Ultrasonography (USG) is a resourceful tool in the perioperative period. A structured training curriculum during residency can enhance the utilisation of USG among residents. This cross-sectional online survey was conducted to evaluate the utilisation of USG in the perioperative period and to assess the adequacy of current training. It was found that although the availability of USG has increased, its use in the perioperative period is limited due to various factors such as time constraints. The use of USG in the preoperative and postoperative periods is limited when compared to the intraoperative period. The majority of the residents (N = 82, 81.2%) felt that they needed more training in the utilisation of USG.
USG: Ultrasonography; GRV: Gastric Residual Volume; DVT: Deep Vein Thrombosis; ECHO: Echocardiography, POCUS: Point of Care Ultrasound, BMI: Body Mass Index
The evolution of ultrasound (USG) has revolutionised the medical field with its rapid and accurate diagnosis for effective management especially during emergencies. It is portable and its availability is increasing even in low-resource settings [1]. The role of USG in the perioperative period is rapidly emerging. It is used for various purposes such as vascular access, administration of regional nerve blocks and echocardiographic evaluation of cardiac function [2]. Since anaesthesiologists frequently encounter unanticipated emergencies, USG can be a useful tool at hand, considering its easy accessibility and portability. More emphasis is being placed on including USG in routine clinical practice to improve diagnostic accuracy by implementing USG as a fifth pillar of clinical examination [3]. The two important steps in the proper utilisation of USG include a clear image acquisition followed by an interpretation of the acquired image. This necessitates a structured training curriculum regarding the principles of ultrasound, a knowledge of its utilisation in the perioperative period and its role in the determination of the treatment plan during residency.
A cross-sectional online survey was conducted via Google Forms among anaesthesiologists at various Tertiary care centres in India. All anaesthesiologists who were willing to fill out the forms were included. No prior sample size calculation was done.
A questionnaire was formatted consisting of 15 questions. The questionnaire was sent to the participants through email or any electronic mode of communication. This was an electronic survey conducted after obtaining informed consent from the participants. The participants were directed to complete the self-reported questionnaire and submit the responses. The survey was conducted over one week. Each participant was allowed to submit one response only. Confidentiality of the records was maintained.
The questionnaire consisted of 15 questions (Table 1) regarding the designation of the participant, the availability of ultrasound and the utilisation of ultrasound in the perioperative period. It was aimed at evaluating the various indications for which ultrasound was used and also to assess the adequacy of training among anaesthesiology residents pertaining to the perioperative utilisation of ultrasound. The questions were in English and distributed as Google forms with all questions requiring a response mandatorily. However, it was not validated or tested in a pilot study.
Table 1: Questionnaire on Perioperative utilisation of ultrasound. View Table 1
Anaesthesiologists at various tertiary care institutes in India who were willing to submit their responses to the questionnaire were included.
Those who declined the consent for participation were excluded.
Statistical analysis was performed with Microsoft Excel (office 365) software.
The google forms were distributed via email or other electronic modes. Out of the 250 forms distributed, 101 responses were recorded with a response rate of 40.4%. The data was collected for one week and the collected data was entered in Microsoft excel for analysis and graphical representation. Most of the participants were junior residents pursuing anaesthesiology residency (N = 58, 57.4%) at a tertiary care centre and Senior residents, who completed three years of residency training in anaesthesiology (N = 35, 34.7%) (Figure 1). USG was available for routine use at almost all institutes (N = 100, 99%). More than half the residents (N = 66, 65.3%) used USG on a daily basis in the perioperative period for various indications. Less than half the residents (N = 43, 42.6%) received training in utilisation of USG regularly whereas a few residents (N = 7, 6.9%) never received any formal training during residency (Figure 2). The utilisation of USG was predominantly for performing intraoperative procedures (N = 85, 84.2%) such as venous and arterial cannula or administration of regional nerve blocks, with limited use in the preoperative evaluation (N = 10, 9.9%) and postoperative diagnosis and treatment (N = 6, 5.9%) (Figure 3). Preoperative evaluation of fluid status for prediction of intraoperative hypotension and to determine the intraoperative fluid requirements was done in specific cases only (N = 81, 80.2%) and routinely in all cases by a few (N = 3, 3%). The use of USG for preoperative estimation of gastric residual volume (GRV) in emergency cases for prediction of risk of aspiration (N = 13, 12.9%) as well as for the assessment of anticipated difficult airway (N = 20, 19.8%) was very minimal. Less than half the residents performed Deep vein thrombosis (DVT) screening preoperatively (N = 46, 45.5%) in all high-risk cases such as cases of long bone fractures with prolonged immobilisation. Screening echocardiography (ECHO) for preoperative assessment of cardiac function such as evaluation of valvular function and to identify any regional wall motion abnormalities was done by many (N = 73, 72.3%). When encountered with multiple failed attempts at spinal or epidural anaesthesia, the majority of the anaesthesiologists (N = 86, 85.1%) opted to conduct the case under general anaesthesia rather than attempting central neuraxial blockade under USG guidance (N = 15, 14.9%). The majority of the residents (N = 86, 85.1%) felt that USG is being underutilised in the perioperative period and everyone felt that USG should be included as a part of the anaesthesiology curriculum during residency. Time was considered as a limiting factor for the underutilisation of USG by many (N = 53, 52.5%). Even though USG has been utilised more in recent times, the majority of the residents (N = 82, 81.2%) felt that they needed more training (Figure 4).
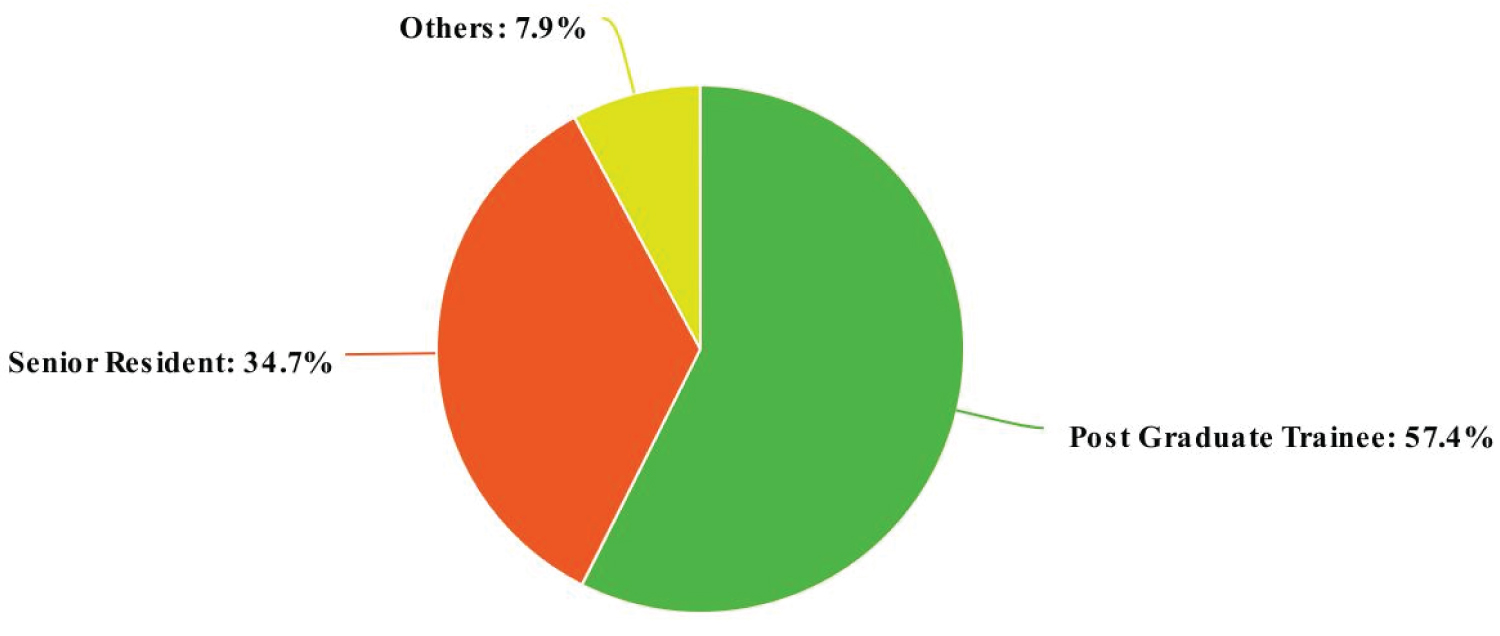 Figure 1: Pie Chart showing the current designation of participants.
View Figure 1
Figure 1: Pie Chart showing the current designation of participants.
View Figure 1
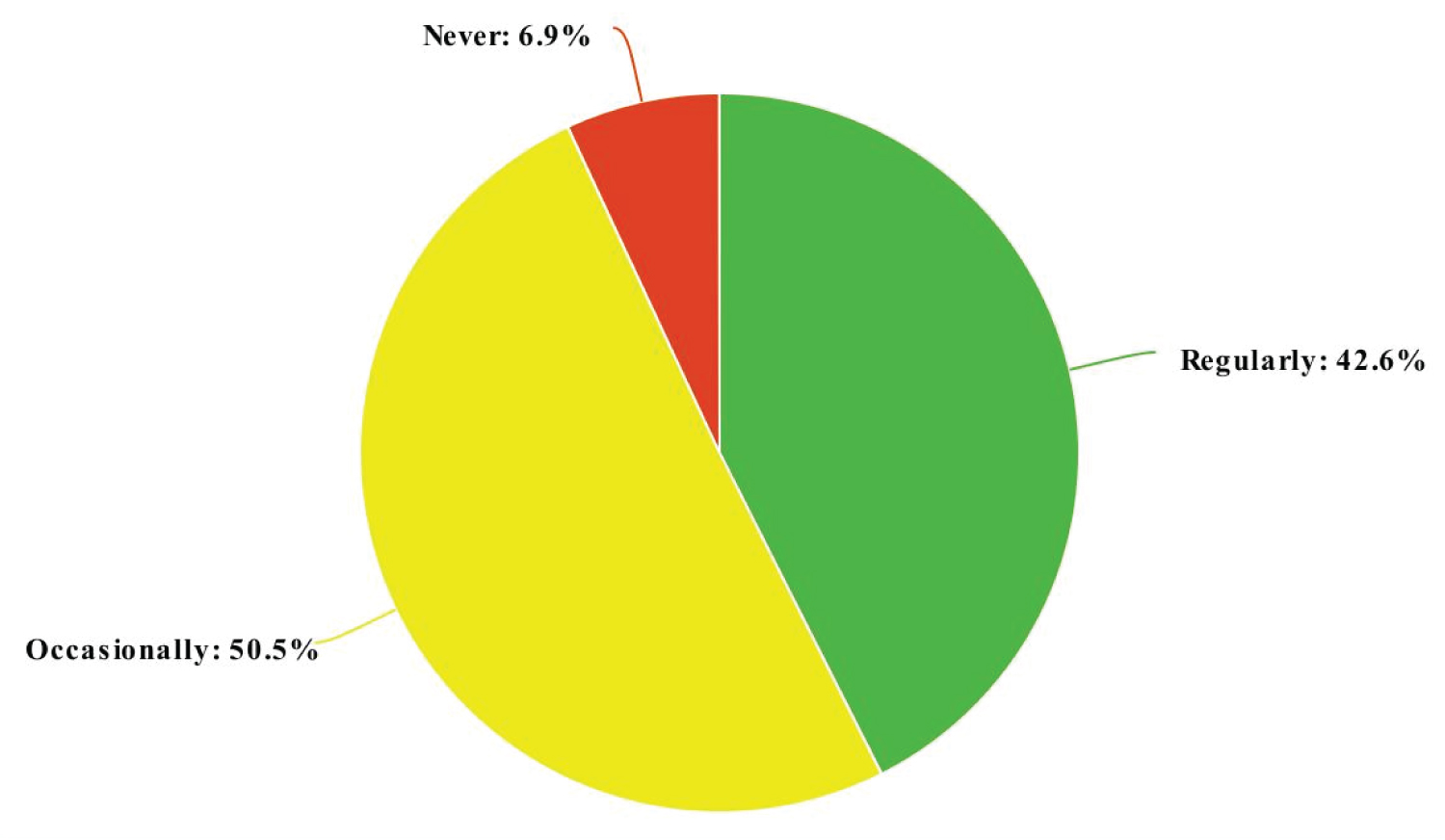 Figure 2: Pie chart showing the frequency of formal training received about utilisation of Ultrasound.
View Figure 2
Figure 2: Pie chart showing the frequency of formal training received about utilisation of Ultrasound.
View Figure 2
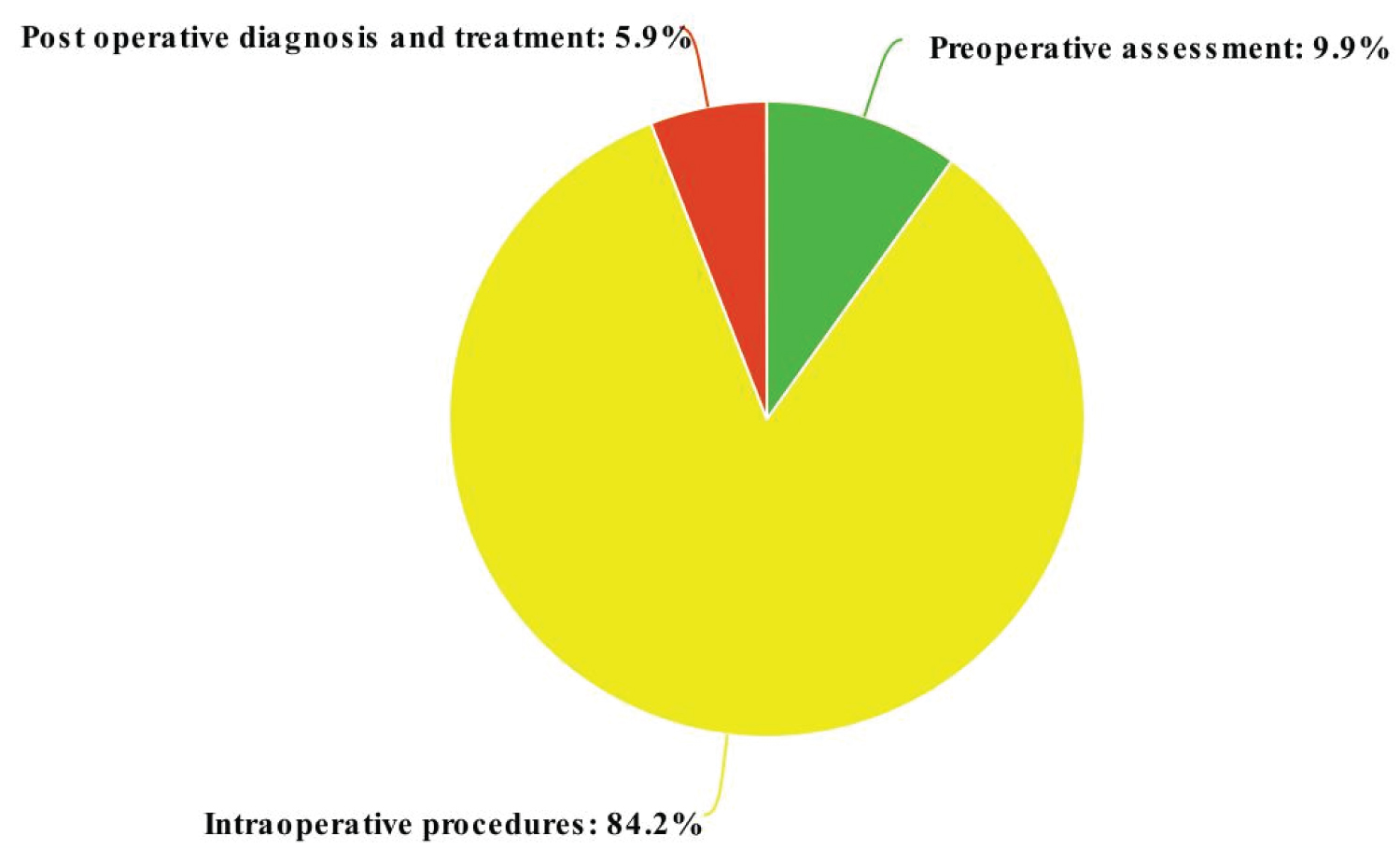 Figure 3: Pie chart showing the usage of USG in the perioperative period.
View Figure 3
Figure 3: Pie chart showing the usage of USG in the perioperative period.
View Figure 3
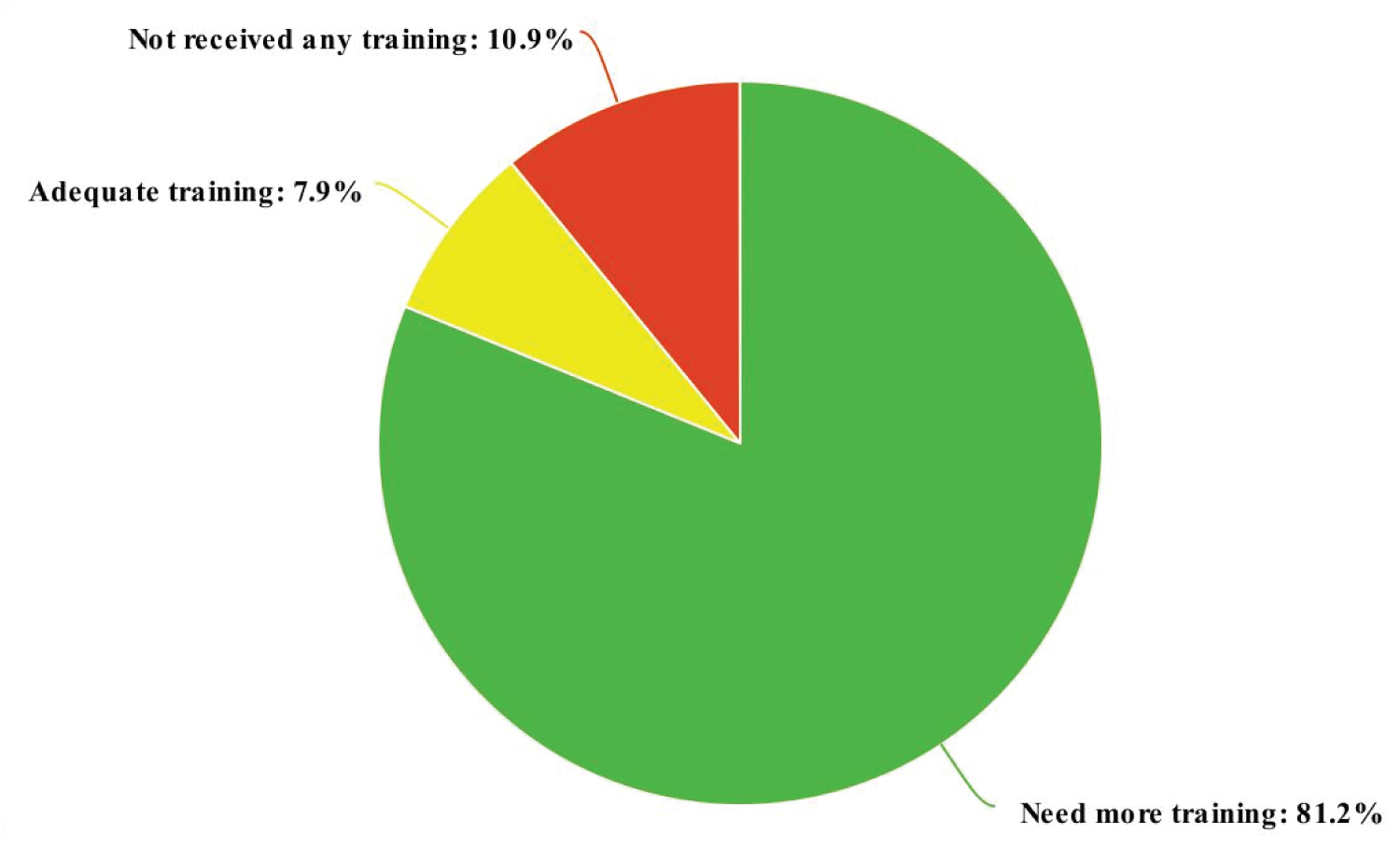 Figure 4: Pie chart depicting the adequacy of training in USG.
View Figure 4
Figure 4: Pie chart depicting the adequacy of training in USG.
View Figure 4
This questionnaire-based survey was conducted to assess the utilisation of USG in the perioperative period. Although the availability of USG has increased in recent times, integration of USG as a part of the anaesthesiology curriculum during residency is still restricted due to various limiting factors such as time constrain. Though USG can be used for various indications in the perioperative period, it is mainly used for performing intraoperative procedures such as central venous cannulation, arterial cannulation and USG-guided nerve blocks. The usage of USG is limited in preoperative evaluation and postoperative diagnosis when compared to its usage in the intraoperative period.
Ramsingh D, et al. assessed the impact of perioperative ultrasound training in anaesthesiology residents and concluded that a whole-body Point of care ultrasound (POCUS) curriculum can be effectively taught to anaesthesiology residents and that this training may provide clinical benefit. Clinical examinations performed in the organization after the study (n = 224) showed that point of care ultrasound affected clinical management at a rate of 76% and detected new pathology at a rate of 31% [4]. Ultrasound is gaining clinical importance in various areas of preoperative assessment. One such area is its role in preoperative assessment of anticipated difficult airway. It aids in the identification of airway sonoanatomy and also assists in performing procedures such as percutaneous tracheostomy [5].
Estimation of preoperative GRV can play a role in estimation of aspiration risk. Chaitra T, et al. measured the gastric antrum in both supine and right lateral decubitus positions using USG in the immediate preoperative period, and gastric residual volume was calculated. It was found that As Body Mass Index (BMI) increased, there was a statistically significant ( p -value < 0.001) increase in mean antral cross-sectional area in both supine and right lateral decubitus positions. There was a statistically significant association found between type 2 diabetes ( p -value 0.045 * ) with antral grade. Ultrasound plays an important role in evaluation of lung pathology preoperatively. With adequate training, ultrasound can be a very powerful diagnostic tool in the identification of conditions such as pneumothorax, pulmonary edema and pleural effusion. It also plays a major role in the intraoperative period. It can be used for the confirmation of endotracheal tube placement, for securing vascular access, for assessing cardiac function and as a primary diagnostic modality for identifying regional wall motion abnormalities [6].
Although there is extensive literature available regarding the various indications for which ultrasound can be used, there are many limitations in the perioperative period which can adversely affect the use of ultrasound. Lack of adequate training remains the most important barrier to ultrasound utilisation [7]. Inculcating a structured curriculum during the anaesthesiology residency can overcome this limitation.
The validity of the questionnaire was not tested prior. The inclusion of more anaesthesiology residents can give a better idea of the availability and utilisation in more centres. Analytical approaches were not utilised. The results of this study cannot be generalised to all health care centres across India as it included tertiary care centres only.
Ultrasound has emerged as a valuable tool for anaesthesiologists for various purposes in the perioperative period. A thorough understanding of sonoanatomy and adequate training, hold significant potential to enhance patient care. Despite the increasing availability of ultrasound in numerous medical centres over recent years, its integration into perioperative procedures remains limited for diverse reasons. To address this limitation, incorporating fundamental ultrasound skills into the curriculum for anaesthesiology residents can facilitate more effective utilization of this resource. This initiative is pivotal in advancing patient-tailored care and minimizing complications during the perioperative period.
None.
None.