This case study presents the management of a 54-year-old British male patient suffering from retrosternal goiter with a BMI of 46.11, who was scheduled for lipoma excision and biopsy with adjacent tissue transfer or rearrangement on the back. The patient had a complex medical history, including type 2 diabetes mellitus, hypertension, hyperlipidemia, and obstructive sleep apnea. Preoperative assessments revealed difficulties in mask ventilation, intubation, and ventilation due to anatomical factors, such as a thyromental distance of less than 6 cm and a large retrosternal goiter causing compressive symptoms and wheezy breathing. A multidisciplinary team implemented a dual-plan approach utilizing a laryngeal mask airway (LMA) as the primary airway management strategy, with an endotracheal tube as the backup plan. The patient underwent successful surgery with stable vital signs and optimal oxygenation. This case emphasizes the significance of comprehensive preoperative assessments, multidisciplinary collaboration, and adaptable airway management strategies in challenging surgical cases.
Retrosternal goiters, also known as retrosternal thyroid goiters or retrosternal thyroid masses, are thyroid enlargements that either extend below the thoracic inlet or have more than 50% of their mass located within the mediastinum. RSG are usually benign in nature can occur in 1-20% of goitres. Retrosternal goiter is not a common cause of different degrees of tracheal compression and tracheomalacia [1,2]. It commonly result in the compression of structures within the mediastinum, which can lead to significant complications, including cerebral hypoperfusion and axillosubclavian vein thrombosis [3]. All of these may lead to difficult intubation or postoperative tracheal collapse. Anesthetic management of patients with mediastinal masses and comorbidities remains challenging as acute cardiorespiratory decompensation may follow induction of anesthesia.
Scattered case studies describing patients who experienced acute cardiorespiratory decompensation during anesthesia have been reported which was attributed to tumor-related compression of mediastinal organs that have life-threatening or outcomes fatal [4,5]. We describe the anesthetic management of comorbid patient with massive retrosternal goiter accompanied severe intrathoracic tracheal narrowing scheduled for Lipoma excision and biopsy.
A 54-year-old British male patient with a BMI of 46.11 was posted for lipoma excision and biopsy with adjacent tissue transfer or rearrangement on the back. The patient had a medical history of type 2 diabetes mellitus, hypertension, hyperlipidemia, and obstructive sleep apnea, and was dependent on BIPAP for ventilation. On preoperative assessment, the patient had difficulty in mask ventilation, intubation, and ventilation, with a thyromental distance of less than 6 cm and neck circumference of 24 inches. The patient also had a large retrosternal goiter causing compressive symptoms and wheezy breathing. The patient's hematological and biochemical findings were all within normal limits. The complete blood count (CBC) showed a hemoglobin of 13.7 g/dL, hematocrit of 42.7%, white blood cell count of 8760/µL, and platelet count of 289,000/µL. The serum chemistries showed a normal glucose, electrolytes, liver function tests, and renal function tests. Patient's chest X-ray revealed prominence of bronchovascular markings within the bilateral lung fields, which is indicative of changes related to bronchitis (Figure 1).
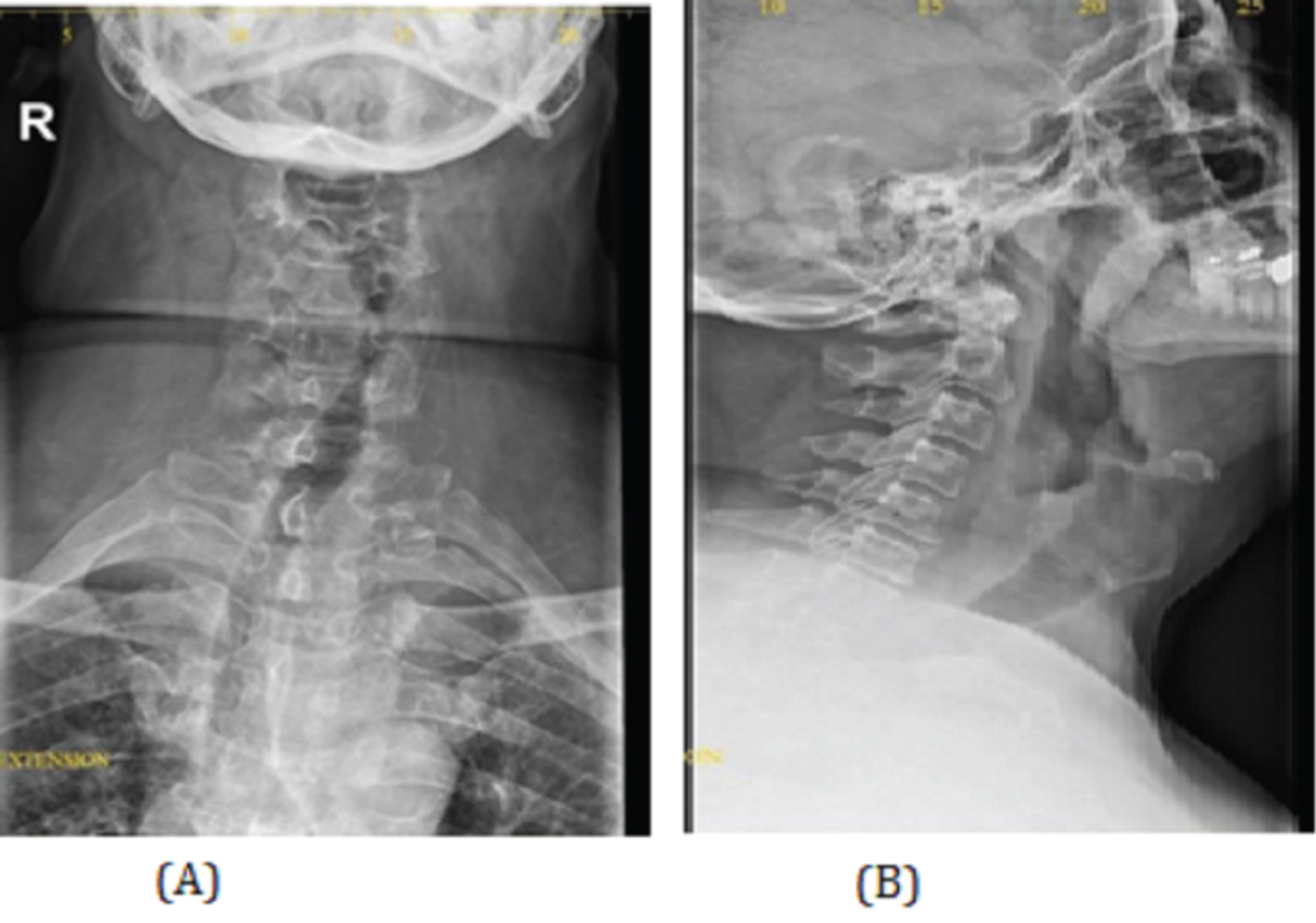 Figure 1: (a) X-Ray examination plate for Neck Anterior-Posterior Position; (b) X-Ray examination plate for Neck Lateral Position.
View Figure 1
Figure 1: (a) X-Ray examination plate for Neck Anterior-Posterior Position; (b) X-Ray examination plate for Neck Lateral Position.
View Figure 1
During the ultrasound examination of the neck, a subcutaneous lipoma was identified, which was an unexpected finding. Further concerns were raised when the presence of internal foci of calcification within the lipoma was observed, which is considered atypical for lipomas (Figure 2).
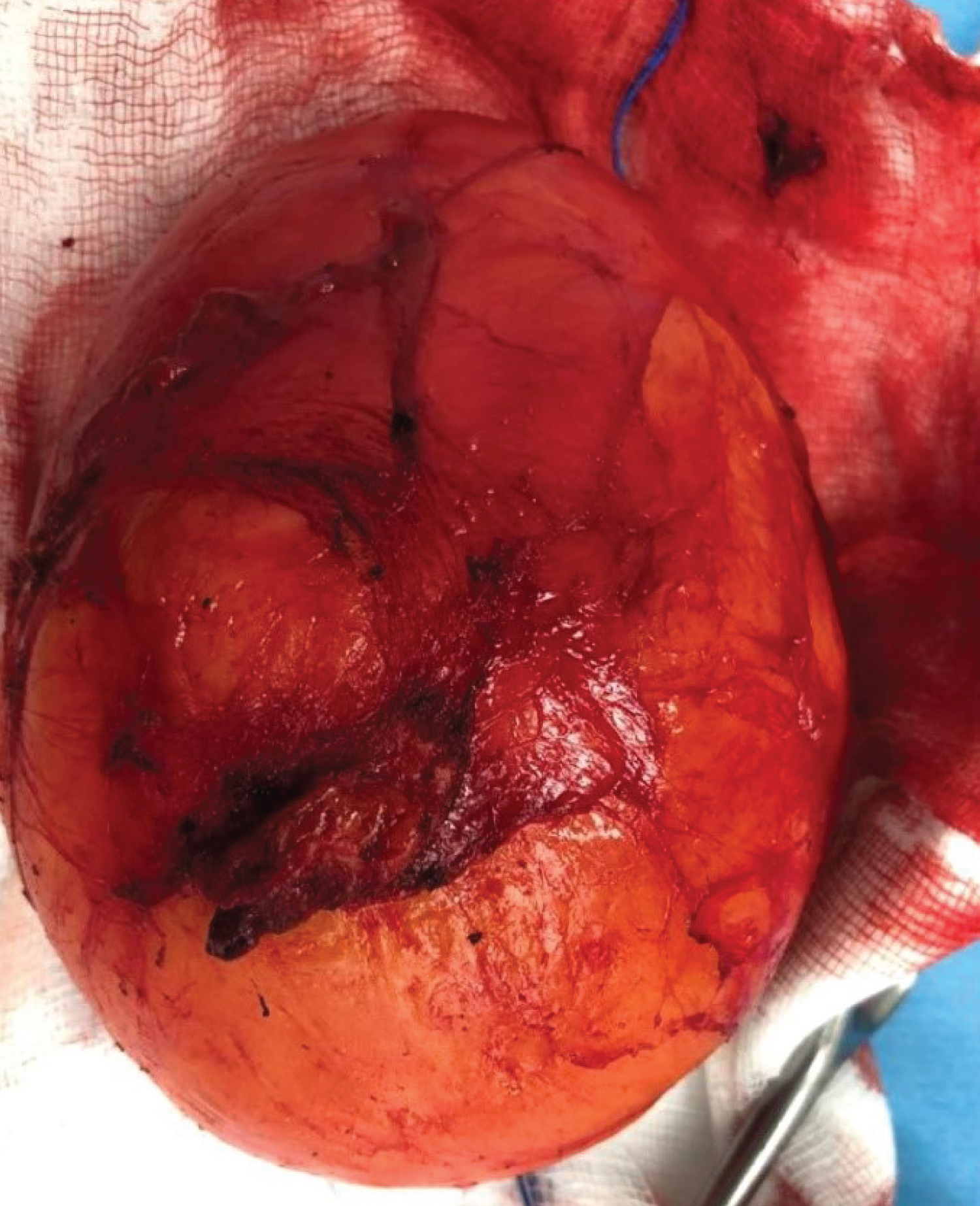 Figure 2: Identification of Neck Lipoma.
View Figure 2
Figure 2: Identification of Neck Lipoma.
View Figure 2
The MRI of the neck revealed significant findings, including a large multinodular goiter with retrosternal extension and rightward tracheal deviation. The goiter was exerting pressure on the trachea and esophagus, resulting in their compression. Additionally, the MRI demonstrated degenerative changes at the C6-C7 and C5-C6 levels of the cervical spine, indicative of spondylo degenerative changes. Furthermore, cervical myospasm was observed. These findings suggest that the goiter's size and position were contributing to the compression of nearby structures, leading to the development of degenerative changes and muscular spasms in the cervical spine. During the patient's preoperative assessment, it was noted that the patient had audible breathing, indicating potential airway obstruction. The patient's Mallampati classification was determined to be Class 1, indicating good visualization of the patient's oropharyngeal structures. Based on these findings, the anesthesia plan was formulated with a primary plan of using a laryngeal mask airway (LMA) for general anesthesia. However, to account for any difficulties or potential complications, an endotracheal tube was designated as the secondary plan in case the use of an LMA was unsuccessful or ineffective. This dual-plan approach ensures appropriate airway management options are available to secure the patient's airway during the surgical procedure. Anticipating challenges for various airway management scenarios, several items were gathered for the patient's airway intervention including a gastro-LMA size 4, which is a specific type of laryngeal mask airway designed for better access to the esophagus during surgery. Additionally, cough-inflated LMAs in sizes 4 and 5 are prepared. Lateral position was selected for patient's induction followed by administered fentanyl 100 micrograms, lidocaine 40 mg, and propofol 200 mg intravenously to facilitate the induction of anesthesia. The plan for airway management involved using a classic laryngeal mask airway (LMA), as tracheal intubation was not found to be necessary due to the patient being fasted and not having reflux. To maintain anesthesia, propofol was given at a rate of 6 mg per kilogram of the patient's body weight per hour, mixed with oxygen at a concentration of 30% and air. Adequate ventilation was confirmed, and the administration of Inj esmeron 100 mg facilitated muscle relaxation. Throughout the procedure, the patient's vital signs remained stable and well-maintained. The pulse rate ranged between 80 to 86 beats per minute, systolic blood pressure between 100 to 90 mmHg, and diastolic blood pressure between 52 to 62 mmHg. Additionally, the oxygen saturation (SpO 2 ) consistently remained at 100 percent, indicating optimal oxygenation. The patient exhibited good tolerance to the procedure, reflecting a favorable response to the anesthesia and surgical intervention. After the completion of the surgical procedure, the patient was placed in a semi-sitting position for extubation. To facilitate a smooth extubation process, INJ suggamadex 400 mg was administered to reverse the effects of muscle relaxation induced by the anesthesia and prompt recovery of neuromuscular function. This ensured the patient's ability to maintain spontaneous breathing and regain control of their airway independently following extubation.
Mediastinal masses encompass a range of diseases that pose specific challenges for anesthesiologists during general anesthesia. These challenges typically arise from external compression on the airway, obstruction of venous return, or impeding the heart's output. Approximately 7% to 18% of patients with mediastinal masses experience severe complications, specifically related to airway obstruction, which can lead to sudden and refractory cardio-respiratory collapse upon the induction of general anesthesia [6]. In cases of unavoidable general anesthesia maintenance of spontaneous ventilation and avoidance of neuromuscular blockade are superior to positive pressure ventilation and paralysis. CT scans and MRI (magnetic resonance imaging) play crucial roles in providing detailed anatomical information about mediastinal masses and their relationships with surrounding structures [7]. These imaging modalities aid in the development of a well-thought-out plan for both anesthetic and surgical management in patients with mediastinal masses and determining the optimal airway management strategy. General anesthesia can impact the mechanics of the lungs by reducing lung volume and functional residual capacity. It also relaxes the smooth muscles in the airway, increasing the compressibility of larger airways. This relaxation, combined with extrinsic compression, muscular relaxation, and disturbances in active airway inspiratory force, can lead to partial obstruction and the generation of negative pressures that flatten the trachea [8]. As a result, the volume of the chest wall decreases, reducing external support for narrowed airways. Other factors such as the supine position, the absence of glottic regulation of airflow due to endotracheal intubation, and the size and location of the mediastinal mass, as well as preexisting obstructive or restrictive airway conditions, may contribute to the collapse of the airway. An endotracheal tube (ETT) is commonly used as the preferred method for airway management during general anesthesia. However, in patients with mediastinal masses, the insertion of an ETT can present challenges. The presence of the mass may obstruct the view of the vocal cords, making intubation more difficult, and the patient may be more prone to coughing or gagging during the procedure [9].
Laryngeal mask airways (LMAs) are often utilized for airway management as supraglottic devices that sit above the vocal cords and form a seal around the laryngeal inlet. The use of LMAs is particularly favored in patients with mediastinal masses due to their advantage of smaller size that reduces the likelihood of obstruction by the mass, making insertion easier and reducing the risk of coughing or gagging [10].
LMAs are associated with less risk in patients with mediastinal masses as it does not require direct visualization of the vocal cords, simplifying the insertion process. Additionally, they do not block the esophagus, reducing the risk of aspiration. In the context of patients with mediastinal masses, the risk of airway obstruction is a significant concern. The mass itself can exert pressure on the airway, potentially leading to partial or complete obstruction. Laryngeal mask airways (LMAs) have been associated with a reduced risk of airway obstruction compared to other airway management techniques providing a clear pathway for ventilation [11]. In addition, use of LMA has been associated with a lower incidence of postoperative sore throat and coughing compared to endotracheal tubes. The present case demonstrates a rare case of efficient and successful airway management using LMA in a comorbid patient with retrosternal goiter. Without the closed chain of survival and the presence of appropriate equipment, the patient’s life would not have been preserved.
In present case study, a patient with multiple comorbidities, including obesity, obstructive sleep apnea, and a large retrosternal goiter, presented challenges for airway management during surgery for lipoma excision. Preoperative assessments revealed potential airway obstruction and difficulty in mask ventilation and intubation due to anatomical factors. The patient's Mallampati classification and imaging findings indicated the feasibility of using a laryngeal mask airway (LMA) as the primary airway management plan. The secondary plan included the availability of an endotracheal tube as a backup option. The induction and maintenance of anesthesia, utilizing the LMA, resulted in stable vital signs, optimal oxygenation, and successful surgical intervention. The patient's favorable response to anesthesia and smooth extubation with the assistance of suggamadex demonstrated effective airway management and recovery.