Epidural anaesthesia with 2% lidocaine has been reported to be more effective in caesarean section, but somato-visceral pain remains a potential complication, and can generate many dire effects including mother psychological impairment and burden. Pain during caesarean deliveries is a challenge, but any study was performed to identify risk factors associated to it.
We conducted this study to identify pain risk factors, investigate whether surgical anaesthesia length is sufficient, and discover possible correlation between pain rate and surgery duration, while assessing 2% lidocaine efficacy.
This study enrolled 612 patients who underwent scheduled caesarean section under 2% lidocaine epidural and adrenaline, at 1st affiliated hospital of Chongqing medical university in 2019. Pain was considered only for patients with successfully epidural anaesthesia. Exclusion criteria included emergencies and general anaesthesia, 100 mmhg < baseline systolic blood pressure > 140 mmhg, pregnancy term < 37 weeks and > 42 weeks. SPSS 25.0 was used and adequate tests were performed for statistical analysis. P < 0.05 was adopted for statistical significance.
Total local anaesthetic dose < 12 ml was more likely associated with pain during caesarean section than a total local anaesthetic ≥ 12 ml. Baseline systolic blood pressure < 120 mmhg was greater associated with pain during caesarean section than that > 120 mmhg. Maternal height > 160 cm was also associated pain during caesarean section.
The variables involved in pain prevalence were total local anesthetic dose, systolic baseline blood pressure, and parturient height. Surgical analgesia length was overall judged sufficient. There was no correlation between pain rate and surgery duration. The identified risk factors associated with pain will help to reduce pain incidence and will help to improve mother-baby peripartum condition.
Epidural anesthesia, Caesarean section, Lidocaine, Pain
Cesarean section (CS) is an obstetric surgery normally performed when vaginal delivery may compromise the well-being of mother and/or neonate [1]. Its prevalence went beyond the limit (10-15%) recommended by World Health Organization (WHO) [2], and reached 32% [3,4], even 46%, [5]. Prevalence exacerbation is due to the performed CS upon request, of some mothers whose reasons include pain fear of normal vaginal delivery. Not only, according to previous studies via surveys [6], avoiding pain during CS was among the greatest and leading concerns of parturients, but also, pain during CD under neuraxial anesthesia may compromise the comfortability and generate a free self-guilt of anesthesia providers, in view of it has been identified as one of the main causes for a successful medico-legal claim [7]. The surgery requires anesthetic techniques and drugs for pain-free from abdominal visceral traction [8,9], which is among important mothers' anesthetic expectations and outcome preferences [6], then, a criterion for parturients satisfaction [10] which must, moreover, be a goal of a very medical practionners. However, this ideal, is not always got [8]. Hence, pain may wreak havoc on mother and fetus, since it was linked with some mothers' depression [9,11], could impair mother-baby bonding and affect baby's health evolution in the whole puerperium time [9]. We are still wondering how psychological condition would be for those women who request CS without any medical indication supposedly to escape pain and then meet with it during CD. Many endeavors were made to overcome to this side effect by changing parturients positions, anesthetic techniques, local anesthetics and additives [12,13], nevertheless, studies are still reporting somato-visceral pain occurrence, even with 2% lidocaine epidural that recent study findings attributed many advantages such as less systemic toxicity, little hypotension rate and rapid surgical anaesthesia onset time [14], compared to other LAs commonly used in this setting. Severe somato-visceral pain during CS defined as an excruciating nociceptive sensation during CS, requiring intravenous opioids or GA, despite a successful epidural anaesthesia is, therefore, a second challenge and main preoccupation of anesthesiologist after hypotension [14]. Researchers focused on pain incidence and surgical anaesthesia onset time after epidural anesthesia with 2% lidocaine, but were not interested in the risk factors associated with somato-visceral pain prevalence. We conducted, then, this observational study in order to, mainly, identify the risk factors associated with somato-visceral pain, and evaluate the surgical anesthesia duration with lidocaine and adrenaline for assessing its efficacy. We hypothesized that, lidocaine 2% together with Adrenaline 1:200,000 in EPIA, may not have sufficient surgical anesthesia duration, and pain rate may increase with surgical duration increasing.
For this retrospective observational and institutional- based study; after ethical clearance via institutional review board of 1st affiliated Hospital of Chongqing Medical University (CQMU) (“Research ethics in 2020 (2020-526)”), we entered electronic database of anesthesiology department in The first affiliated hospital of CQMU, for extracting data of performed CS under EPIA using lidocaine2% and adrenaline 1:200,000. This institution is a tertiary and academic hospital set up at Chongqing municipality in southwestern China. Data were collected and managed according to the declaration of Helsinki of 1975 as revised in 2013. We searched medical reports of the period from January 1st to December 31st, 2019, and our foremost tool were anesthetic records and other relevant medical records as well. We collected and analyzed information of 2944 parturients but 612 parturients who had CD under epidural 2% lidocaine with adrenaline, and fulfilled our inclusion criteria have been retained as our cohort. This study adhered to the international guidelines for observational Studies according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE), 2020 statement (see file in Supplementary material/STROBE checklist). Different variables in our data collection encompassed parturients' demographic data (Age, body weight, Maternal height, Body Mass Index, American Society of Anesthesiologists status, Parity, Gravidity, gestation age), surgical data (starting and end time of surgery, fetal extraction time, estimated blood loss) and anesthetic data (amount & time of different doses of LA, vasoactive and opioid agents, muscle relaxant and hypnotic drug, sensory analgesia level , parturient position and site of epidural puncture). Apgar scores at first, five and ten first minutes, were electronically recorded and have been collected. Peri-anesthetic conduct was computerized and has been collected: Patients entered the operating theatre with an intravenous line on the forearm already started, with a crystalloid perfusion. To every parturient; at least 3 ml per minute of oxygen was supplemented after epidural puncture. Monitoring of peripheral oxygen saturation was systematically performed. Non-invasive BP and electrocardiogram were recorded continuously during the whole time of surgery. When systolic blood pressure (SBP) dropped under 100 mmhg, left uterine displacement was performed. The blood pressure fluctuation, heart rate, anesthesia onset time were also recorded and have been collected. The cases of hypotension were treated by phenylephrine and/or ephedrine. Oxytocin and dexamethasone were given to every mother.
Inclusion criteria included all admitted healthy parturients in surgery theatre for scheduled CD: SBP above 100 mmhg, less or equal than 140 mmhg, ASA physical status no more than three, singleton pregnancy, gestational age between 37 and 42 weeks, sensory block level at T8 (Thoracic dermatomal number 8) or above, without any condition contraindicating epidural anesthesia.
Exclusion criteria included multiple pregnancies, SBP less than 100 or above 140 mmhg, pregnancy age under 37 weeks or above 42 weeks, American Society of Anesthesiologists (ASA) physical status more than three, unsuccessful epidural anesthesia including sensory block level less than T8, and other conditions contraindicating elective CD. In retrospective study, important information, can be omitted, that is why, to minimize bias, we considered more than one proof as signs of severe somato-visceral pain occurrence. Hypnotic and/or opioids (fentanyl, sufentanil, remifentanil) administered after fetal extraction signified pain prevalence. Patients for whom these medications above-said had been injected before baby extraction were considered as with an unsuccessful epidural anesthesia. SBP < 90 mmhg was retained as hypotension criteria referred to many previous research considerations [15-17]. Lowest blood pressure or/and vasoactive agents' amount given helped us to recognize severe hypotension. We have, then, considered severe hypotension for parturient who received more than 50 micrograms of phenylephrine or more than 6 mg of ephedrine as vasopressor, and parturients whose SBP dropped under 90 mmhg during CS.
After data collection and compilation using Microsoft Excel spreadsheet, we checked their consistency and completeness, coded and recorded all variables into 2017 SPSS software 25.0 version, before performing appropriate statistical analysis. We expressed our data as mean, median, Standard Deviation (SD), minimum, maximum or number (%) as indicated in a descriptive statistic. All parametric and non-parametric data were tested for normal distribution and P value less than 0.05 was used to identify statistical significancy. We used chi-square test along with Odds Ratio (OR) and its 95% Confidence Interval (CI) to evaluate the difference between two categorical data within one variable, in an univariable logistic regression analysis. Categorical variables with a P value ≤ 25% in risk factors univariate analysis for somato-visceral pain, were put into multivariable model for multivariate logistic regression analysis, after adjustment of all variables included in univariate analysis. Results were displayed as Adjusted Odd Ratio (AOR) and 95% CI.
Among 2944 parturients who have been documented, 1752 women (59.51%) where found to have been undergo CS under GA or EPIA in emergency situation, and were early excluded. 1192 (40.49%) mothers underwent scheduled CS under EPIA with 2% lidocaine and adrenaline 1:200000. These 1192 patients were strictly checked. Among them, 280 with incomplete data, and unsuccessfully epidural anesthesia including sensory block level less than T8 were excluded. 35 cases of multiple pregnancies were also excluded. 116 and 140 patients have been sorted out for their baseline SBP and pregnancy age, respectively, out of normal margin as specified by our inclusion criteria. We finally retained 612 parturients like our cohort as summed up by Figure 1.
 Figure 1: Study population flow chart diagram showing how we arrive at our retained cohort.
Figure 1: Study population flow chart diagram showing how we arrive at our retained cohort.
ADR*: Adrenaline
View Figure 1
The variables collected are expressed as descriptive statistics in Table 1.
Table 1: Socio-demographic characteristic data. View Table 1
In our study, we found that the site of puncture for epidural anesthesia was L1-2 (lumbar dermatomal interspace between number one and number 2) with 71.9% and L2-3 with 28.1% of frequencies. The minimum LA injected was 8 ml, while the highest dose was 20 ml. The targeted sensory block level seemed to be T8 dermatomal, his categorical frequency reached 78.58% (Table 2 and Figure 2).
 Figure 2: The global incidence of somato-visceral pain among parturients who underwent caesarean section with xylocaine 2% and adrenaline as additive.
View Figure 2
Figure 2: The global incidence of somato-visceral pain among parturients who underwent caesarean section with xylocaine 2% and adrenaline as additive.
View Figure 2
Table 2: Baseline characteristics of categorical data of our cohort. View Table 2
Univariate severe somato-visceral pain risk factors analysis of our study showed that pain incidence increased with the lowest LA dose and biggest parturient height (Table 3).
Table 3: Univariate somato-visceral pain risk factors analysis. View Table 3
Multivariate analysis revealed that relevant factors in correlation with somato-visceral pain prevalence during CD. Table 4 recaps categorical variables in association with severe somato-visceral pain.
Table 4: Relevant factors associated with somato-visceral pain. View Table 4
All EPIA for CS in Anesthesiology department at the first affiliated Hospital of Chongqing Medical University were performed with 2% lidocaine and 1:200000 adrenalines as adjuvant. Epidural catheter was inserted mostly through L1-2 (71.9 %) and L2-3 (27.6%), exclusively in lateral position, and mainly with paramedian approach.
Our study found that the risk factors associated with somato-visceral pain were total LA dose, BSBP, and maternal height. In fact, a BSBP < 120 mmhg had great chance to experience somato-visceral pain during CS than a BSBP > 120 mmhg with a P value of 0.045, (AOR: 0.576; 95%CI: 0.334-0.993). The speculation for any reason behind this clinical observation should go in sense of little circulating volume including cerebrospinal fluid, that do not allow a good spread of LA around some nerve roots for inducing good block. Likewise, a total LA dose < 12 ml was more likely to be associated with severe somato-visceral pain during CS than a total LA ≥ 12 ml with a P Value of 0.001, (AOR: 2.576; 95%CI: 0.216-0.698). This is maybe due to the fact that LA tends to concentrate down than the top, and reverse from the top to down. As the amount of LA is smaller, as it should be insufficient to provide required analgesia from lower extremities to the whole abdominal cavity, resulting in possible somato-visceral pain. Height > 160 cm was associated with a greater likelihood of having severe somato-visceral pain during CS with a PV of 0.046, (AOR: 0.320; 95%CI: 0.073-1.405). The explanation for this is that: As LAs tend to concentrate downwards, as surgical anesthesia intensity will go diminishing from thoracic dermatomes, then abdominal and pelvic dermatomes. Therefore, traction or handling of intra-peritoneum organs may result in increased somato-visceral pain for taller women than smaller. Pain incidence increased by the decrease of total LA dose and parturients 'height. Our results demonstrated that a dose of 12-17 ml was associated with a relatively little hypotension incidence without any distressed neonate. Early, a study had showed that a total dose of 23 ml of 2% lidocaine with adrenaline displayed 13.6% of hypotension incidence without any cardio-systemic toxicity sign [18]. Research with more 23 ml in co-administration of lidocaine, epinephrine, bicarbonate and fentanyl resulted in 12% of pain rate [19]. Natan Weksler, et al. demonstrated how the increased dose of bupivacaine from 7.5-10 mg to 10-12.5 mg decreased the pain rate from 75% to 31.6%. Therefore, 12 ml as total dose of 2% lidocaine with adrenaline can be recommended as a minimum dose, but still needed a heated debate for polarized options approval or further investigations to fix a cut-off of a maximal total LA dose in this area based on each parturient height, in purpose to achieve the ideal of pain-free [9]. Xiangqi di, et al. [7], who suggested a determination of optimal dose, by considering the maternal height strongly supported our point of view. We had hypothesized that lidocaine 2% together with Adrenaline 1:200,000 as additive, in Epidural Anesthesia, does not have sufficient surgical anesthesia duration and pain rate may increase with surgical duration increasing. Comparing different CD durations (≤ 45 min, > 45 min), we did not find any statistically significant difference, with a p value of 0.480, (OR: 1.248, 95%CI: 0.675-2.308). Many surgical durations (≤ 45 min, > 45 min, ≥ 60 min, ≥ 80 min in Figure 3) comparison did not neither display any significant difference. We only noted a rise of the curve in category of ≥ 80 min as surgical duration, and two patients out of seven (28.6%) in this category experienced somato-visceral pain during surgery. As the sample size (1.14% of the whole sample) was so small, we could not make conclusion. Otherwise, further investigations with enough samples of this category are necessary. These anti-hypothesis findings may enlighten and dissuades pessimistic anesthesia providers about lidocaine length surgical anesthesia. Moreover, a large systematic review and other studies found as highest CS durations means of nearly 52 min, including high BMI women category that is known to lengthen the anesthesia procedure and surgical durations [7,17,20]. Lidocaine 2% can, therefore, be chosen for the all-cesarean indications allowing neuraxial anesthesia without fear about surgical analgesia length, all the more reason that previous studies said it is less toxic, presented little hypotension incidence, and rapid surgical anesthesia onset compared to other many local anesthetics commonly used in CS epidural anesthesia [14,19] (Figure 4).
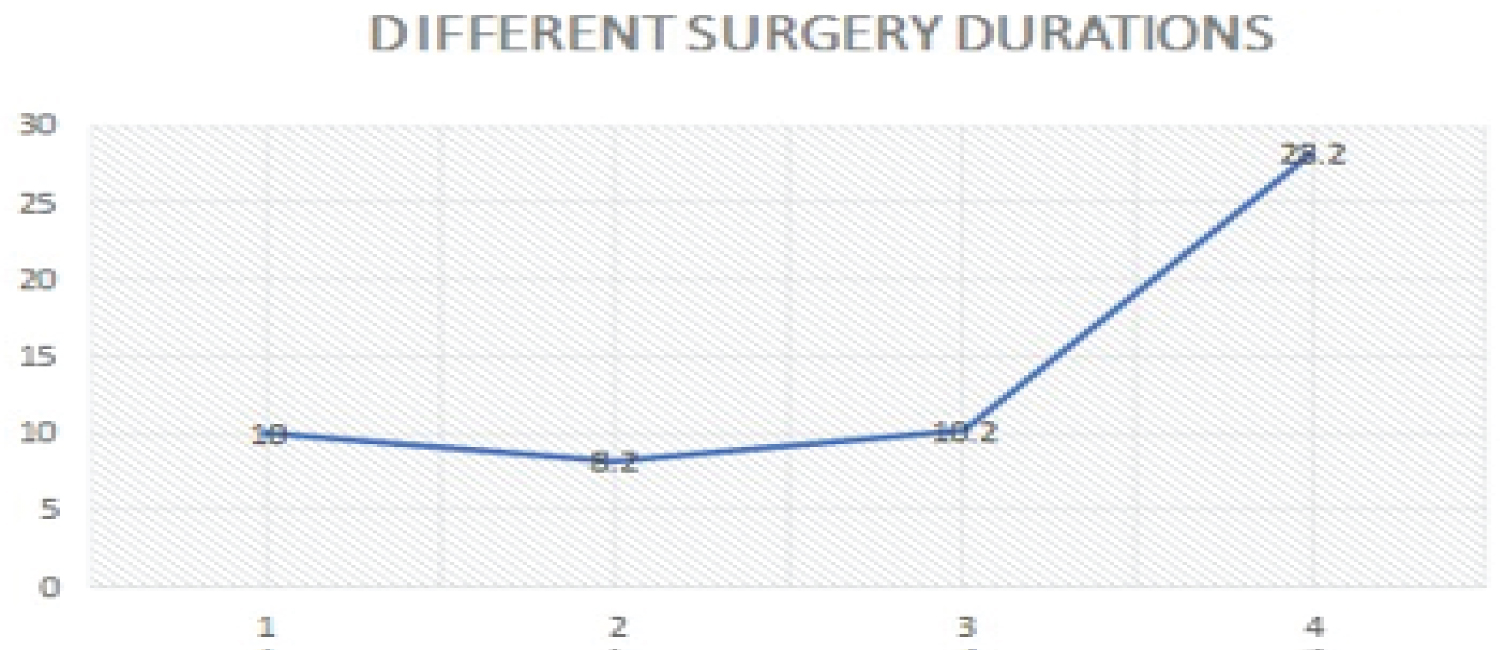 Figure 3: Graphic shows how pain rate evolved with increasing surgery duration.
Figure 3: Graphic shows how pain rate evolved with increasing surgery duration.
1 = pain rate with a surgery duration ≤ 45 min was 10%, 2 = pain rate with a surgery duration > 45 min was 8.2% , 3 = pain rate for a surgery duration of ≥ 60 min(n = 49 = 8%) was 10.2%, 4 = pain rate for a surgery duration of ≥ 80 min (n = 7 = 1.14%) was 28%.
View Figure 3
 Figure 4: Hypotension rate in parturients who underwent scheduled cesarean section.
Figure 4: Hypotension rate in parturients who underwent scheduled cesarean section.
1 = hypotension rate (13.3%), 2 = No hypotension (86.7%).
View Figure 4
The general somato-visceral pain incidence in our study was 9.47%, with one EPIA converted to GA with endotracheal intubation. Our findings are very close to Sharawi N, et al. study's findings in lidocaine-use with 3 additives [21], in purpose to achieve the highest quality of surgical analgesia, but better compared to 3% chloroprocaine results [21], and other many previous studies, with different LAs, additives, different anesthesia techniques and positions [13,20,22-24]. It is actually known that epidural adrenaline has antinociceptive properties and enhances analgesia duration when co-administered with Las [25-26]. In addition, Aliza Olapour, et al. recently found that sensory and motor block with lidocaine were superior to the ropicaine's, and added adrenaline exerts important role [25-27]. Recent Japanese clinical research let know that, the more cephalad the epidural catheter is, better the quality of analgesia is [28]. It did, nevertheless, not find any difference between epidural catheter placed in T10-11 and T11-12 spaces in post-CD for pain alleviation. It also argued that the LA injected into lumbar for CD may not provide sufficient analgesia in the lower thoracic dermatome. Based on our findings and this research result, we concluded that the reasons of lower pain incidence in our study include the site of puncture mainly in L1-2 interspace. It seems that the optimum pain relieve is obtained when epidural catheter is placed between the highest lumbar and lowest thoracic dermatomes.
Our study did not find any distressed new-born at 1st, 5th and 10th min. Three neonates had 8/10 of Apgar score but had already become 10/10 at 5th min. Our findings are similar to Chantal T. Crochetière and co-worker's results [29]. Researchers considered distressed neonates those with Apgar score < 7/10 [23,29], and Sandra Kampe, et al. found some distressed neonates in their study [29]. This permits a conclusion that 2% lidocaine-adrenaline did not induce abnormal Apgar score for new-bons in the conditions of our study. Our research found a hypotension rate of 13.3% which is relatively lower compared with many previous studies [15,29], in this area. These best results is probably due to the site and position of puncture in our study, as supported by other researches [11,15,16,30].
The literature is short of data about factors associated with pain incidence and length of surgical anesthesia time when 2% lidocaine-adrenaline is applied for CS. We would like to use the visual analogue scale, level three, as other criterion of severe somato-visceral pain, but it was not recorded. Inadequate insertion of epidural catheter because of little experience of resident physicians in anesthesia training may result in increased pain incidence or exclusion of some patients in our study. The list of identified risk-factors associated with somato-visceral pain in our findings may not be exhaustive; we encourage then other investigations on this topic after removing the afro-mentioned limitations. The pain and hypotension rates should be interpreted with caution in sense that even slight change of analgesia sensory block level consideration and hypotension definition, are likely to yield substantial modifications.
The variables associated with somato-visceral pain were BSBP, total LA dose and maternal height. The length of surgical anesthesia was overall judged enough, while the pain rate was not increased by the increasing duration of CD. Identified pain risk factors will contribute to build up a front-line against pain, in so far anaesthesia providers will be awake, willing to recognize parturients likely to have severe pain and should then take preventive strategies. Corollary, pain incidence should considerably decrease. This will improve the mother-baby conditions in peripartum and puerperium time, and it is susceptible to increase the mother's satisfaction inasmuch as pain- free was cited as great parturients' concern, anesthetic expectations and outcome preferences, and an important consideration for mothers' satisfaction. The pain and hypotension rates were relatively lower in our study compared to the findings of previous studies using lidocaine or other local anesthetics, while any neonate was found distressed. Hereby, 2% lidocaine and adrenaline as additive, confirm their efficacy and safety, in the specific constellations hyphenated to our study.
Raw data for this study are available and maybe provided upon request.
None.
None.
We would like to thank Drs Astère, Laurent and Mork for their technical support and language edition.