Healthcare workers at the forefront during the COVID-19 pandemic faced increased workload and stress. Young doctors who are training in Anesthesiology and Reanimation residency are one of the groups most exposed to this condition. Increased stress load; may impair the mental and physical health of the doctor, causing burnout syndrome. The aim of this study is; To evaluate the anxiety levels, being affected by individual stressors and coping methods before and during the pandemic of the doctors who continue their training in anesthesiology and reanimation residency.
Since asking questions is the best way to understand the issues that health professionals are most worried about, the study was prepared as a questionnaire form. The questions in the study were divided into 4 main categories: Demographic information, Stressor factors rating, Perceived Stress Scale (PSS) and Coping methods. Doctors were asked to fill in the questionnaires individually.
The study was performed in Ankara City Hospital, Turkey. 49 male, 24 female Anesthesia and Reanimation residents participated in our study. There was no difference in terms of demographic data and weekly working hours. Group rates were found to be close to each other in each seniority group. A strong positive correlation was found between residents' pre-intensive care working (ICU) values and their values during ICU working (r = 0.631; P = 0.001). This correlation was also at similar levels between seniorities (p > 0.05). When evaluated in terms of coping methods, it was found that the residents most frequently used the strategies of accepting, focusing on the problem and planning, regardless of gender discrimination.
Burnout occurred more frequently and differently from previously reported situations among healthcare professionals working during the COVID-19 pandemic. Common and high workload, work stress and time pressure, protective equipment and organizational factors; while increasing stressors for anxiety, it also changed perception levels and coping methods.
COVID-19, Anesthesiology residency, anxiety, perception of risk.
During the residency training of young doctors who have just graduated from medical faculty, learning and applying the information in practice is a time-consuming process.
The fact that anesthesia and reanimation education has a wide field that includes many disciplines is a situation that increases the skills of anesthesiologists. At the same time, anesthesiologists play important roles as the leader of the rescue and decision-making team during both natural and man-made disasters [1]. A doctor may experience burnout at different stages of her /his career, most often during her/his residency training [2].
Many countries around the world have been exposed to the pandemic of the new coronavirus (COVID-19). During the COVID-19 pandemic, healthcare professionals working at the forefront may face increased workload and stress. Understanding and supporting the burnout risk of healthcare workers is very important to maintain the quality of healthcare services during the pandemic. Resident doctors, who are trained in hospitals under normal conditions, experience stress in their daily lives due to long working hours, heavy workload, night shift, insufficient time for sleep, food and training [3]. Indeed, stress can have beneficial effects when faced with an appropriate cognitive approach and adequate coping strategies [4]. The ability to deal with challenging situations can increase doctors' confidence. Some medical specialities are at high risk of psychological stress. Anesthesia residents are also one of the groups with high stress levels. The management of life-threatening scenarios may cause this situation, as patient follow-up in anesthesia operating rooms causes mental fatigue. It is not surprising to find a high incidence of burnout among healthcare professionals working as anesthetists. In a cross-sectional study conducted in 2016, it was found that 40.1% of consultant anesthetists and 52% of resident doctors were psychologically distressed [5].
However, as in the pandemic period, the increased stress load can damage the mental and physical health of the doctor and cause burnout syndrome [6]. Previous studies examining psychological responses during past infectious disease outbreaks, such as SARS (Severe Acute Respiratory Syndrome), have shown relatively high psychological morbidity among healthcare workers [7]. Resident doctors are a significant part of the healthcare professionals responding to the COVID-19 pandemic internationally. During the current pandemic; It is unclear how factors such as the seniority of resident doctors and exposure to high-risk areas affect the psychological and coping responses of resident doctors.
The aim of this study; To learn and evaluate the anxiety levels, the level of being affected by individual stressors, and coping methods before and during the pandemic of the doctors who continue anesthesiology residency.
After the approval of the ethics committees of Ankara City Hospital and Ministry of Health of Republic of Turkey, 73 resident doctors actively working in the intensive care unit during the pandemic process were included in the study. Doctors who did not work in intensive care were excluded from the study Young doctors were asked to complete the questionnaires individually. Since asking is the best way to understand what healthcare professionals are most worried about, the study was prepared in a questionnaire form.
The questions were divided into 4 main categories in the study:
1. Demographic information (age, gender, weight, height, marital status, comorbid illness, drugs used continuously, smoking and alcohol consumption, job (profession) and speciality satisfaction and weekly working hours)
2. Determination of stressors
3. Perceived Stress Scale (PSS)
4. Coping methods (strategies)
The frequency and severity of stressors specific to intensive care units were graded using Likert-type scales [8]. The Likert scale is a closed-ended psychometric questionnaire that measures the participant's views on a series of statements. Likert scales are frequently used in questionnaires because they have a determining feature of participant views. Instead of marking the expressions that they adopt, the individual who takes the attitude scale determines the extent to which he agrees with each statement [9-10].
The Perceived Stress Scale (PSS) is the most commonly used 10-question psychological stress test to measure perception. The questions are designed to assess how participants find their lives unpredictable, uncontrollable, and overloaded. The scale also includes a series of direct queries about current experienced stress levels. The items are easy to understand, and answer alternatives are easy to grasp.
Responses were asked to be rated as Never: 0 Almost never: 1 Sometimes: 2 Less often: 3 Very often: 4.
The scores for questions and change the scores as follows: 0 = 4, 1 = 3, 2 = 2, 3 = 1, 4 = 0 is reversed.
Points are added up for each item to get a total. Individual scores range from 0 to 40, with higher scores meaning higher perceived stress.
* Scores ranging from 0 to 13, low stress,
* Scores ranging from 14-26, moderate stress,
* Scores ranging from 27-40 are considered high perceived stress.
The coping attitudes assessment scale is a self-report scale designed to evaluate the coping attitudes people use in the face of difficult situations in their lives. Developed by Carver and Scheier in 1989 under the name of COPE inventory (The Coping Orientations to Problems Experienced scale), it was introduced to our language as Cope (Coping Attitudes Assessment Scale) in 2005 Agargun et al. translated and validity and reliability study has been done by (10). No questionnaire responses were excluded from the study.
Data suitability to normal distribution was tested with Shaphiro wilk. Student t test was used to compare normally distributed characteristics in two independent groups, and Paired t test was used to compare measurements made before and during intensive care working. Mann Whitney u test was used to compare non-normally distributed properties in 2 independent groups. In addition, one-way analysis of variance (ANOVA) and LSD multiple comparison tests were used for properties showing normal distribution in comparison of numerical data in more than 2 independent groups. Kruskal Wallis test and All pairwise multiple comparison test were used for non-normally distributed properties. Relationships between numerical variables were tested with Pearson's correlation coefficient. Cronbach alpha coefficients were calculated in order to test the validity and reliability. As descriptive statistics, mean ± standard deviation for numerical variables, number and % values for categorical variables are given. SPSS Windows version 23.0 package program was used for statistical analysis and P < 0.05 was considered statistically significant.
49 male, 24 female Anesthesia and Reanimation residency doctors were participated in our study.
Demographic data and weekly working hours are given in Table 1. Descriptive statistics of categorical variables are given in Table 2. In the second table, the results of the answers given by the participants to the questions of gender, seniority, marital status and number of children, medications used if there are comorbidities, alcohol and cigarette consumption, and specialization and professional satisfaction were evaluated.
Table 1: Descriptive statistics. View Table 1
Table 2: Descriptive statistics of categorical variables. View Table 2
It was determined that the number of participants among the seniority groups was close to each other. It was determined that the occupational satisfaction of the physicians who received training in the residency of Anesthesia and Reanimation was 65.8%, while the specialty satisfaction was 82.2%. It was observed that the rate of cigarette consumption was 21.9%.
In the Covid -19 pandemic period, resident doctors of all seniority who were assigned very quickly in intensive care units; They were asked to evaluate the positive or negative situations (self-criticism) when they evaluated themselves in terms of their education level during their working period. When they evaluated the procedures they learned during the residency training, they reported that they encountered very few procedures they did not know (6.8%) during the pandemic process. When they evaluated their positive or negative mistakes, the results were found to be pleasant. During this period, it was determined that they were sometimes worried when approaching patients with a definite diagnosis of Covid -19.
A strong positive correlation was found between residents' pre-intensive care (ICU) values and their values during ICU working period (r = 0.631; P = 0.001). This correlation was also at similar levels between seniorities (p > 0.05). A moderate positive correlation was determined between residents' pre-intensive care stressor scale values and perceived stress scale values during intensive care unit working period (r = 0.401; P = 0.001).
The stressor value (50.24 ± 9.71) of men during intensive care working period were statistically significantly higher (p = 0.001) compared to the pre-intensive care values (46.29 ± 9.82). The stressor values (49.88 ± 9.97) of residents with seniority level 1 and 2 during intensive care working period were significantly increased compared to pre-intensive care values (p = 0.018). There was no statistically significant difference in the evaluations of the residents with a seniority level of 3 or more (p > 0.05).
It was observed that stressor responses of single residents increased statistically significantly compared to married residents. It was observed that the stressor values of the residents who did not have children during the intensive care unit (49.57 ± 9.55) were statistically significantly higher than the pre-intensive care values (45.55 ± 9.98) compared to the residents who had children (p = 0.001).
For residents who do not use drugs or medications, do not smoke or use alcohol and resident doctors who satisfied with their profession but not satisfied with the specialty branch; It was observed that stressor perception values during intensive care working period increased statistically significantly compared to pre-intensive care values (p < 0.05) ( Table 3).
Table 3: Examination of perceived stress scale scores with demographic characteristics. View Table 3
When the men and women were evaluated separately, it was observed that the PSS (perceived stress scale) values during the intensive care unit working period (24.57 ± 4.38) were statistically significantly higher than the pre-intensive care values (22.08 ± 4.63) (p = 0.001). However, it was observed that PSS values were higher in men than in women before intensive care (p = 0.001). However, values during intensive care working period were observed to be similar between genders (p > 0.05). It was observed that the PSS values (24.56 ± 3.37) of residents with a seniority of 1, 2 and 3 during intensive care working period were statistically significantly higher than their pre-intensive care values (20.94 ± 4.95) (p = 0.001). PSS values of those with or without children were similar. However, their values before and during intensive care were significantly different. Being single or married didn't make any significant difference either. The effects of comorbid illness, medication use, smoking and alcohol use on PSS values were similarly increased. Similarly, no difference was found between the individuals who were satisfied with the profession and the branch and those who were not.
When evaluated in terms of coping methods, it was found that the residents most frequently used the strategies of accepting, focusing on the problem, and planning, regardless of gender discrimination (Figure 1).
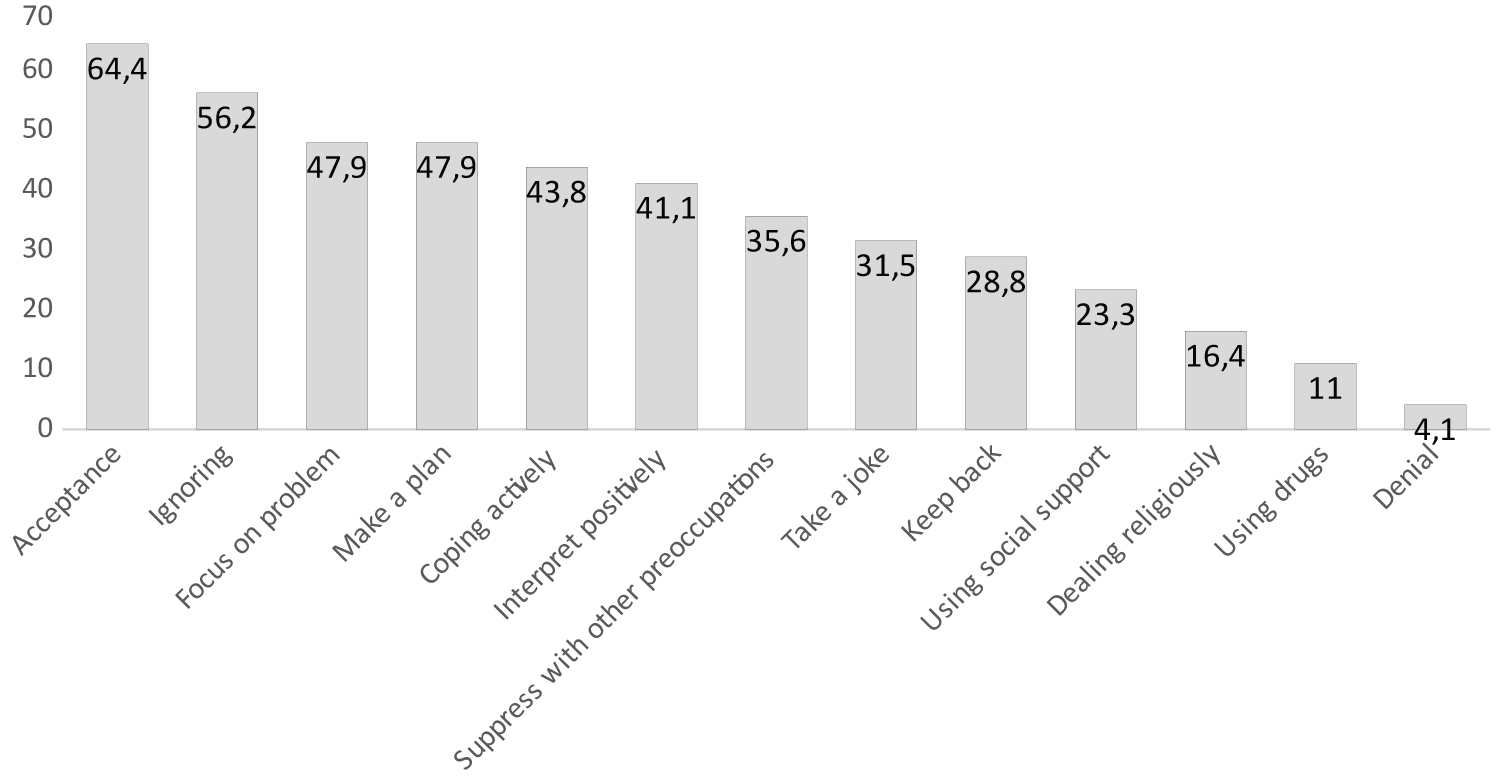 Figure 1: Evaluation of coping methods
View Figure 1
Figure 1: Evaluation of coping methods
View Figure 1
When the relationship between the gender of residents and their methods of coping with stress was examined, it was observed that the rate of denial as a method of coping with stress in women (12.5%) was statistically significant compared to men (p = 0.011). Acceptance as a method of coping with stress was observed at a statistically significantly higher rate in males (73.5%) than females (45.8%) (p = 0.021).
During the pandemic, residents from different seniorities working in the anesthesia clinic (operating room) were assigned to work in intensive care units.
In this cross-sectional study conducted at the stage where the COVID-19 pandemic was intense, it was found that the stress level of our clinic anesthesia resident doctors was not related to the time they spent in residency training. Some studies in the literature stated that young doctors are exposed to stressors at a higher level than more senior doctors [11-14]. In a review article by Downey et al. stated that young doctors' perception of exposure to stressors is lower than their experienced colleagues [15].
Unfortunately, the articles about the effect of age and experience on burnout syndrome do not contain a common result. Anesthetists with less experience may feel less responsible while continuing their work than senior residents who are involved as consultants. They can also be stressed and less confident in managing difficult scenarios on their own, such as difficult airways, cardiac arrest, and other emergencies. In a study by Chewv, et al. In which they evaluated the psychological states of residents and their methods of coping with stress without making clinical discrimination in a training hospital during a pandemic in Singapore, they did not find any difference between newcomers and experienced residents in terms of anxiety perception [16]. In addition, such a large pandemic is a special case, unlike other studies in which anxiety, stress perception and coping methods were evaluated on health professionals before the pandemic period. Regardless of seniority, all residents doctors have faced the unprecedented situation for the first time in recent years. In a study of 1244 cases in which Alrubaiee, et al. Evaluated the anxiety levels of healthcare workers working in the foreground against covid-19 in Yemen; They found that age and gender did not make a significant difference in perception of stress [17-19].
They found similar results to Alrubaiee, et al. in their evaluations on healthcare workers during the corona pandemic period in Vietnam and Iran, respectively. Regarding gender, Chiron, et al. in a study conducted on French anesthetists before the pandemic period reported that women were more exposed to burnout [13]. In another study evaluating German anesthetists, no relationship was found between gender and burnout [5] Shams, et al. In their study among anesthesiologists who pursued an academic career in Egypt, found a higher burnout risk in men [20]. China, Italy and some researchers in Turkey have reported a higher level of anxiety and depression in women health care providers during Covid-19 outbreak [21-23]. In our study, the level of being affected by stressors during intensive care working period was found to be significantly higher among male anesthesia resident doctors.
Personal lives of doctors (such as marriage and having children) can also affect the level of burnout and perception of anxiety. In three different studies in the literature, it was determined that the marital status of healthcare workers was not associated with burnout [14,24,25]. Only Shams et al found in their study that personal life affects the perception of anxiety [20]. In our study; It was determined that the stressor exposure of single (not married) resident doctors while working in the intensive care unit was statistically significantly higher than their condition before working in the intensive care unit. However, when evaluated in terms of individual stress perception scale, it was found that the scale scores of married and single doctors were similar. On the other hand, Morais, et al. Showed that having a child is among the factors that change the perception of stress [11]. This situation was interpreted as the difficulty of coping with family duties while at the same time being exposed to an important workload. In the study of the Yeni Elbay, et al. It was shown that having a child is associated with lower levels of anxiety and depression [23]. In our evaluation, the level of being affected by stressors of residents who do not have children; During the intensive care working, a statistically significant increase was observed compared to the values before the intensive care working. Having a child was thought to be protective against stressor effects.
The effects of weekly working hours on burnout have been the subject of many studies in the literature. De Oliveira Jr. et al. reported that increased workload (70 hours per week) of physicians working during anesthesia training was associated with a higher incidence of burnout and depression [24]. Similarly, Rui, et al. showed that working over 60 hours per week independently resulted in high depersonilization and low coping methods [26]. In an evaluation conducted on Portuguese anesthesiologists, they stated that the main factors that produce stress are excessive workload, undisciplined surgeons, lack of adequate working conditions (insufficient resources, lack of auxiliary staff) and technically challenging situations (e.g. airway management) [11]. Brazilian anesthesiologists have reported that working hours in night shifts are the most common factor causing burnout syndrome [25]. Our anesthesia resident doctors working in our intensive care unit worked 84 hours a week.
Burnout can negatively affect health systems at different levels, resulting in low patient safety and quality of care. Because; fatigue prolongs reaction time to events encountered, may cause memory problems and inability to make decisions. As a result, it can lead to high risk mistakes by affecting individual work performance [27]. For example, in a study by Okell, et al. It was found that dural puncture is more common during epidural anesthesia attempts performed between midnight and 6 am [28]. In our study; When our resident doctors who exposed to various stressors evaluate their own performance; We found that 52.1% made very few mistakes with no negative consequences. It was determined that 11% did not make any mistakes. It was seen that no resident doctor chose the “I often made mistakes” option.
When evaluated in terms of patient care and time management, our resident doctors; 43.8% and 49.3%, respectively, stated that they had trouble sometimes. 47.9% of our resident doctors said that they often followed the patients well, and that they were supported by specialist doctors in matters that they felt insufficient.
It is a fact that sudden changes in life and work programs during the pandemic have a stressor effect on our resident doctors. At the same time, encountering procedures they did not implement more frequently due to their insufficient seniority has also been a source of stress. In our study, we determined that 31.5% of our resident doctors performed procedures “very rarely” that were not available in their training. It was determined that 6.8% saw different transactions. Of course, we think that many interventional procedures are included in the anesthesia core program, which is effective in this low rate among anesthesia residents.
While working in intensive care units under normal conditions can cause anxiety, depression and burnout alone, it is not a surprise that the approach to pandemic patients with high contagiousness will increase this level. 42.5% of our resident doctors stated that they sometimes experience anxiety when approaching patients, and 24.7% very rarely. The rate of resident doctors who did not experience any anxiety was 1.4%.
People who are exposed to stress use various coping methods to restore their mental balance. These methods are also defined as cognitive and behavioral efforts [29]. Lazarus and Folkman reported that coping is a dynamic process and changes during stressful interactions between the person and her/his environment [30]. In dealing with stress, people generally use three strategies. These are problem-focused, emotion-focused, and thought-focused coping methods [31]. Most of the participants in our study preferred the “acceptance” method (64.4%) as a strategy to cope with stress. This was followed by methods of ignoring (56.2%), focusing on the problem and planning (47.9%), respectively. The denial method (4.1%) was the least preferred method. When the relationship between gender and methods of coping with stress was examined, a different result was observed in women with a rate of denial (12.5%), while this method was never used in men. In men, acceptance was statistically significantly higher than in women.
As an expected result, as a method of coping with stress for resident doctors who have no job satisfaction; The percentage of preferring the denial method was higher than those who were satisfied. Methods of coping with stress were evaluated as similar in differences in marital status, smoking, alcohol and medication use. It is an important point that the greatest concern of the physicians participating in the study and the best anxiety relief measure relates to having adequate protective equipment. Having a sufficient amount of protective materials and equipment in our hospital has completely eliminated this concern.
Our study, which evaluated their anxiety levels before and during the pandemic, and methods of being affected by individual stressors and coping methods, had limitations. The pandemic process is still continuing. Resident doctors are rested at regular intervals and reassigned in intensive care units. Therefore, it was not possible to determine the level of influence of the resident doctors after the intensive care work. Relating the concept of pandemic to burnout was a new issue. Increased workload and duration, time pressure, maintaining a new normal order increased stressors for anxiety and changed perception levels and coping methods. As a result, the incoming articles on this topic from different parts of the world, we wanted to add the research we did on doctors working in anesthesia residents in Turkey.