurred in 55 patients out of 893 with puncture in lateral decubitus, with an incidence of 6.1%, and in 513 patients with puncture in the sitting position, the incidence was 5.6%. There is no correlation between the puncture position and the incidence of paresthesia (p-value of 0.7276).
Comparing the median and paramedian puncture and the incidence of paresthesia it was observed that in 62 (7.3%) of the 842 patients with median needle insertion, while the incidence was observed in 22 (3.9%) of the 564 patients with paramedian insertion. There is an association between the incidence of paresthesia and needle insertion, showing that it is significantly lower in the paramedian insertion. Using Fisher's Exact test suggests that there is a significant association between insertion and paresthesia (p-value of 0.007982).
No patient who experienced paresthesia during thoracic puncture with both needles (cut and pencil point needles) complained of neurological symptoms at follow-up. No neurological complications were observed in the 1,406 patients who underwent thoracic spinal anesthesia, with a puncture between T8 and T11.
The results of this evaluation showed that the pencil point needle has a side hole and full size up to the end of its 2 mm hole. As the cut point needle the orifice is terminal there is no such doctor. The value of 2 mm is smaller than all the distances between the dura mater and the spinal cord (Figure 3).
Paresthesias are relatively common during spinal needle insertion in lumbar puncture, however, the clinical significance of the paresthesia is unknown. In this study with 1,406 patients undergoing thoracic spinal puncture between T8 and T11, paresthesia occurred in 84 (5.9%) patients, with a maximum duration of three days and without any postoperative neurological sequelae, and no severe cardiovascular complications. In all 1,406 patients, CSF appeared and the 1st drop was allowed to hub to confirm its correct positioning.
Studying 104 patients with pencil-point needle in lumbar puncture (25G Whitacre and 22G Gertie Marx) paresthesia occurred in 14/103 (13.6%) of patients, with one patient experienced two paresthesias, and all paresthesias were transient [14]. Thus, the incidence of paresthesia in our study (5.9%) with thoracic puncture was slightly less than half of the cases with lumbar puncture, justified by the presence of the cauda equina in the lumbar region and the large space between the dura mater and the spinal cord in the thoracic region [6-8].
Paresthesia during regional anesthesia is an unpleasant sensation for patients and, more importantly, in some cases it is related to neurological injury. Paresthesia is an abnormal condition in which patients feel a sensation of burning, numbness, tingling, itching or prickling. Although the etiology of paresthesia has not been precisely determined, the widely held conventional wisdom is that they result from needle to nerve contact.
In Letter to the Editor I agreed with Jonnesco [1], and concluded that cut point needles would be safer for chest puncture [15]. Pencil point needles have the side orifice and starts at 0.8 mm and ends only at 1.7 mm, so there is a need to penetrate into the subarachnoid space 2 mm for the CSF to appear [16]. Checking the measurements of the pencil point needle, we found a distance needed to enter the subarachnoid space above 2 mm. The cut point needle (Quincke) does not have this type of measurement because the needle opening is already at the point, and as soon as the point enters the subarachnoid space, the CSF immediately appears in the hub needle [17].
However, in this study with 1,406 patients, the incidence of paresthesia was the same with both the pencil point and the cut point needle. In most evaluations of our study with Magnetic Resonance Imaging (MRI) of the thoracolumbar spine, the mean distance from the dura mater to the spinal cord was 3.9 mm in the interspace of T2, 5.8 mm in T5 and 4.1 mm in T10 [6-8]. It is worth noting that the needle entry angle in these interspaces has a minimum angle of 9° and a maximum of 55°, increasing the distance and protecting the spinal cord [6-8]. This study showed that the need for penetration with a maximum of 2 mm of the pencil point needle in the subarachnoid space and perforating the meningeal of the spinal cord, did not occur any neurological sequelae by the protective effect of the pia mater [18]. As the cut needle has a terminal orifice, there is no study of this measure, found in the literature, or on the websites of several manufacturers.
The volume of CSF at thoracic levels is smaller compared to the volume in the cervical and lumbar region [19], and the thoracic nerve roots are more thin compared to the cervical and lumbar segments [20]. This explains the rapid onset of sensory block at around one minute. In this way, there is a lower dilution of the anesthetic solution injected in relation to the puncture site, and the roots are more easily blocked due to their small size, producing efficient blocking of these segments.
Studying the dura in cadavers it was noted that the dura was regularly pushed or “tended” up to 1 cm or more in front of the needle before the CSF could be seen in the needle hub, indicating dural puncture [18]. Similarly, the spinal cord was pushed ahead of the needle in cadaveric studies and was sometimes pulled back, but, due to the protective effect of the pia mater, rarely punctured [18]. Lateral puncture between C1-C2 for cervical myelography continues to be used in several institutions, and is considered within the standard of care by most neuroradiology programs nationwide [21].
In a previous study, doses of 5 to 10 mg of hyperbaric or isobaric 0.5% bupivacaine, provides a rapid onset of action, lower incidence of motor block, and caused minimal cardiocirculatory changes [11]. In this study with isobaric and hyperbaric solutions of 0.5% bupivacaine and doses ranging from 5 to 15 mg, the incidence of bradycardia was 3.1% (44 patients), and the incidence of hypotension was 13.2% (186 patients). Both bradycardia and hypotension were easily treated with a dose of atropine or a vasopressor.
The group from Italy started using continuous thoracic spinal anesthesia for surgeries in elderly urology and abdominal surgery patients with excellent results [22-24]. Finally, in an editorial, the authors defend that thoracic spinal anesthesia: an interesting alternative to general anesthesia [25].
All 84 paresthesias observed in this study were associated with free flow of CSF when the stylet was removed from the needles, with short duration of pain and transient. This study showed, once again, that no association was found between the type of spinal needle and the incidence of paresthesias. The most important result of this study with 1,406 patients is to confirm the results of Jonnesco [1] in 1909, and several other studies showing that the thoracic spinal anesthesia is a feasible procedure and showed no neurological sequelae [9-11]. The low incidence of paresthesia allows us to state that spinal thoracic anesthesia is safe with both needles, against what has already been said in another study in the lumbar region which neurological damage followed spinal or combined spinal-epidural anesthesia using an pencil point needle [26].
If the anesthetist has an adequate knowledge of the relevant modern anatomy, physiology and pharmacology, safe and satisfactory anesthesia can easily be obtained to the mutual satisfaction of the patient, surgeon and anesthetist. Thoracic spinal anesthesia represents all this knowledge. I have always been teaching the various techniques of spinal anesthesia. It's just what I've been doing for many years, but the technique is just a means and not the end. Think about the story and what story we want to tell. If you don't have a story to tell, you have no reason to teach, and nor research spinal anesthesia.
No financial sources supported this work.
No competing financial interests exist.