Artificial Intelligence (AI) will change our lives beyond recognition, it will have a far bigger impact than the internet or mobile technology. We are now at the threshold where machine intelligence is comparable with human intelligence, in certain limited aspects, for the first time in history. Enhancements in technology, both software and hardware, have resulted in some human decision-making being inferior to, and more erratic than, AI in many fields, including medicine. However, it is widely accepted that rather than compete with machines, using AI to support and help make better informed decisions is the key to future medicine. In areas like anaesthesia, AI can be used to develop useful advanced clinical decision support tools based on machine learning.
Anaesthesiology, Machine learning and Pain management
Anaesthesiologists need to identify high-risk patients and optimize their fitness both for surgery and post-surgical care in order to promote and enhance recovery. Other factors include major trauma, resuscitation, airway management, and critical emergencies that pose an immediate threat to life. Anesthetics influence in patient care is essentially three phase, pre-operative, interoperative and post-operative (Figure 1). In the per-operative phase the aim is assessment of the patient's surgical and anaesthetic preoperative morbidity and mortality. It is essential to acquire as much information from the patient as possible in order to achieve the best outcome.
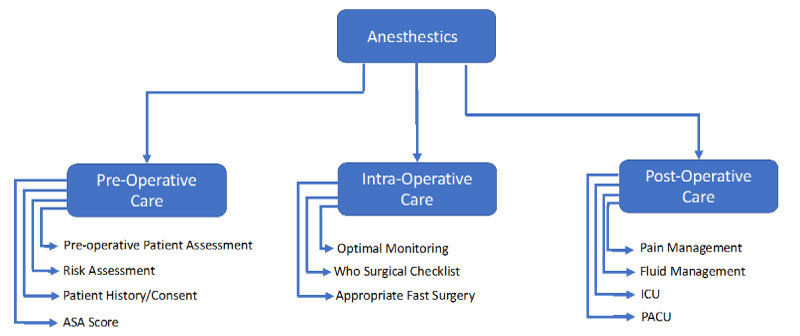 Figure 1: Role of anesthestics.
View Figure 1
Figure 1: Role of anesthestics.
View Figure 1
The American Society of Anaesthesiologists (ASA) has proposed a widely-accepted classification scheme to aid pre-operative assessment. However, it is quite subjective, and is prone to varying interpretation based on the type of surgery, patient's age (Geriatric or Young), anaemia, obesity, etc. The correlation of ASA scores with operating times, hospital length of stay, postoperative infection rates, overall morbidity and mortality rates following various different surgery has been extensively studied [1-4] Table 1.
Table 1: ASA classification score. View Table 1
Interoperative anaesthetics involves the patient monitoring and drug control management during surgery. It requires very accurate and controlled doses of drugs to be administered in a timely fashion. Any errors in any aspect of the process are extremely dangerous. Target-controlled infusion (TCI) is part of anaesthesia delivery in many countries, resulting in the precision, reliability, efficacy, and safety of intravenous (IV) anaesthesia delivery. Advancement in drug development has primarily modifying the chemical structures of existing drugs to improve their pharmacodynamic, pharmacokinetic, and side effect properties [5].
Monitoring of depth of anaesthesia during surgery is subjective and depends on the patient's ASA classification and the surgery type to allow accurate drug administration against the measured state of arousal of the patient. The patient's sensitivity may vary throughout the surgical procedure, and the haemodynamic effects of the drugs may limit the amount that can be given safely.
As it is desirable to minimize anaesthetic drug dosage during surgery, another potential complication is under dosing, which can result in a patient become aware during an operation (i.e., insufficient depth of anaesthesia, DoA). Quite apart from the inherent undesirability of this, it can lead to serious adverse physiological reactions. It may arise due to equipment failure, or due to misjudgements by the anaesthesiologist. Conversely, inappropriate titration of the hypnotic components, leading to excessive DoA), may also compromise patient outcome [6,7].
Post-operative care of patients who have received anaesthesia is conducted in a post-anaesthesia care unit (PACU) prior to discharge. However critically ill patients are normally monitored in the intensive care unit (ICU), Intensive care requires support for numerous possible medical interventions: Cardiovascular instability, airway or respiratory compromise, acute renal failure, or multiple organ dysfunction syndrome. Medications used to treat chronic painful conditions need to be carefully monitored and most medications have significant side effect profiles [8,9].
The goal of developing an automated anaesthesia system is not new, the earliest efforts dating to 1950 when Bickford described a system for monitoring and maintaining aesthetic depth based on summing electroencephalography signals. Other, more complex successors have emerged, (e.g., McSleepy), but all are clear descendants of Bickford's closed-loop feedback control system. Characteristic of all these systems is the structure of the controller, invariably based on a large set of carefully hand-crafted rule and response algorithms that attempt to maintain the target variable (depth of anaesthesia) around a set point Figure 2. Modern systems typically use a reliably quantifiable target measure as input, such as bispectral index, rather than electroencephalography, but the overall structure remains the same [7,10].
 Figure 2: McSleepy control loop for anaesthesia in surgery.
View Figure 2
Figure 2: McSleepy control loop for anaesthesia in surgery.
View Figure 2
Such systems have not been without their successes: McSleepy has been providing automated anaesthesia since 2008, and recently has worked with DaVinci, a robot surgeon, in the first all-robotic surgery on a prostatectomy patient at the Montreal General Hospital. However, it is difficult to generate by hand the rules needed for such robot anaesthetists to handle complex scenarios as well as simple ones, this has proved to be the Achilles' heel of all such systems to date; it is difficult, perhaps intractable, to scale them to match human performance. Once a certain degree of complexity is evinced in a problem, rule-based algorithms fail to equal the ability of a suitably skilled human to perform the task. Consider, for example, the Sedasys pharmacologic robot from Johnson & Johnson. It was designed to control the hypnosis and analgesia domains using several closed-loop feedback systems including algorithm-based calculations of standard vital sign data inputs as surrogate measures of depth of anaesthesia. Despite much fanfare upon its approval by the Food and Drug Administration, it was pulled from the market in 2016 due to dismal sales [11].
There is, however, an alternative approach to the problem of automating anaesthesia, to take advantage of the rapid growth in capability of so-called learning algorithms, the study of which is currently an area of explosive growth in the field of Artificial Intelligence (AI). These algorithms have the ability to learn from experience, or, more prosaically, to be "trained" to perform a task by being shown a large set of example inputs to a problem and the desired responses of the system. So, in an anaesthesia machine, the controller would be trained by example on a large number of sample cases of control inputs (e.g., bispectral indices) and desired set point values. So, in contrast to the so-called "top-down" approach of handcrafting control rules, a system is "trained" or "grown" in a "bottom-up" manner. The key advantage of this is that nothing is missed, it is possible for the system of absorb all the information implicit in the training data and automatically condense an appropriate "rule-set" that captures the detailed statistics of the inputs, something that top-down designers find very difficult to do.
Surgery is a very stressful condition with severe sympathetic stimulation, HTN, tachycardia, arrhythmias. Most drugs used for general and regional anaesthesia cause homodynamic instability, myocardial depression, hypertension and arrhythmia. Under general anaesthetic the patient maybe hypo or hyperventilated and may develop hypothermia. Blood transfusion maybe required due to anaemia and hypotension. Intraoperative monitoring is essential to maintain the normal patient physiology and homeostasis throughout anaesthesia and surgery. The term "standard monitoring" defined by ASA refers to pulse oximeter, electrocardiography, noninvasive blood pressure and temperature monitoring [12].
A major issue with current deep learning systems is "opacity." Although a machine may be trained to perform a specific input-output mapping, it is often unclear as to which part of the training network is responsible for any specific outcome. This is undesirable, as physicians need to understand and trust the operation of any autonomous anaesthesia system.
A subcategory of Machine Learning (ML) is so-called Deep learning, which is a computational structure that attempts to mimic the architecture of the human brain. This structure is the Artificial Neural Network (ANN), comprised of "layers" of simple elements (mimicking neurons in the cerebral cortex) connected in a network structure. The recent dramatic breakthroughs inability of AI are almost wholly attributable to advances in computer hardware that have made much larger ANNs (i.e., "deep nets") feasible [13] Figure 3.
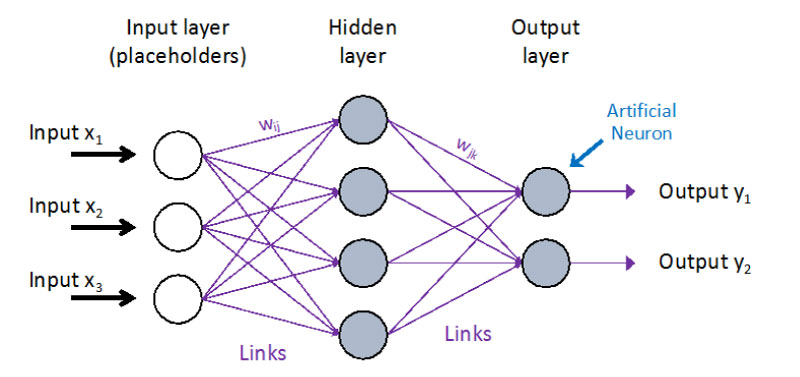 Figure 3: Basic neural network design.
View Figure 3
Figure 3: Basic neural network design.
View Figure 3
The difficulty of AI and machine learning models is the classifier and training dataset used. High performance is essential to minimizes the prediction error, this directly relates to having a large dataset. The obstacle to AI implementation in healthcare is not technological but access to large amounts of data. Research is hampered by difficulties in accessing large medical datasets, for legal or other reasons.
Training and Building of Neural Network.
AI Benefits are life changing from a clinical perspective. Humans in some aspects are bad at making decisions and this is where machines excel.. in terms of speed, reliability and repeatability. AI machines are very good at pattern matching, so are ideal for applications in image recognition such as melanoma and cancer diagnosis. AI can also be used to search and currently information in extremely large databases provided clinicians with a accurate and useful information Figure 4.
 Figure 4: Neural Network (Multi-layered).
View Figure 4
Figure 4: Neural Network (Multi-layered).
View Figure 4
As information progresses from left to right in the picture, successively more complex abstractions of the input data are formed, finally achieving the desired output on the right. It can be seen that the network is organised in "layers", a modern "deep" network can have hundreds of such layers. The system "learns" by employing mathematical optimisation algorithms (e.g. "back propagation") to automatically adjust the parameters of each layer (the so-called "weights") to achieve the overall function of the system based on the training examples given. Key to the whole system is that the detailed behaviour is not programmed, instead is developed by the optimisation algorithm based on the supplied training data [14].
Figure 5 shows the use of a neural network in the control loop of an automated anaesthesia system. It is immediately clear that the system shows marked similarities to the classic McSleepy approach, the only real change is to replace the McSleepy controller with an Adaptive Neural Network. This is the key point, the McSleepy controller contains an extensive hand-crafted set of rules, generated by a human programmer in consultation with human anaesthesiologists (a typical example of 1980s'-90's "Knowledge Engineering". The proposed system, on the other hand, is not programmed in this sense at all. Instead, it is "trained", by exposing it to an extensive set of example "inputs" and "desired outputs". These data are generated by logging all the data from a large number of real operations carried out in the past, under the supervision of human anaesthesiologists. Using a neural network training algorithm, the system learns to map the inputs into the desired output responses. The advantage of this approach is that it does not rely on introspection, there is no "human in the loop" (i.e. programmer) attempting to rationalise what is happening, instead the system automatically learns the desired set of responses. In a technical sense, the system is learning the statistics of the input patterns and mapping these to the desired responses. It "learns by imitation", finding mapping that mimic the actions of all of the human anaesthesiologists whose operations were monitored to acquire the training data. As it learns by observing the decisions of many human anaesthesiologists, it may well achieve behaviour equivalent to that of an individual anaesthesiologist.
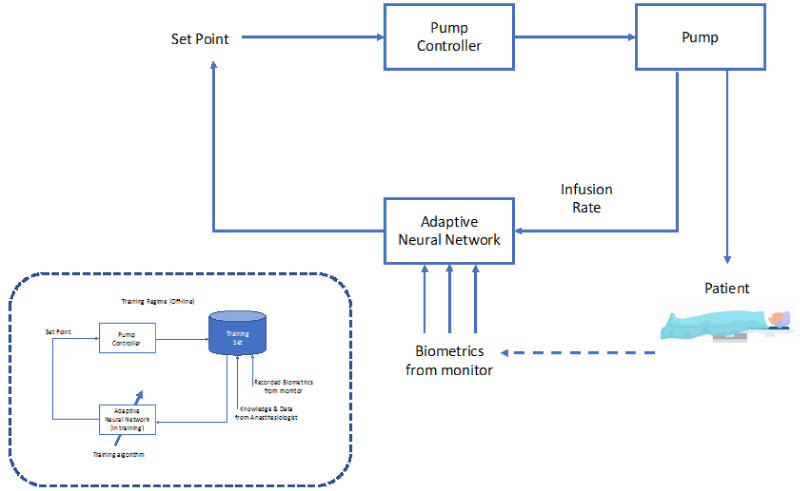 Figure 5: Adaptive neural network control loop for anaesthesia in surgery.
View Figure 5
Figure 5: Adaptive neural network control loop for anaesthesia in surgery.
View Figure 5
Technological advancement has made robots an integral part of several fields, including surgery. Pharmacological robots are closed-loop systems, able to precisely titrate the dose of anaesthetic drugs to a preset value, concerning hypnosis, analgesia and neuromuscular block. Mechanical robots automatically reproduce manual tasks, showing promising performance. Decision support systems can improve clinical practice. The use of robots in anaesthesia shows the advantage of eliminating the repetitive part of the workload, allowing the anaesthesiologist to focus on patient care.
The neural network system unlike McSleepy and other closed loop control systems which are rule based, used large data sets to train AI system. Difficulty is the requirement of very large data set. For these AI systems to play a future in the vast amounts of data generated by monitoring systems are used database.