The answer to this title question is simple. Get a correct diagnosis. In order to improve your recovery from any whiplash case, soft tissue injury with no objective medical findings, or a cervical sprain, there are several easy steps a trial attorney can follow. First and foremost is to obtain an accurate diagnosis.
Often, a trial attorney has a client who has been rear-ended, suffered a hyperextension hyper flexion injury, as normal X-rays, MRIs, and CAT scans, and has had numerous sessions of physical therapy and/or chiropractic care. The treating physician tells the trial attorney "I can't find anything wrong. It must be cervical sprain or strain." Nothing could be further from the truth. Johns Hopkins Hospital physicians report that 63% of these patients need surgery to improve [1].
It is important to understand the mechanics of a rear end collision. Even with restraints, and head-rest, the 20 pound ball sitting on top of the neck (the head) is first thrust backwards, and then forward. Additionally, the chest either hits the steering wheel, or is compressed by the airbag, and often the seat-belt dislocates the 10 th rib.
These motions result in a consistent pattern of injuries, which are often overlooked by treating physician, and more importantly, are not readily detected by X-ray, MRI, or CAT scan.
These injuries are:
1) Post concussion syndrome
2) Torn ligaments in the cervical spine, producing either spinal instability, or a damaged discs
3) Thoracic outlet syndrome
4) Temporomandibular joint syndrome
5) Tietze’s syndrome
6) Slipping rib syndrome
Each of these syndromes can be clinically detected by a thorough history, and physical examination, and, more importantly, documented by objective medical testing which can be used for an early and large settlement.
What are the steps to follow in order to achieve this it improved recovery? The first step is to document that your client has a valid complaint of pain. This is accomplished using a test developed by a team of doctors from Johns Hopkins Hospital, called the Pain Validity Test found at www.MarylandClinicalDiagnostics.com. There have been nine articles published about this test, involving 794 patients, authored by faculty members at Johns Hopkins University School of Medicine, and other institutions [2-10].
The Pain Validity Test has been admitted as evidence in over 30 cases in 8 different states. The Pain Validity Test can predict which patients will have abnormalities on objective medical testing with 95% accuracy, and predicts who will not have abnormalities with 85% to 100% accuracy. Therefore, this test can be used to refute the defense claim that the patient is faking or malingering, even in the presence of normal MRIs, CAT scans, and x-rays. Also, the Pain Validity Test can predict intra-operative findings with 93% accuracy [9], and identify drug seeking behavior with 95% accuracy [10].
Research from a team of doctors at Johns Hopkins Hospital indicates that only 6% to 13% of claimants are exaggerating their complaints of pain [3-5]. More importantly, 87% to 94% of all claimants have a valid complaint of pain, which will be documented by objective medical testing [3-7]. Actually, more correctly, the valid complaint of pain will be documented by the correct objective medical testing. The X-ray, MRI, and CAT scan are not the correct medical test for posttraumatic lesions.
What are the correct medical test? A trial lawyer should understand that pain is a subjective physiological experience, which cannot be measured. You cannot take a picture of pain. The best way to explain this to jury is to ask “If I had an oven up on the wall, and I took a picture of it, and I handed it to you, could you tell me if the oven is hot?" Then ask "If I put a thermometer in the up and I handed to you, and it read 375 °F, could you tell me if the oven is hot?" These questions clearly and quickly demonstrate to a jury the difference between anatomical test, such as X-rays, MRI, CT compared to physiological tests, such as facet blocks, root blocks, and provocative discograms, as well as flexion extension X-rays, or rotational 3D-CT, or a cine-MRI of the temporomandibular joint, or a SPECT scan or PET scan of the brain, or vascular flow studies with the arms up in arms down. Typically, a trial attorney may not have a client who has received the latter group of test, or in some cases, the trial attorney was never even heard of some of the tests in the latter group.
What is the real distinction between anatomical testing and physiological testing? The MRI (an anatomical test) misses detection of damaged discs 78% of the time compared to provocative discograms (a physiological test) [11]. Upright X-rays never reveal the pathology of a torn ligament in a patient who complaints of worse neck pain with either flexion or extension. Only flexion-extension X-rays can detect motion, which produces the pain. Likewise, the CT misses boney lesions 56% of the time compared to a 3D-CT [12,13], and EMG-Nerve conductions studies miss the vascular compression which is part of the pathology of thoracic outlet syndrome [14]. That's why clients are so misdiagnosed.
Once the Pain Validity Test is been obtained, the trial attorney now knows whether or not it is worthwhile to pursue medical testing for his client. The next question becomes determining which medical test is appropriate. Before proper testing can be obtained, the client needs an accurate diagnosis. Research from a number of medical institutions indicates that 40% to 80% of chronic pain patients are misdiagnosed, and may reach 91% to 97% for electrical injuries and “fibromyalgia” [1,15-21]. The same group of physicians from Johns Hopkins Hospital who developed the Pain Validity Test also developed The Diagnostic Paradigm and Treatment Algorithm, from www.MarylandCliicalDiagnostics.com. After a client completes this test, within 5 min. results are available, which lists diagnoses that have a 96% correlation with diagnoses Johns Hopkins Hospital doctors [22]. Based on these accurate diagnoses, the correct medical test is listed. The results of the correct medical test are what a trial attorney has available to him to take to settlement. These test are readily available the medical community, and provide irrefutable evidence of pathology. Armed with this information, the attorney can now begin to assemble the material needed to pursue settlement.
This is a physiological phenomena, so it requires physiological testing.
The brain is like a bowl of Jell-O contained within a very hard skull. One of the most common areas of damage is when the brain slides forward and strikes the petrosal ridge. Typically, this damages the temporal lobe. This can produce difficulty with speech, memory, personality, and can produce partial complex seizures. The other areas of the brain which are damaged or the frontal lobe, the occipital lobe, it was termed a coup-countercoup phenomena. Damage to the frontal lobe will affect smell, taste, and personality, while damage to the occipital lobe may produce difficulty with vision.
The patient often will complaint of memory loss, loss of smell or taste, trouble remembering words, or even periods of loss of consciousness.
A skilled clinician will perform the following physical testing on a patient: test for sense of smell, test for sense of taste, tuning fork hearing test, both Weber and Rhine, test eyes for nystagmus, check the pupils reactivity to light, and equal size, subtract 7’s from 100, give 5 cities, and ask the patient to repeat them in 5 minutes (always give the same 5 cities so you remember them), ask similarities, I.e. how are an apple and an orange alike? (both fruits), How are canoe and a basketball alike? (both float), How are a fly and a tree alike? (both living).
When post-concussion syndrome suspected, there is limited value in obtaining an MRI or CT of the brain. This would determine sub-dural hematomas, or other space occupying lesions, but not the subtle intellectual changes that are associated with post concussion syndrome, such as memory loss, altered speech patterns, change in emotion, and sometimes partial complex seizures. The objective medical test which can be used to determine elements of post-concussion syndrome are EEG, SPECT scan of the brain, and a PET scan of the brain, as well as a WAIS IQ test, Bender-Gestalt testing, Raven progressive matrices, and Luria Nebraska testing.
There are some exercises which can help to improve functionally, where one area of the brain takes over function for the damaged area. This is a time consuming process, and often no major improvement is seen.
In addition to the incorrect medical tests, physicians fail to address the clinical features of the patients with chronic pain. One of the most overused group of diagnoses is sprains and strains. Sprains are defined as overstretching of the ligaments, the fibrous tissue which holds the bones together. Trains are defined as an overextension of muscle tissue, which is attached to the bone by the ligaments [23].
Sprains and strains should last no longer than a month. After that period of time the problem is something other than a sprain or a strain. In fact, the Department of Health and Human Services of the US government has defined a strain as a disorder which causes an average of 7.5 days of restricted activity, two days of bed disability, and 2.5 days of work loss [24]. So any “sprain or strain” which persists beyond the month is incorrectly diagnosed 100% of the time, and requires a more directed medical evaluation.
In the flexion extension injuries typically seen with whiplash, the ligaments which hold the vertebral bodies together are often torn. This allows excessive motion of one vertebral body on the other, accentuated by either flexion or extension. However, the facet joints of the neck are oriented horizontally, so a torn ligament may also result in pain when turning the head side to side. Additionally, the inter-vertebral disc may also be damaged, but not be visible on CAT scan or MRI.
The patient will complaint of worse pain leaning his head forward, or leaning his head backwards, worse pain in the neck and possibly the arm with coughing or sneezing or bowel movements.
One obvious examination is to have the patient leave his head forward and lean his head backwards and tell the physician what he experiences at the time. The Spurling test consists of hitting the patient on top of the head, to see that reproduces the pain worsens the pain that they may feel in the neck and/or the arms. This movement compresses the disk in the neck. Muscle tenderness is often present in the scalene muscles, splenious muscle, semi-spinalis capitus muscle, trapezius, and other muscles of the head and neck, but really contribute little to the diagnosis.
The patient should have flexion extension X-rays with obliques, and open mouth odontoid views. If there is pain with turning the neck, then a 3D-CT with rotation will show rotational subluxation. Then the patient should have facet blocks. A temporary facet block given at the level of suspected pain, and the level above and below the suspected level, since a facet joint has sensory innervation not only from the level of the pain, but receives contributions from the level above and below the area of physical damage. A facet denervation is the treatment of choice.
If there is pain down the arms, root blocks, of specific levels C3 through C7 should be performed. EMG/Nerve conduction studies are often normal since they do not measure sensory nerve damage very well. So a sensory nerve test, call the current perception threshold (Neurometer) will document sensory nerve damage [24]. If there's associated headache, pain over the ear, radiating to the eyebrow, the patient should also have a C2-C3 root block.
Finally, if the patient complains of worse neck and arm pain with coughing and sneezing, or flexion or extension, the patient should have provocative discometry, C2 through C3 [1].
If facet syndrome is confirmed, then a facet denervation will provide relief. However, only 40% of patients get up to 2 years relief. The definitive treatment is a fusion. The same holds true for root damage, although a foraminotomy may help, instead of a fusion. If there is a damaged disc, the treatment is discectomy [1]. In fact, research from Johns Hopkins Hospital documented that 63% of patients with normal MRI, CT and X-ray, who were diagnosed with “whiplash” really had damaged discs and needed surgery to improve [1].
Another commonly overlooked diagnosis after a rear-end collision is thoracic outlet syndrome. In 90% of these cases, compression of the brachial plexus between the anterior and medial scalene muscle is the source of the symptoms Figure 1. Only 10% have vascular compression [25,26].
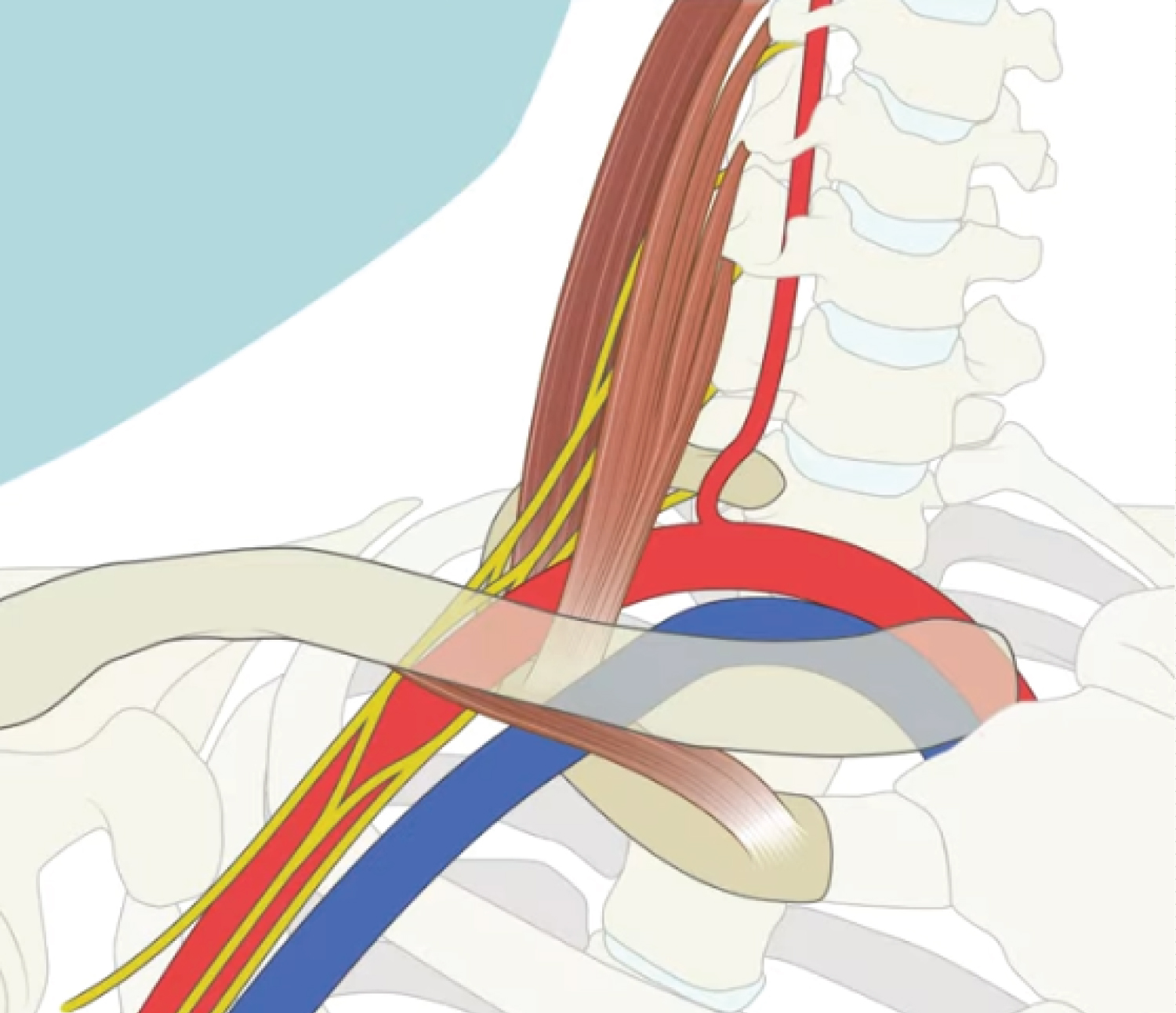 Figure 1: The anatomy of Thoracic Outlet.
View Figure 1
Figure 1: The anatomy of Thoracic Outlet.
View Figure 1
The nerve, artery and vein supplying the arm passes between the anterior and medial scalene muscles, but 34% of the time, nerve going down the arm also pass between the posterior and medical scalene muscle [18].
Typically, the patient complaints of pain and/or numbness in the arm going to the last two fingers, or perhaps all fingers. The symptoms worsen with hold the arms elevated for 3 minutes or more, often seen when trying to hang a picture or brushing hair, or painting a ceiling, Extension of the head or rotating the head will also worsen symptoms.
Since the pathology of thoracic outlet syndrome is mostly neurological, or combination of neurological and vascular pathology, the best clinical tests is the Roos maneuver [25,26]. A Roos maneuver consist of asking the patient to elevate their arms, with their elbows as high as their shoulders, and bent 90° at the elbow. The patient is then asked to hold that position for 2 min., and then asked what they feel in their fingertips. If the fingertips are numb, then this is a positive Roos test. The Adson maneuver consists of feeling the radial pulse and asking the patient to turn their head in the opposite direction. A diminution of the pulse is indicative of a positive Adson maneuver. Obviously, this maneuver detects vascular compression, which occurs less than 10% of the time in thoracic outlet syndrome, and even then it is unreliable 80% of the time (Figure 2).
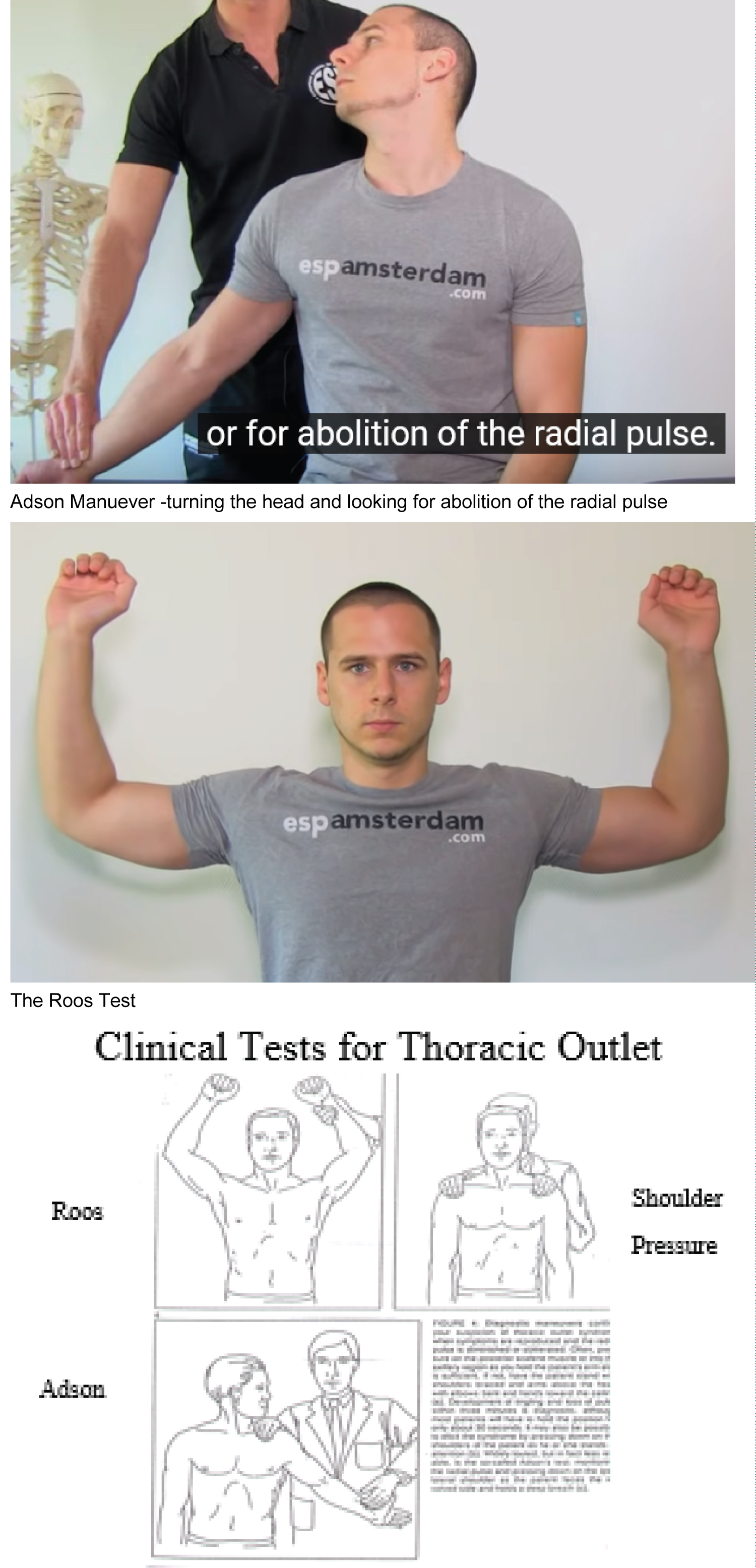 Figure 2: Clinical tests for thoracic outlet.
View Figure 2
Figure 2: Clinical tests for thoracic outlet.
View Figure 2
However, when vascular compression does accompany thoracic outlet syndrome, the Roos maneuver is a better test than the Adson maneuver, as demonstrated by vascular flow studies with the arms up and arms down, in the bruise position, compared to the Adson maneuver. Over 80% of the time, vascular compression will be demonstrated by the Roos maneuver, but missed by the Adson maneuver. Again, as is true with all sensory nerve damage, the neurometer studies are useful for detecting sensory nerve damage, and are especially valuable, if the studies are conducted when the patient has their arms in the Roos position, compared to being at rest [27] (Figure 3).
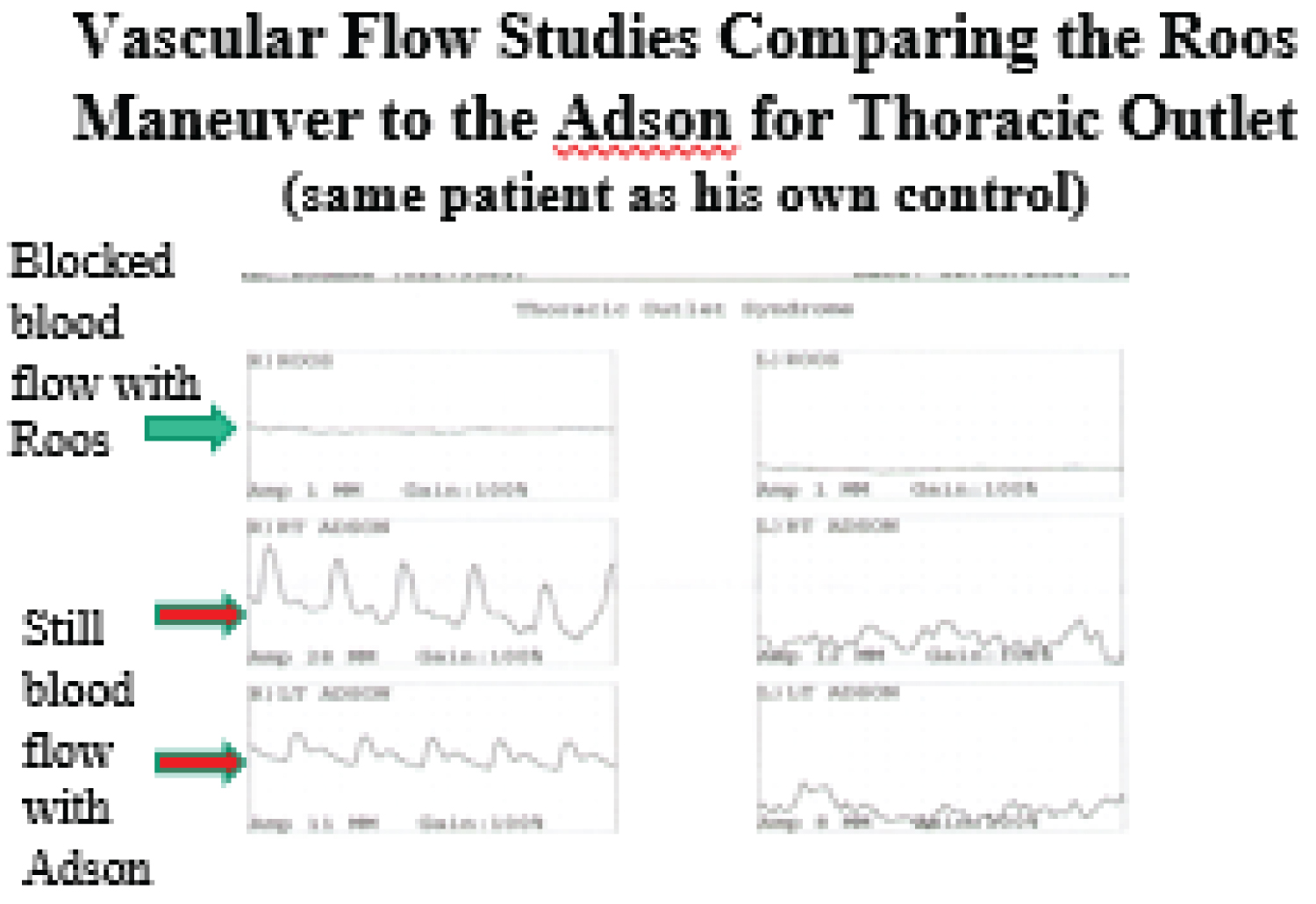 Figure 3: Vascular flow studies.
View Figure 3
Figure 3: Vascular flow studies.
View Figure 3
The EMG-nerve conduction studies are of little use in trying to establish the diagnosis of thoracic outlet syndrome. because the distance across Erb’s point is less than 5 inches, which does not produce reliable EMG nerve conduction velocity study results. Neurometer studies with the arms up and down will help document sensory nerve compression.
Resection of the first rib to decompress the thoracic outlet is the definitive treatment of choice. Some surgeons decompress the brachial plexus from above, and resect the anterior and medial scalene muscle, and first rib [28] (Figure 4).
 Figure 4: (Image from radiopaedia.org- used with permission). Normally, the disc resides as a cushion between the fossa in the skull and the head of the mandible, called the condyle. The image shows an anteriorly dislocated disc without recapture on mouth opening. The best way to determine if the disc displaces with movement is to use a Cine MRI. This is a MRI movie of the TMJ as the patient opens and shuts his or her jaw. The patient is performing the very activity (opening and shutting the jaw) which produces symptoms, so the physician has the opportunity to see what actually happens when the patient opens and shuts his or her jaw.
View Figure 4
Figure 4: (Image from radiopaedia.org- used with permission). Normally, the disc resides as a cushion between the fossa in the skull and the head of the mandible, called the condyle. The image shows an anteriorly dislocated disc without recapture on mouth opening. The best way to determine if the disc displaces with movement is to use a Cine MRI. This is a MRI movie of the TMJ as the patient opens and shuts his or her jaw. The patient is performing the very activity (opening and shutting the jaw) which produces symptoms, so the physician has the opportunity to see what actually happens when the patient opens and shuts his or her jaw.
View Figure 4
Tempro-mandibular joint syndrome (TMJ) may manifest as pain in the temple, the TMJ, and a click with opening the jaw. It may be associated with associated bruxism, which is grinding of the teeth. This can be caused by damage to the ligaments and/or disc of the joint between the skull and the head of the jaw. The temporomandibular (TMJ) joint is a very unusual joint. It slides forward, slides side to side and hinges. It is formed by the head of the condoyle of the jaw (mandible) inserting into a recess in the skull right beneath the temporal bone.
The jaw is held against the skull by ligaments. The temporomandibular (TMJ) joint is a very unusual joint. It slides forward, slides side to side and hinges. It is formed by the head of the condoyle of the jaw (mandible) inserting into a recess in the skull right beneath the temporal bone. Excessive motion can be caused by damage to the ligaments and/or disc of the joint between the skull and the head of the jaw. In an accident, when the head is thrown forward, the jaw moves with the head, but has enough momentum to continue to go forward, even when the head stops going forward, which tears the ligaments holding the jaw to the skull. These are the strong lateral temporomandibular ligaments and two weaker medial ligaments [9]. The nerves that supply the joint are the auriculotemporal and branches of the third division of the trigeminal nerve [9]. Irritation of these nerves produces pain in the jaw, cheek, and/or temple.
Tempro-mandibular joint syndrome (TMJ) may manifest as pain in the temple, the TMJ, and a click with opening the jaw. It may be associated with associated bruxism, which is grinding of the teeth. The patient may also have ringing in their ears, and tenderness in the sternocleidomastoid muscle, and a sensation of a stuffy ear with reduced hearing. Other symptoms may be facial pain, in the cheek, pain in the area of the joint, pain in the jaw line, dizziness, pain in the temple and clicks in the jaw on opening or closing the jaw [29].
The patient may feel tenderness over the masseter muscle, the temporalis muscle, and the sternocleidomastoid muscle. There may be a click in the TMJ with opening of the jaw.
If there is severe ligamentous damage, the disc will be displaced, which is best seem on cine-MRI, which is a movie taken using an MRI machine, while the patient opens and shuts his jaw. Trigger point injections into the sternocleidomastoid muscle may give temporary relief and serve as a confirmatory test.
A bite plate may help the grinding of the teeth. Under no circumstances should the teeth be ground down to “line up the bite.” Only in rare and extreme cases would surgical repair of the ligaments be indicated.
This Is an often overlooked sequela of an auto accident. Seat belt injuries occur on the side where the seat belt inserts into the restraint. Typically, this will be on the right side for a driver and left side for a front seat passenger.
The 2 nd through 9 th rib join the sternum. However, the 10 th , 11 th rib and 12 th rib have a cartilage joining these bones to the rib above it. This cartilage can tear as the result of trauma.
The patient will feel pain in the lower outside rib cage with bending over or twisting, or pressure on the 10 th and 11 th rib. Pain will be in the side of the chest at the level of the 10 th rib in line with the nipple.
The “hook sign” is the best way to determine slipping rib syndrome [30]. A physician puts his fingers under the rib cage of a patient, at the 10 th rib, and lifts up. If this reproduces the pain, this is a positive hook sign, and the patient has slipping rib sign. Also, if pressure at the site of the pain intensifies the pain, this is compatible with slipped rib syndrome.
Although widely discounted due to overuse, thermography often will show a “hot spot” at the site of dislocation and inflammation.
Steroid injections at the site may help, but the ultimate treatment is excision of the rib tip of the 10 th rib, 11 th rib and 12 th rib.
Tietze’s Syndrome (Costochondritis) occurs when there is inflammation at the junction of the rib bones 2 through 9, and breastbone (sternum). There is cartilage joining these bones. This cartilage can tear as the result of trauma.
Costochondritis can be found after a traumatic injury. Typically, this is after a car accident, where the driver's chest strikes the steering wheel, or from the air bag deployment.
Most patients with costochondritis experience pain over the front of the upper chest (the area of the breastbone). Because of serious conditions, most importantly conditions related to heart problems, costochondritis should only be diagnosed after excluding other more serious problems. Costochondritis pain is usually worsened by activity or exercise. Often the pain is worsened when taking a deep breath. This stretches the inflamed cartilage and can cause significant pain.
Touching the area involved by costochondritis can be extremely painful for the patient.
Although widely discounted due to overuse, thermography often will show a “hot spot” at the site of dislocation and inflammation.
Costochondritis usually responds well to rest. In order to decrease the inflammation, avoid activities which cause pain, such as lifting. Applying heat several times a day to the chest can be helpful in relieving symptoms of costochondritis. Nonsteroidal anti-inflammatory medications (I.e. Motrin, Advil) may help decrease inflammation, which is the primary problem. While symptoms usually improve within a few weeks and resolve completely within a few months, some patients have this problem persists for months. In persistent cases, costochondritis may be treated with cortisone injections.
The best example of what to expect from a thorough evaluation of whiplash and cervical sprain cases was reported in an article by a team of physicians from Johns Hopkins Hospital, led by Donlin Long, MD, PhD, who was the chairman of neurosurgery [1]. The article was titled “Fusion for Occult Posttraumatic Cervical Facet Injury,” and was publish in Neurosurgery Quarterly (Volume 16, Number 3, September 2006, pages 129-134). Dr. Long and his team evaluated seventy patients with normal MRI, CT and X-Rays, who had persisting pain after injury (median 1.7 y), who had failed all usual conservative forms of care. They had been told by their referring physicians that there was nothing more to do to help them. The patients were offered a diagnostic block protocol to determine the origins of the persisting pain. Blocks included C-2-3 roots bilaterally; C-2-3-4 zygapophyseal joints (facet joints) and provocative discography at C-3-4, 4-5, 5-6, 6-7. Of the 70 patients, 68 completed the block protocol, and of these 68 patients, 44 of them (65%) went on to have posterior cervical fusions of C-l, 2, 3, 4 in several combinations. Seventy nine percent of patients achieved complete pain relief, while 14% received satisfactory pain relief.
If the trial attorney has their medical personnel evaluate their “whiplash” or cervical sprain cases after an auto accident for each of the 6 commonly found disorders, there is a strong likelihood that many if not all 6 of the disorders will be found, and 63% will likely need a cervical fusion to improve. This will provide better patient care, and certainly increase recovery, which helps both patient and attorney alike.