Complimentary methods to support the anaesthesia consent process are underutilized in low and middle-income countries (LMICs).
To establish whether patients who access a mobile health (mHealth) application following a pre-anaesthesia review have better knowledge of the anaesthetic process and higher satisfaction overall than those who receive a patient information leaflet.
Adult patients for elective surgery under general anaesthesia at the Aga Khan University Hospital, Nairobi.
This was a double-blind randomized control trial conducted between January and May 2019, with patients randomized to either an mHealth application or an information leaflet. The proportion of patients in each arm who achieved a set score of 9 on a survey designed to test knowledge was evaluated.
A total of 72 patients were recruited. While there was no difference in baseline knowledge between the two groups, 71.8% of those in the mHealth group and 17% in the leaflet group achieved the set score of 9 (p < 0.001). A greater proportion of patients without previous anaesthetic experience were very satisfied with the information given.
mHealth is a viable tool for information dissemination for patients in LMICs scheduled for surgery under anaesthesia, and a useful adjunct to the pre-anaesthesia review.
mHealth, Leaflet, Informed consent, Knowledge, Satisfaction
Up to 80% of health-related information supplied by healthcare personnel to patients is forgotten, with evidence that patients often have poor understanding of information provided despite signing a consent form [1-3]. It is therefore widely accepted that the pre-anaesthesia interview alone is insufficient for the provision of the necessary information required for informed consent prior to surgery, and that complementary methods should be employed [2,4]. This concept however is poorly developed in LMICs.
While there is no replacement for the verbal information provided by the anaesthetist, patient information leaflets and the use of mobile applications designed to contain the content of these leaflets may permit patients to process the information in their own time and continue to be a point of reference [5]. They may also have some use in counteracting inaccurate content on the internet and elsewhere. It is therefore critical to find measures that can improve retention of important information surrounding the anaesthetic process. Unlike patient information leaflets, mHealth applications allow the continuous addition of new information, alter information as knowledge changes and upload other modes of information transfer such as through the use of videos and other interactive programs and can be used by those who have problems with literacy [6].
The World Health Organization (WHO) describes mHealth as the “medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistances and other wireless devices” [7], and has recognized the potential of electronic-Health “to improve quality, safety and access to care” [8]. The World Bank describes an increase of mobile subscribers in Africa from 25 million to 650 million in a space of eleven years with the availability of better mobile network and cheaper smartphones more accessible to the continent. This is estimated to grow to one billion before the end of this decade. Kenya is considered to be one of the leading markets for smartphones in Africa [9].
The Global System for Mobile Communications (GSMA) estimates the number of mobile phone subscribers in Sub-Saharan Africa to be approximately 456 million, with 55% of the East African community expected to own smartphones [10]. There are at least 41 million mobile users in Kenya at present. The use of mHealth in Kenya currently includes communication with patients in chronic care such as those with HIV infection and those with non-communicable diseases [11]. Its use as an adjunct to surgery and anaesthesia care has not been explored. There is in addition paucity of data regarding the type, quantity, and format of information patients in Kenya and other LMICs want concerning their anaesthesia care. The aim of this study was therefore to establish whether patients in a LMIC who have access to a mobile health application in addition to the pre-anaesthesia review have better knowledge of the anaesthetic process and higher satisfaction overall than those who receive a pre-anaesthesia review and a patient information leaflet.
This was a double-blind, randomized controlled trial conducted at the Aga Khan University Hospital, Nairobi (AKUHN), a private 280-bed tertiary teaching hospital situated in Nairobi, Kenya. AKUHN is to the best of our knowledge one of a handful of facilities in Kenya to offer a pre-anaesthesia clinic service [12]. Current standard of care for elective surgery patients at AKUHN involves a review in the pre-anaesthesia clinic during which the process of anaesthesia is explained including anaesthetic options, risks, benefits and alternatives. Written consent is then obtained from the patient for the selected form of anaesthesia. There are currently no complementary materials (eg patient information leaflets) to support the anaesthesia consent process here.
The leaflet used in the study was derived from the patient information leaflet of the Association of Anaesthetists of Great Britain and Ireland (AAGBI) [13]. The mobile application used in this study was the Siha ® app:
https://play.google.com/store/apps/details?id=com.connecthealth.consumer&hl=en&gl=US
This mobile app allowed patients to chat with the PI and had features that provided summary data showing which patients had accessed the app during the course of the trial and had sent messages via the secure chat service. The app was customized to allow the creators of the app to generate data such as ‘the number of times a user accessed the application’, but patient personal details were not accessible to them.
The knowledge survey consisted of a set of questions ranging from who an anaesthesiologist is, why general anaesthesia (GA) is given, fasting guidelines, the process of GA, risks involved, and memory of events while under GA. These were assessed in the pre and post survey in both arms and contingency tables created to see how well each question was answered by each group. The knowledge survey also allowed free text spaces for patients to offer feedback regarding the usefulness of each method, adequacy, and clarity of information, and whether all the information they would have like to have was provided.
The primary outcome of interest was the proportion of patients who would achieve a score of 9 in an in-house survey designed to test comprehension of the elements of general anaesthesia. The questionnaire was adapted from the Standard Anaesthesia Learning Test (SALT I and II), and Snyder– Ramos’ tool for the assessment of anaesthesia knowledge and information gain [14]. We defined ‘very satisfied’ as a score of five on a 5-point Likert scale and ‘not very satisfied’ as scores of three and four.
Our target population was adult patients aged 18 years and above who were scheduled for elective surgery under general anaesthesia. We excluded patients under the age of 18 years, patients for emergency surgery and those who did not speak either English or Kiswahili. We also excluded patients who were unable to give consent for any reason such as altered consciousness, those without capacity to consent, patients receiving only sedation, local or regional anaesthesia for their procedure, obstetric patients and patients who did not visit the pre-anaesthesia clinic for their anaesthesia review. Patients who did not have a smartphone were also excluded. A smartphone was defined as a mobile phone device that performs many of the functions of a computer, typically having a touchscreen interface, internet access and an operating system capable of running downloaded apps [15].
Consecutive patients presenting to the pre-anaesthesia clinic were screened for eligibility and consent to participate obtained. Participants were randomly allocated to either arm using simple randomization. A random allocation sequence was generated by a statistician using a computer algorithm and consenting participants allocated to either arm based on this sequence. The principal investigator was blinded to the randomization. The principal investigator was blinded to the randomization.
The patient then proceeded to the pre-anaesthesia review where an anaesthetist who was blinded as to whether the patient was in the app group or not carried out an anaesthesia review. Each review lasted between 20-30 minutes. On completing the review, patients in the app group had the app downloaded onto their phones and the ones in the leaflet group were given a patient information leaflet. The information provided in the mHealth app and the leaflet in hard copy were identical. A link to the anaesthesia leaflet was provided within the mHealth app. The only difference was therefore in the medium of communication. When the participant arrived in the pre-operative receiving area of the main theatres on the day of surgery, a self-administered survey was given to them to fill.
Only the principal investigator (SB) had access to the app and chat service and could access the patients in the app group and their details. Ethical clearance was obtained from the Aga Khan University Institutional Ethics Review Committee (IERC) prior to commencement (IERC Ref: 2018/REC-75).
We required 30 patients in each arm for the primary objective (information gain) and 36 for the secondary objective (satisfaction) i.e. to compare a 30% vs. 73% proportion for information gain and 41.3% vs. 80% for satisfaction, factoring in a 20% attrition rate. Patients who did not read the leaflet or use the application were excluded from the study. Contingency tables were created to compare how well each question was answered between the two groups. Pearson’s chi-squared test was used to compare patient demographics, the proportion of patients who scored 9 on the knowledge portion of the survey, level of satisfaction with the anaesthesia consent process and association between knowledge and satisfaction between the two arms. Fisher’s exact test was used to compare the level of satisfaction with information between the two arms of the study. Independent t-tests were used to compare the mean difference in overall patient satisfaction between the mHealth group and the leaflet group.
The study took place between January 2019 and May 2019. A total of 772 patients were seen in the pre-anaesthesia clinic during the study period, 80 of whom were enrolled (Figure 1). Two patients refused to download the app, citing lack of space on their smartphones, and were excluded from the study.
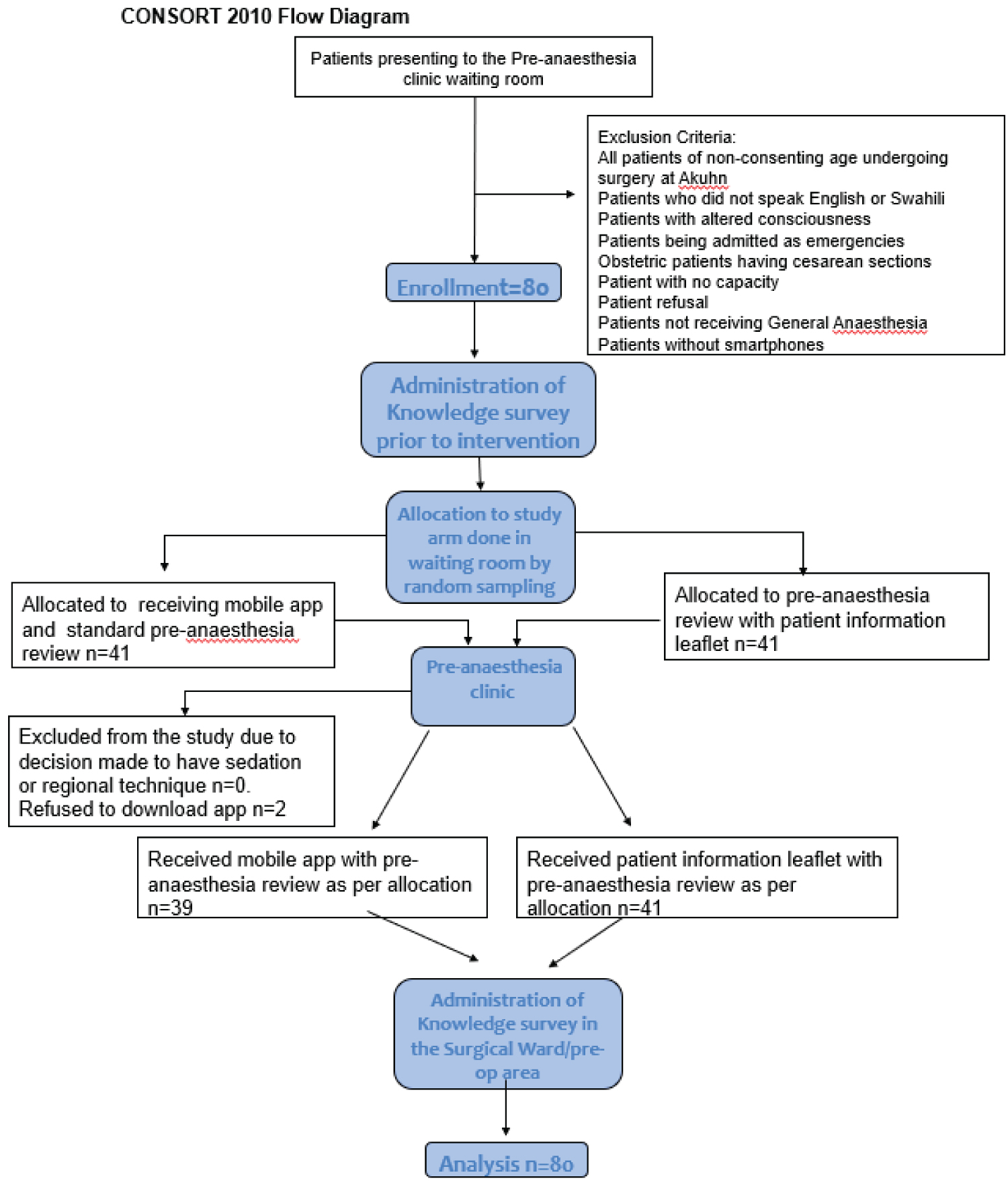 Figure 1: Participant flow diagram.
View Figure 1
Figure 1: Participant flow diagram.
View Figure 1
The majority of patients recruited were female (65%), aged between 35-44 years (45%), with university level education (56%). Most had not had anaesthesia prior to this study (Table 1). A greater proportion of patients in the leaflet arm were women (78%) compared to the mHealth arm (51.3%) (Table 2). There was however no difference between the two groups when it came to gender composition overall. The proportion of patients with previous anaesthetic experience was also similar between the two groups.
Table 1: Socio-demographic Characteristics of patients enrolled in the study receiving general anesthesia for elective surgery between January-May 2019. View Table 1
Table 2: Bivariate analysis of Socio-demographic variables of patients receiving general anesthesia for elective surgery between January-May 2019. View Table 2
Although there was no difference in baseline knowledge between the groups, more patients in the mHealth app group scored 9 in the knowledge survey post-intervention compared to the leaflet group (71.8% vs. 17%, p < 0.001) (Table 3). Improvement in the number of correctly answered questions was noted post-intervention in both groups. Overall however, the mHealth group achieved more correct answers post-intervention than the leaflet group across all questions aimed at knowledge testing.
Table 3: The proportion of patients who achieved the set score of 9 post intervention in both arms. View Table 3
The proportion of patients who were very satisfied was lower overall than of those who were not (12%) (Table 4). More patients in the mHealth group were very satisfied however compared to those in the leaflet group, with higher mean satisfaction scores in the mHealth group compared to the leaflet group. This difference was statistically significant (p = 0.0049). Although an equal number of males as females were very satisfied, female patients made up a greater proportion of those who not very satisfied. There was however no statistically difference between patient demographics and level of satisfaction.
Table 4: Level of satisfaction with information between mHealth and leaflet groups. View Table 4
There was also no association between knowledge post-intervention and level of satisfaction in either group (Table 5). More patients without previous anaesthetic experience were very satisfied with the level of information compared to those who had had prior anaesthesia previously.
Table 5: Compare level of knowledge with satisfaction in the two intervention groups. View Table 5
While most patients viewed the mobile application only once during the period of the study, one patient who viewed the content of the app 26 times. The median number of views was 3.5 IQR (2-7.5), range 1-26. A total of 36% of patients sent messages through the chats option within the app, with the majority sending messages twice (range 2-27). Questions asked via the chat services had to do with duration of the surgical procedure, post-operative sore throat, post-operative back pain, the need for a urinary catheter post-operatively and advice regarding post-operative analgesics. Feedback received regarding the app included, ‘wonderful platform, ‘more information needed,’ ‘easy to use’ and ‘difficulty downloading app due to network.’ Feedback from patients in the leaflet group on the other hand included, ‘more information needed about pain,’ ‘sufficient,’ ‘clear,’ and ‘useful.’
We conducted this study to find out whether patients in a LMIC who have access to a mobile health application in addition to a pre-anaesthesia review have better knowledge of the anaesthetic process and higher satisfaction overall than those who receive a pre-anaesthesia review and a patient information leaflet. Our results showed greater knowledge of the anaesthetic process and higher levels of satisfaction among patients who had access to a mobile health application compared to those who received a patient information leaflet.
Anaesthesia is a young specialty in Kenya, often viewed as a minor component of the patient’s surgical journey. It was therefore not surprising that even patients who had previously received general anaesthesia were unable to answer questions in the survey correctly, and that very few knew who the anaesthetist was prior to the intervention. Previous studies from other parts of the world have had similar findings, with a study from Ireland concluding that patients needed further education regarding the role of the anaesthetist and the process of anaesthesia. The fact that anaesthetists spend only a brief period of time with patients pre- and postoperatively is thought to be the major reason for this.
We observed an improvement in knowledge among all study patients regardless of intervention, suggesting that patients in LMICs who are scheduled for surgery are interested in and willing to read additional information around the anaesthetic process, if provided. A larger proportion of patients in the mHealth group than those in the leaflet group however demonstrated the requisite level of knowledge required to support informed consent. The greater knowledge gain in the mHealth may be attributable to the novelty of the intervention, ease of use and accessibility to the app at any time. Digital information provides several benefits over patient information leaflets such as increased availability, mobility, usability and individualization, instant updates, and benefits for the environment as a result of the decreased use of paper [16,17]. MHealth therefore has the potential to replace paper-based formats of information provision in anaesthesia care in LMICs. Some patients however did not have space on their smartphones to download the app, while others had difficulty downloading it due to connectivity issues. A wide range of interventions should therefore continue to be made available that are appropriate for a variety of circumstances and needs [2]. Paper-based information aids will therefore remain useful in LMICs where smartphone technology may lag behind that of more developed countries and where internet connectivity is not always stable [16].
While patients were generally happy with the information given to them, more patients in the mHealth group were very satisfied with the information received. We attribute this to the ability of patients to contact an anaesthetist whenever required, to clarify aspects of the information provided. Satisfaction is a key and emerging issue in anaesthetic care. A multicentre survey conducted in Saudi hospitals found that interaction between anaesthetist and patient as well as amount of information provided plays a key role in patient satisfaction. Feedback from both arms of the study was generally positive and requests for more information were noted in both the leaflet arm and the mHealth arm. Future studies could perhaps explore the exact type of information patients want regarding their upcoming anaesthetic and tailor tools to meet patient requirements. In an era of growing smartphone use among children, interactive media within apps could be used to sensitize children to the anaesthetic process and the theatre environment, reducing anxiety in both parents and children. App-based tools would be able to support the uploading of informational videos and could also be used as to facilitate consent form sign off once patients have read the contents of the app and had their concerns addressed. This may help improve the level of satisfaction with anaesthetic services. The mHealth app could also be trialled as a tool for post-operative follow-up after discharge from hospital.
This was a single centre study in a private institution and our results may not be generalizable. The level of education was high among study patients and the extent of smart phone ownership and utilization may not be typical of other facilities in Kenya. Secondly, it is possible that post-intervention knowledge may have been influenced by other sources of information such as internet searches as we did not control for this. However, this would have affected both arms of the study and not just the mHealth arm. Finally, unlike the mHealth arm, it was not possible to determine whether patients in the leaflet arm actually read the content as this was self-reported. The survey did however ask patients whether they had found the leaflet useful, the majority of whom said it had been, suggesting that they had indeed read it.
Patients who had access to a mobile app following a pre-anaesthesia review had better knowledge of the anaesthesia process and were more satisfied than those who receive a patient information leaflet. mHealth is therefore a viable tool for information dissemination for patients in LMICs scheduled for surgery under anaesthesia, and a useful adjunct to the pre-anaesthesia review. More LMICs should consider its use.