Endovascular treatment of acute stroke patients with tandem lesions is technically challenging. We sought to evaluate clinical and interventional factors that might influence the clinical outcome in these patients.
We retrospectively analysed the interventional and clinical data of patients with tandem lesions and acute embolic stroke in the anterior circulation that underwent endovascular stroke treatment at our institution. Patients were selected if they had a CTA-proved vessel occlusion of the distal ICA or M1/2 segment and absence of early signs of advanced infarction (ASPECT score ≥ 6). The primary endpoint of this study was the proportion of patients with good clinical outcome (mRS-score ≤ 2) at 90-day-follow-up. A multivariate analysis (Random forest approach) was used to investigate the effect of several clinical and interventional factors on clinical outcome.
From January 2012 to February 2018, 41 patients (mean age 65.5 ± 10.2 years; female, n = 12) with tandem lesions in the anterior circulation (Carotid-T, n = 11; M1, n = 25; M2, n = 5) underwent endovascular treatment at our institution. Stenting of the extracranial ICA and successful recanalization of the occluded vessel segment (TICI 2b/3) was possible in all cases. A good clinical outcome at 90-days-follow-up (mRS ≤ 2) was documented in 25 of 38 patients (65.7%). The overall complication and mortality rate was 10% and 17%, respectively.
In multivariate testing, a favourable clinical outcome on follow-up correlated with a younger age (< 70 years), a more peripheral intracranial vessel occlusion (M1/M2 versus Carotid-T), and good cerebral collaterals (p < 0.05). Interventional factors had no statistical effect on clinical outcome.
Interventional treatment of acute stroke patients with tandem lesions is technically feasible and safe. A favourable outcome may be achieved in the majority of patients and is most probable in younger patients with peripheral intracranial occlusion and good cerebral collaterals.
Tandem lesions, Endovascular stroke treatment, Carotid stenting, Thrombectomy, Multivariate analysis, Random forest
Since the publication of the results of the randomized trials on mechanical thrombectomy (MT) in 2015, MT has become an established treatment option in the management of acute stroke patients in neuro-vascular centres worldwide [1-5]. In approximately 10%-20% of patients with stroke, additional ipsilateral high-grade ICA stenosis is present [6]. Endovascular treatment patients with tandem lesions is challenging [7-9] as it complicates endovascular access and requires more technical skills than MT for intracranial occlusion alone. Moreover, primary stenting of the extracranial occlusion may lead to a delay in recanalization of the target vessel occlusion. On the other hand, patients with high-grade ICA stenosis might profit from pre-existing intracranial collaterals that-theoretically- can extend the time window for endovascular treatment in terms of beneficial clinical outcome.
The aim of this study was to evaluate different clinical and interventional factors that may influence the clinical outcome in these patients.
The study was approved by the local ethics committees. We retrospectively analysed the interventional and clinical data of patients with acute embolic stroke in the anterior circulation and a cervical high-grade atherosclerotic stenosis or occlusion of the ipsilateral internal carotid artery that underwent endovascular stroke treatment and simultaneous stenting of the ICA at our institution from January 2012 to February 2018.
Patients were selected for endovascular stroke treatment if they had a CTA-proved vessel occlusion of the distal ICA or M1/2 segment and absence of early signs of an extensive and advanced infarction (ASPECT score ≥ 6). Only patients with concomitant atherosclerotic lesions of the extracranial ICA were included into the study; patients with dissections or chronic occlusions were not included.
All procedures were executed by experienced interventional (neuro) radiologists (> 40 MTs/year). The choice of the interventional technique and the devices used was left to the discretion of the interventionist. All procedures were performed under general anaesthesia.
An 8F sheath (Super Arrow-Flex, 8F, Arrow International, Reading, PA, USA) was placed into the affected common carotid artery via a transfemoral access. After exposure of the ICA-bifurcation, the stenosis or occlusion was passed with a 0.014-inch microwire and pre-dilated with a PTA-balloon to allow fast access to the intracranial vasculature. If passage of the stenosis with an intermediate catheter was possible without immediate stent placement, stenting of the ICA was performed after thrombectomy ("retrograde stenting"). Otherwise, stent implantation was performed prior to cerebral thrombectomy ("antegrade stenting"). Self-expanding stents with closed-cell design were used in all cases (e.g., Wallstent, Xact-Stent, Caspar); additional balloon angioplasty was performed under cardio-protection with atropine.
For intracranial thrombectomy, an intermediate catheter (6F Sophia or Sophia Plus; Microvention, Aliso Viejo, Ca, USA) was advanced through the stent and positioned as close to the thrombus as possible. Mechanical thrombectomy was performed with a stent-retriever (Solitaire, Medtronic, Irvine, Ca, USA) under continuous distal aspiration.
Follow-up CT imaging was performed 24-36 hours after the procedure or whenever clinical worsening occurred. Haemorrhage was classified according to the European Cooperative Acute Stroke Study (ECASS)-2 classifications. Patients were assessed clinically on admission (NIHSS), at discharge (NIHSS, mRS), and on follow-up after 90 days (mRS). Imaging and interventional data were reviewed by two interventionalists (R.E., S.R.).
The primary endpoint of this study was the proportion of patients with good clinical outcome after endovascular stroke treatment, defined by a modified Ranking Scale (mRS)-score ≤ 2 at 90 day follow-up. Follow-up outcome was assessed during an in hospital visit or by a semi structured telephone interview by a neurologist not blinded to the initial treatment.
To investigate the influence of different factors on the clinical outcome after endovascular treatment, we analysed several clinical and interventional parameters (Table 1). Data were extracted from the prospectively collected stroke database of our institution. Continuous data were collected in a data base and described by median and interquartile range or as mean and SD in case of normal distribution. Differences between quantitative and categorical variables were tested for significance using the student's t-test and the chi-square testing, respectively. The effect of different variables on clinical outcome was tested by [1] a dichotomised approach comparing the proportion of patients with an mRS ≤ 2 versus mRS ≥ 3, and [2] a multivariate analysis using a machine learning algorithm approach (random forest) with the statistical software "R", version 3.4.2 (https://cran.r-project.org/bin/ windows/base/old/3.4.2/). The Random Forest is a machine learning algorithm that creates thousands of decision trees, giving an estimate of what variables are important in the classification. It is an effective method for estimating missing data and maintains accuracy when a large proportion of the data are missing. A p-value of 0.05 was considered as statistically significant.
Table 1: Interventional and clinical factors that were tested for the effect on clinical outcome after endovascular treatment of patients with tandem lesions (n = 41). View Table 1
From January 2012 to February 2018, 41 patients with tandem lesions in the anterior circulation were identified that matched the inclusion criteria of this study. Gender, age and clinical data of the patient cohort are given in Table 2. Recanalization of extracranial ICA and thrombectomy of the occluded vessel segment was possible in all cases. Overall, the mean number of thrombectomy manoeuvres was 2.0 [1-7], the mean time from groin puncture to the end of the procedure was 123 ± 44 min. (59-242). Antegrade stenting of the extracranial ICA was performed in 19 patients (46%).
Table 2: Clinical data of 41 patients with tandem lesions of the anterior circulation. View Table 2
NIHSS at discharge was 9.8 ± 12 (0-42). Regarding the primary endpoint, mRS @90 days was available in 38 patients (92.6%). A good clinical outcome (mRS ≤ 2) was documented in 25 of 38 patients (65.7%). There were three major bleedings and one new pontine infarction after the intervention, resulting in a complication rate of 10% (4/41). Overall, the mortality rate was 17% (7/41).
In multivariate testing, a favourable clinical outcome (mRS ≤ 2) correlated with a younger age (< 70 years; p = 0.010), a more peripheral intracranial vessel occlusion (M1/M2 versus cartid-T; p = 0.008), and good cerebral collaterals (Tan > 2, p = 0.012; Table 3 and Figure 1). Interventional factors had no statistical effect on clinical outcome. However, there was a tendency toward a more favourable outcome in patients that underwent antegrade stenting.
Table 3: Effect of dichotomized clinical and interventional factors on favourable clinical outcome (mRS ≤ 2 at 90 day follow-up). View Table 3
The aim of this study was to investigate the influence of different clinical and interventional factors on the outcome of stroke patients that underwent endovascular treatment of tandem lesions. A favourable clinical outcome at follow-up correlated significantly with a younger age, a more peripheral intracranial vessel occlusion, and good intracranial collaterals. The latter feature is known to play a crucial role in stroke treatment in general, as the existence or absence of intracranial collaterals does directly influence the size of the infarct core, the tissue at risk (penumbra), and a potential time window until successful recanalization [10-13]. It is therefore not surprising, that the grade of intracranial collateralisation had an impact on clinical outcome in our patients, as the treatment is more complex and often more time consuming than in "simple" thrombectomy. Good collaterals extend the time window for successful recanalization and might influence indirectly the grade of the neurological deficit.
Similar to the results of Park, et al. [14], we found that patients with a high-grade stenosis had a trend for a better outcome than those with complete occlusion of the extracranial ICA, however, this finding did not reach statistical significance (p = 0.052). Other clinical features, such as the initial NIHSS, the ASPECT-score on admission, or the affected hemisphere, did not influence long-term outcome (Figure 1).
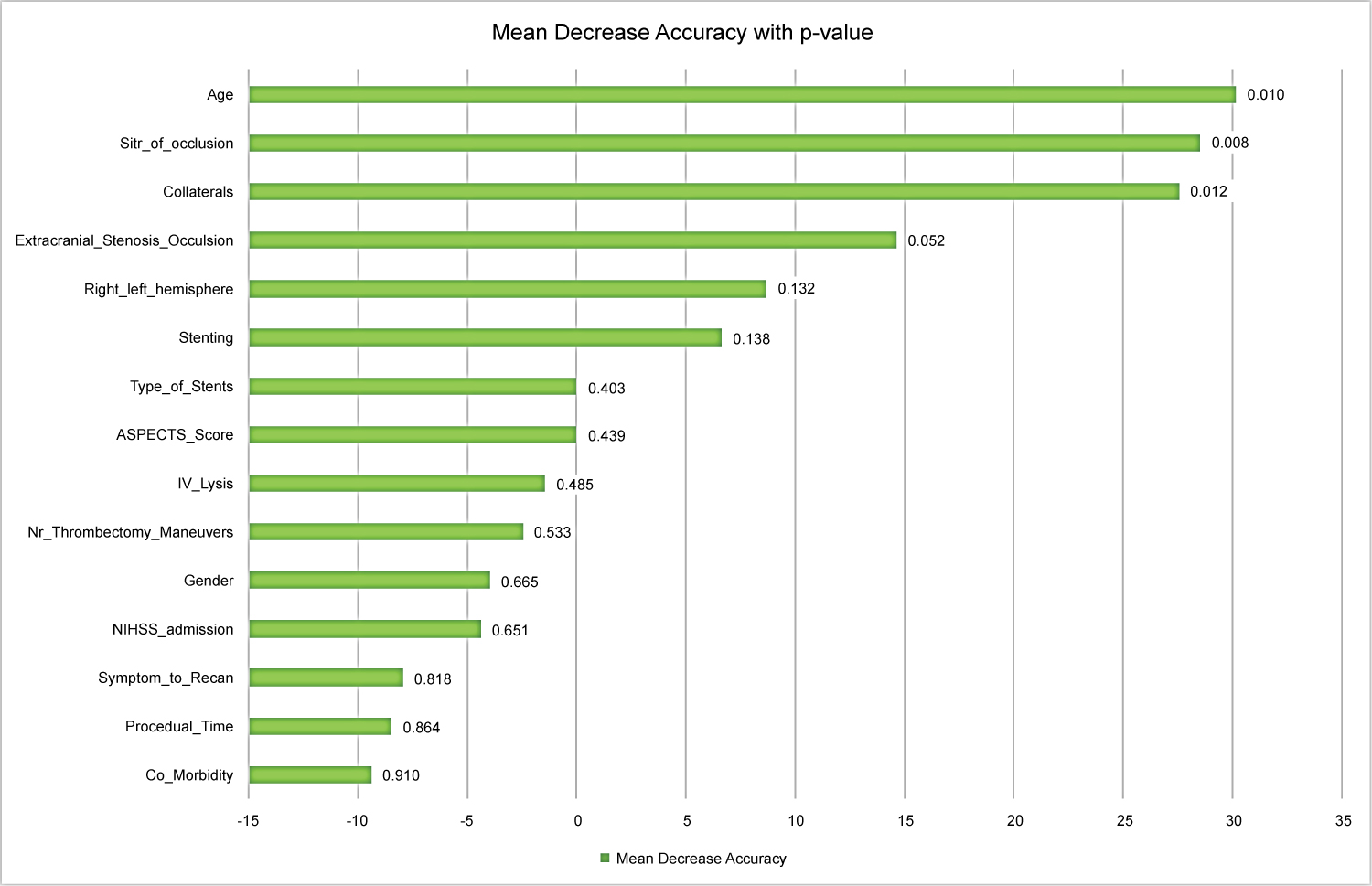 Figure 1: Impact of clinical and interventional factors on good clinical outcome at 90-days-follow-up (mRS ≤ 2) in 41 patients that underwent acute stroke treatment with tandem lesions. The graph shows the mean decrease in model accuracy for each feature; the corresponding p-value is given behind each bar.
View Figure 1
Figure 1: Impact of clinical and interventional factors on good clinical outcome at 90-days-follow-up (mRS ≤ 2) in 41 patients that underwent acute stroke treatment with tandem lesions. The graph shows the mean decrease in model accuracy for each feature; the corresponding p-value is given behind each bar.
View Figure 1
Interestingly, we did not found interventional factors to have a major effect on clinical outcome in our cohort, either. There was a trend for a better outcome in patients that underwent antegrade stenting in comparison to retrograde stenting, however, the factor did not reach statistical significance. Other interventional factors, like the number of thrombectomy manoeuvres, the procedural time or the type of stent, had no statistical effect. An explanation for this finding might be the high proportion of technical success and the relatively high fraction of the patients with a favourable clinical outcome in our study that did not allow for a more technical in-depth-analysis in a rather small population. However, from a more clinical point of view, our analysis provides evidence that patients with good intracranial collaterals and more peripheral occlusions have a high chance of a favourable outcome if they are treated successfully - independently from a specific treatment algorithm or an exact time window.
Our findings are in most parts in line with the results of other groups [15-19], however, they differ regarding the issue of antegrade versus retrograde stenting. The STRATIS collaboration group [15] demonstrated equipoise concerning antegrade vs. retrograde stenting in a prospective, non-randomized mutlicentric study with 147 patients. In contrast, Maus, et al. analysed the long-term outcome of one hundred patients after endovascular treatment of tandem lesions and found that the retrograde strategy yielded a significantly higher rate of successful reperfusion and a higher rate of favourable clinical outcome after 90 days [16]. This might be explained in parts by a faster recanalization of the intracranial vessel occlusion, when the extracranial stenosis or occlusion of the ICA is initially treated by PTA only. Moreover, a retrograde stenting approach allows for a more individual and careful decision making with regard to antiplatelet treatment in the acute setting, probably leading to a lower rate of harmful post-interventional bleedings [17]. For example, using the retrograde approach, the physician can decide not to stent immediately a moderate extracranial stenosis in a patient with unknown or long lasting symptom onset, when there is no relevant impact on the flow. Or he can decide to modify the antiplatelet regimen after stenting according to the individual situation (e.g. monotherapy with ASS or Gp2b3a-Antagonist). This is much more difficult when using the antegrade approach: Because of the limited or missing antegrade flow in the ICA before re-opening of the intracranial vessel occlusion, immediate and effective antaggregation is needed to avoid acute re-occlusion of the ICA-stent and has to be maintained, even when the intracranial recanalization is time consuming or complicated.
The major limitation of this study is its small size. The relatively low number of treated patients together with a high technical success rate influenced our statistical analysis especially with regard to interventional factors that didn’t show any statistical effect on clinical outcome in our cohort as stated above. We tried to overcome these limitations by using a more progressive statistical algorithm for multivariate analysis (Random Forest), however, it is possible that some of the results that are assumed to have little or no statistical effect may not have had enough statistical power. For instance, the number of thrombectomy manoeuvres shows an estimated 23% absolute impact on good outcome proportion (Table 3): This is certainly clinically relevant, but comparisons in this range of proportion are likely to be underpowered.
Moreover, there was no core lab assessment for clinical and/or interventional features. This issue might have influenced especially the angiographic outcome of the interventions. We tried to overcome this limitation using a consensus reading for the assignment of the TICI-score, performed by two experienced neuroradiologists (S.R., R.E.); however, this cannot completely rule out a methodical overestimation of our findings.
Interventional treatment of acute stroke patients with tandem lesions is technically feasible and safe. A favourable outcome can be achieved in the majority of patients and is most probable in younger patients with more peripheral intracranial occlusions and good collaterals.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
There are no competing interests to declare.
1. Rachid Elmouden: Design of the study, acquisition and analysis of the data, critical revision of the work, final approval of the manuscript,
2. Ana Moya: Design of the statistical analysis of the data, critical revision of the work, final approval of the manuscript,
3. Gernot Reimann: Acquisition of the data, critical revision of the work, final approval of the manuscript,
4. Olaf Adamczewski: Acquisition of the data, critical revision of the work, final approval of the manuscript,
5. Michael Schwarz: Interpretation of datacritical, revision of the work, final approval of the manuscript,
6. Stefan Rohde: Conception and design of the study, acquisition and analysis of the data, critical revision of the work, final approval of the manuscript.