Meniscal repair surgery is currently one of the most commonly performed orthopedic procedures. All-inside meniscal repair is simple and often sufficient for meniscal healing. Nevertheless, as with any other surgical technique, they are associated with complications that must be highlighted for better results and to avoid revisions for unjustified meniscectomies. To our knowledge, all inside anchors (FasT-Fix 360Ⓡ, Smith & Nephew, Inc., USA) pulling out and impinging on the deep fibers of the medial collateral ligament in the late post-operative period have not been described previously. These injuries should be considered in the event that a patient presents with sudden pain and mechanical symptoms after meniscal repair despite having favorable early post-operative outcomes.
Level of Evidence: V "Case report"
Meniscus, Repair, Suture, Fast-Fix, Complication
Meniscal lesions are common injuries encountered in orthopedic practice among the general and physically active population. Meniscal repairs are increasingly frequent owing to the advent of new and simple fixation technologies [1]. Several techniques have been described for meniscal repair; of these, the all-inside repair technique has gained popularity due to its technical simplicity, short operative time, and reduced risk of complications [2]. The FasT-Fix anchor system (Smith & Nephew, Inc., USA) was designed to delivera tight mattress suture configuration between fixed anchors, providing a strong, reproducible, and easy meniscal repair with a mean success rate of 86% over up to 12 years follow-up [3-5]. However, despite its biomechanical properties, suture failure has been reported as the predominant mode of failure [6]. Other described complications include local tissue injury, synovitis, and implant-related complications such as implant migration through tissue, breakage, and failure of deployment [7-10]. In this report, we describe an unusual complication associated with the all-inside FasT-Fix meniscal repair system, which has not been previously reported.
A 36-year-old manual laborer presented to our clinic limping and complaining of pain with a history of rotational traumatic injury to his right knee with an audible crack at his workplace when descending from a platform 1 month ago. His surgical history included an operation of the right knee for post-traumatic patellar instability at the age of 16 years. The patient underwent osteotomy of the anterior tibial tuberosity with vastus medialis plasty. Physical examination revealed normal knee alignment, minimal joint effusion without signs of inflammation, an internal meniscal pain point, and normal joint amplitudes (range of motion: 0-130°). There was no instability in the frontal or sagittal plane, with a positive McMurray test of the medial meniscus. Radiological assessment showed a peripheral flap tear of the posterior horn and a vertical longitudinal tear of the middle aspect of the medial meniscus as well as patellofemoral chondropathy related to a history of patellar instability (Figure 1 and Figure 2).
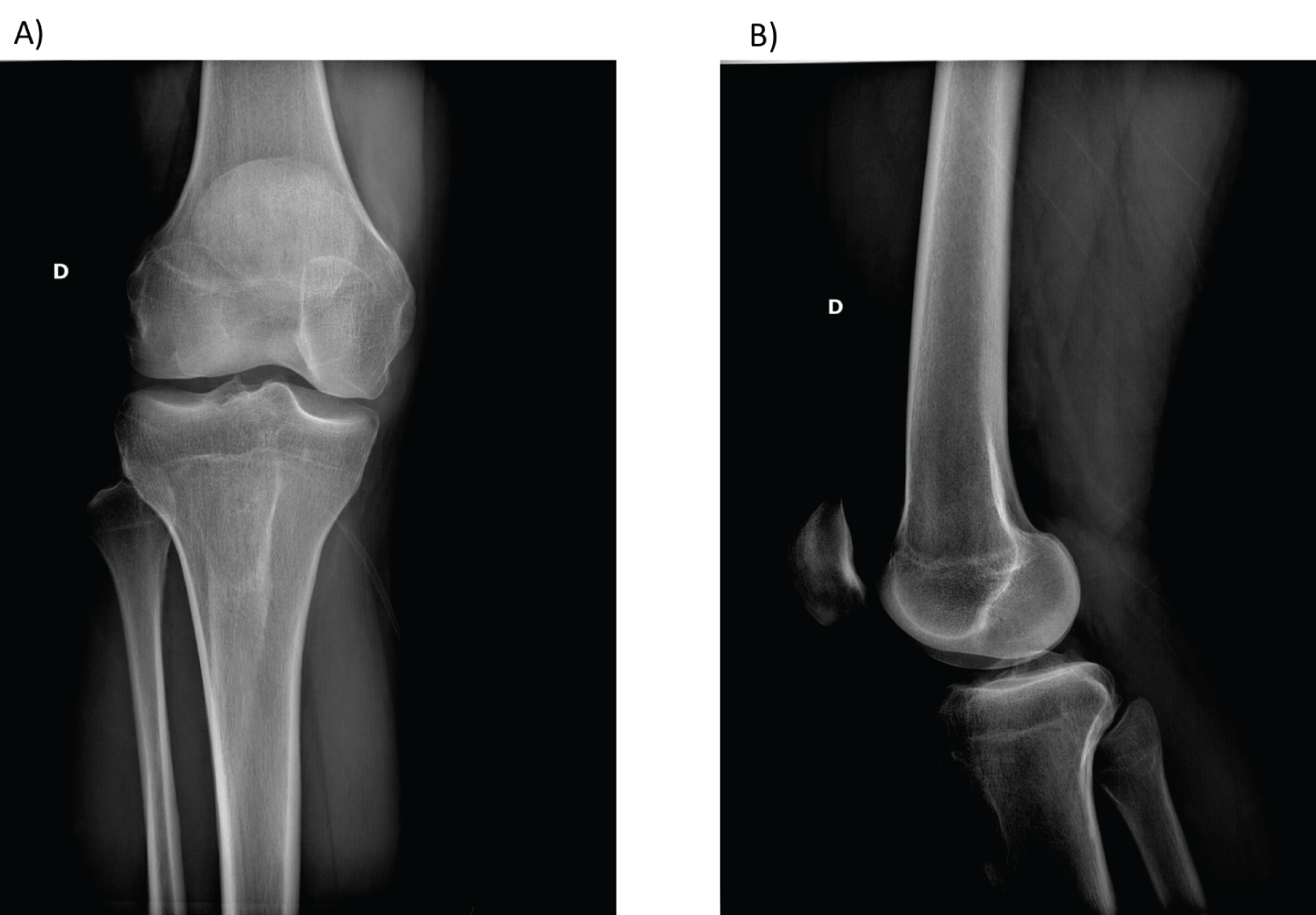 Figure 1: Initial presentation X-ray. (A) AP view of the knee; (B) Lateral view of the knee.
View Figure 1
Figure 1: Initial presentation X-ray. (A) AP view of the knee; (B) Lateral view of the knee.
View Figure 1
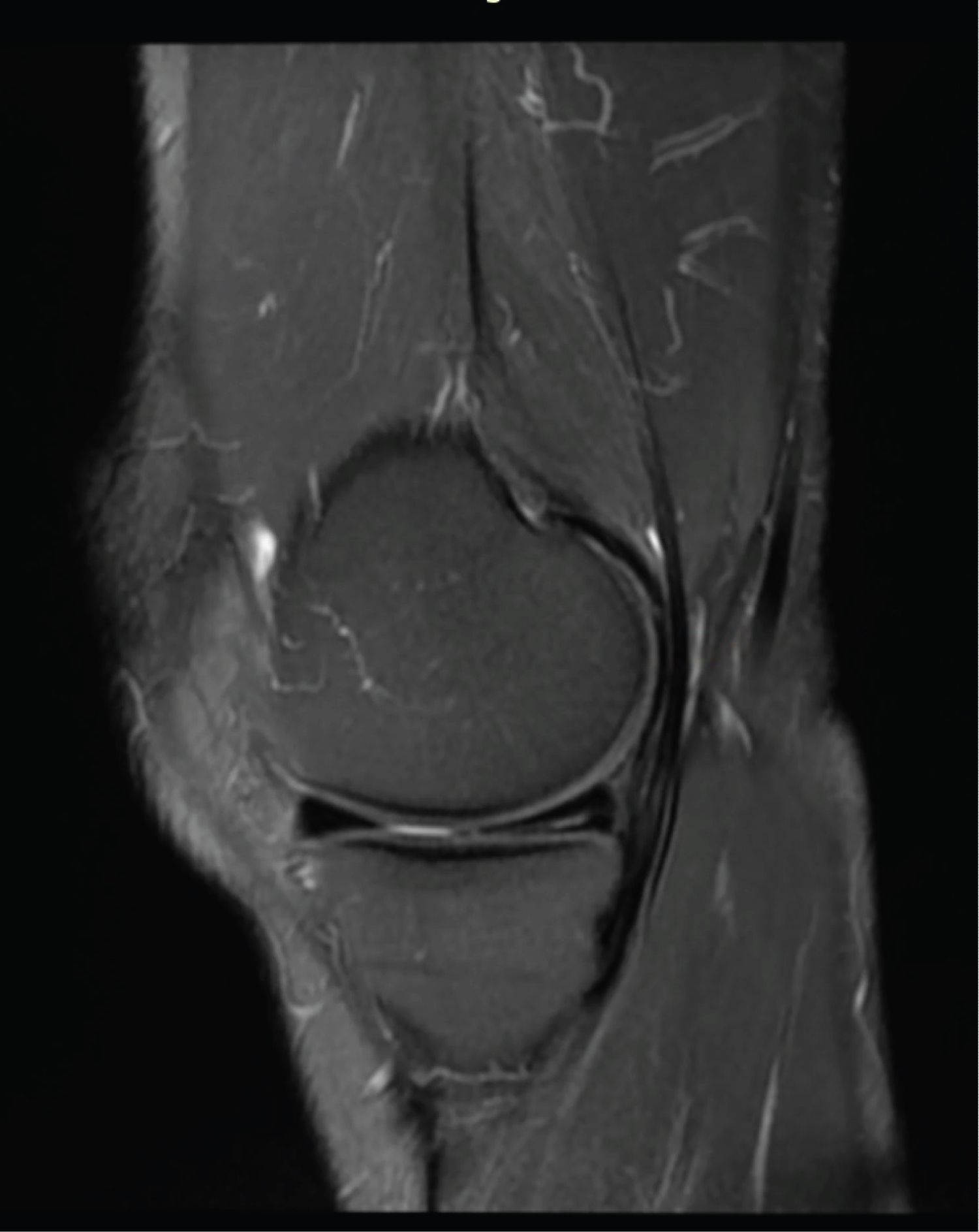 Figure 2: MRI sagittal view showing a peripheral flap tear of the posterior horn and a vertical longitudinal tear of the middle aspect of the medial meniscus.
View Figure 2
Figure 2: MRI sagittal view showing a peripheral flap tear of the posterior horn and a vertical longitudinal tear of the middle aspect of the medial meniscus.
View Figure 2
The patient underwent arthroscopic minimal excision of the unstable flap tear followed by meniscal repair using three all-inside FasT-Fix sutures (Smith and Nephew Inc.) in a horizontal mattress fashion, penetrated at a 16-mm depth of in the middle and posterior segments of the medial meniscus. No other lesions were observed in the lateral meniscus. Surgery was performed as expected without complications. The post-operative care protocol authorized partial weight-bearing and mobilization of the knee at 0-90° for 6 weeks. At the 6-week post-operative follow-up visit, the findings were favorable, with a slightly painful knee and walking without limping or walking aids. Clinical examination showed slight joint effusion in a stable knee with normal mobility (0-130°). Three months postoperatively, the evolution was satisfactory despite the persistence of pain in certain positions (hyperflexion). Clinical examination revealed a dry and stable knee with normal joint mobility and a negative McMurray test of the patient had pain on palpation of the internal femorotibial space. However, 8 months postoperatively, the patient presented with significant disabling knee pain localized anteromedially to the knee joint, associated with a sudden decrease in motion. Magnetic resonance imaging (MRI) findings were unremarkable and failed to identify the cause of sudden pain and impaired functionality of the knee joint. Arthroscanner findings revealed the presence of a small meniscal fissure at the junction between the posterior horn and the body of the medial meniscus communicating with the articular surface on the femoral side (grade 3) with the presence of internal parameniscal cysts but failed to identify the loose anchor plate (Figure 3). An echography of the knee was performed and demonstrated impingement of the anchor plate of the FasT-Fix material on the deep fibers of the medial collateral ligament that appeared thickened and hypoechogenic with a loss of the fibrillar aspect on contact (Figure 4 and Figure 5).
 Figure 3: Arthroscanner findings revealing the presence of a small meniscal fissure at the junction between the posterior horn and the body of the medial meniscus communicating with the articular surface on the femoral side (grade 3).
View Figure 3
Figure 3: Arthroscanner findings revealing the presence of a small meniscal fissure at the junction between the posterior horn and the body of the medial meniscus communicating with the articular surface on the femoral side (grade 3).
View Figure 3
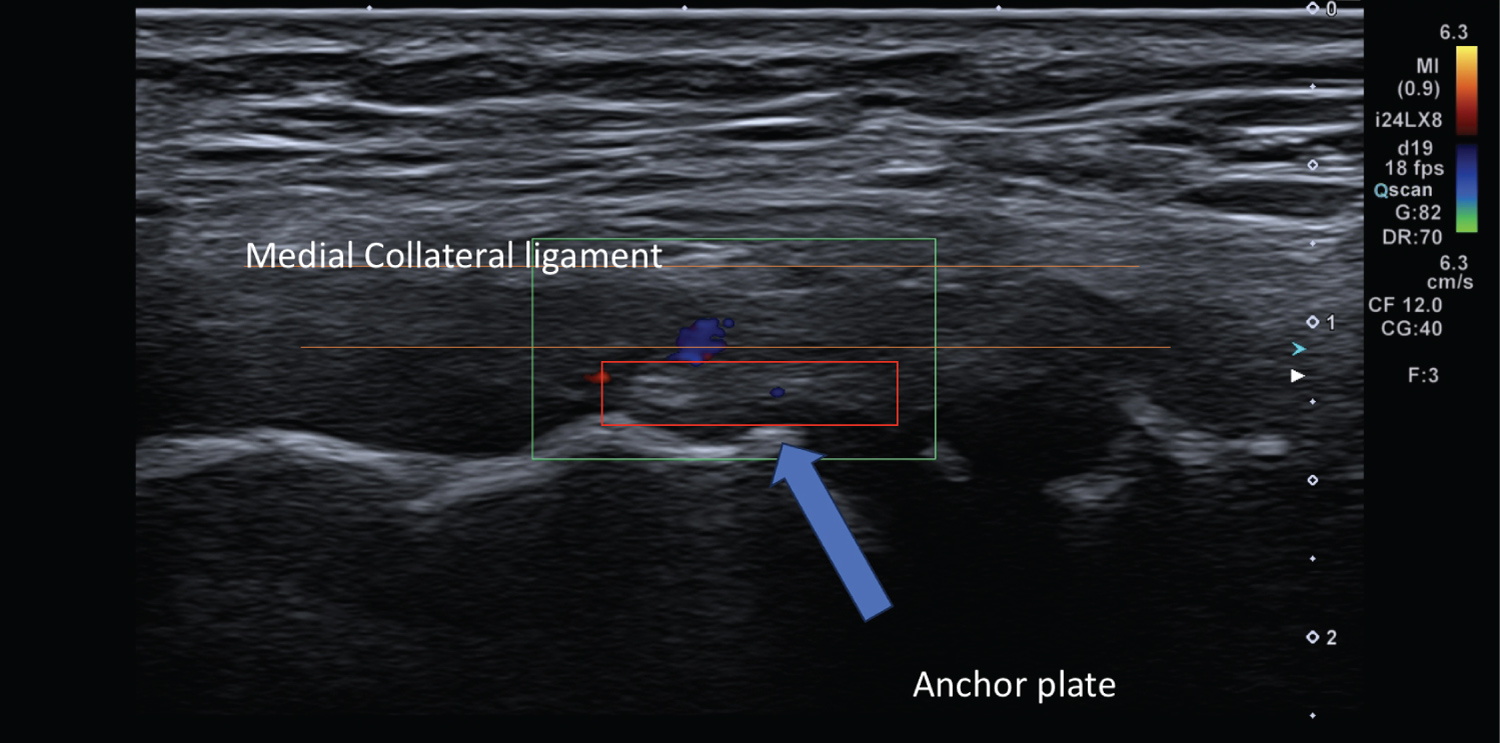 Figure 4: Echography of the knee: Sagittal view of the knee demonstrating the impingement of the anchor plate of the FasT-Fix on the deep fibers of the medial collateral ligament.
View Figure 4
Figure 4: Echography of the knee: Sagittal view of the knee demonstrating the impingement of the anchor plate of the FasT-Fix on the deep fibers of the medial collateral ligament.
View Figure 4
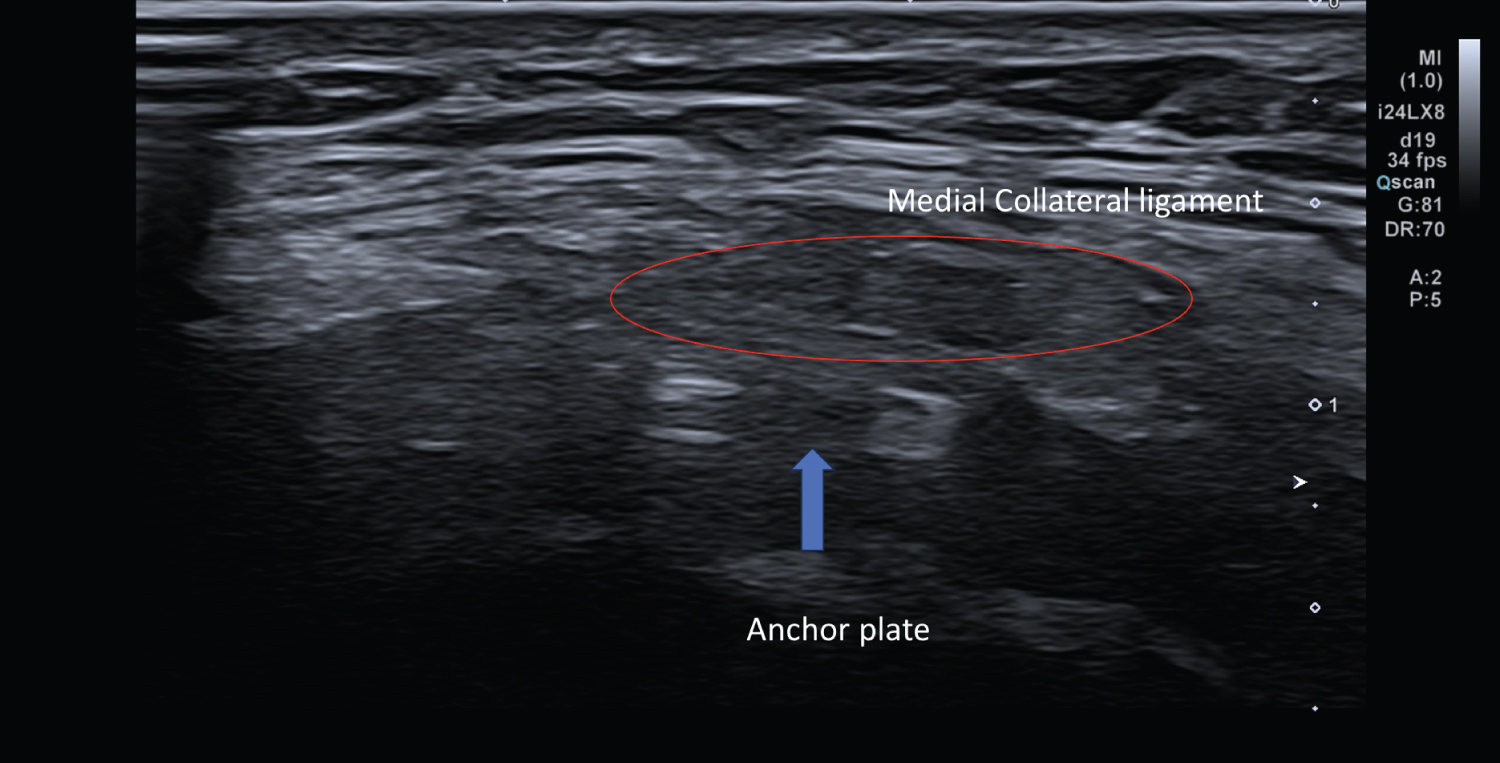 Figure 5: Axial view of the knee using echography showing the medial collateral ligament that appeared thickened and hypoechogenic with a loss of the fibrillar aspect on contact with the anchor plate.
View Figure 5
Figure 5: Axial view of the knee using echography showing the medial collateral ligament that appeared thickened and hypoechogenic with a loss of the fibrillar aspect on contact with the anchor plate.
View Figure 5
A surgical intervention carried out arthroscopically allowed to objectify this impingement and remove the material in a day surgery. The medial meniscus had a lesion in the middle horn, and the anchor plate was entrapped deep into the medial collateral ligament (Figure 6 and Figure 7). The patient noticed an immediate post-operative improvement in his pain level and remained pain-free with appropriate functional outcomes during the follow-up visits. The patient has provided the treating team with written consent and permission to discuss and publish his case for educational purposes.
 Figure 6: Intra-operative arthroscopic imaging showing the medial meniscus with a lesion in the middle horn, and the anchor plate entrapped deep into the medial collateral ligament.
View Figure 6
Figure 6: Intra-operative arthroscopic imaging showing the medial meniscus with a lesion in the middle horn, and the anchor plate entrapped deep into the medial collateral ligament.
View Figure 6
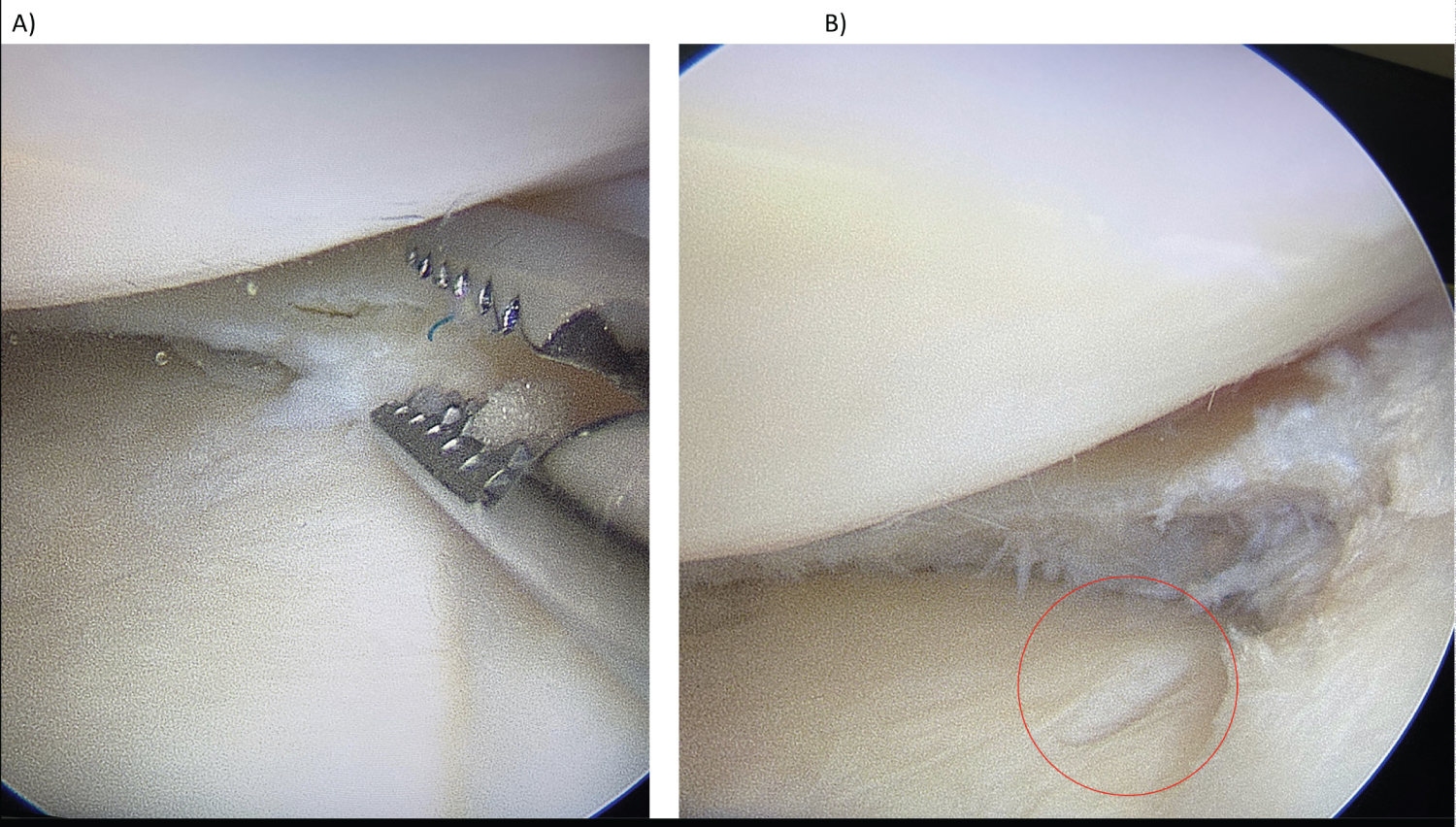 Figure 7: Intra-operative arthroscopic imaging. A) Demonstrating final steps of attraping the anchor plate and removing it from the deep fibers of medial collateral ligament; B) Final view of the knee joint with chondral lesion to the tibial plateau resulted from the anchor plate contact (circled).
View Figure 7
Figure 7: Intra-operative arthroscopic imaging. A) Demonstrating final steps of attraping the anchor plate and removing it from the deep fibers of medial collateral ligament; B) Final view of the knee joint with chondral lesion to the tibial plateau resulted from the anchor plate contact (circled).
View Figure 7
Over the years, there has been a significant increase in the number of meniscal repair surgeries that have been directly linked to the development of the all-inside technique [4]. Nowadays, many surgeons prefer all-inside repair because of its ease of use, low risk of soft tissue damage, and faster learning curves [7,11]. FasT-Fix implants have proven to be biomechanically advantageous over other all-inside systems [6]. However, the use of these implants can still be associated with common complications, mainly intraoperatively related to inappropriate implant use and technical errors leading to mispositioning, failure to deploy, and anchor slippage during suture tightening [12]. Among post-operative complications, persistent joint pain and swelling, functional limitation, and diffuse synovitis have been previously described [13].
This case report describes a rare late post-operative complication with the use of the FasT-Fix system of Smith and Nephew Inc. in meniscal repair, in which the anchor plate disengaged and impinged on the deep fibers of the medial collateral ligament causing abrupt disabling anteromedial pain associated with a decreased range of motion of the knee joint. To our knowledge, no other reports in the literature have described this complication. Rauck, et al. [14] reported two similar cases in which both patients underwent meniscal repair using FasT-Fix implants, and the anchors were pulled out from the posterior horn and lodged by the anterior horn of the menisci approximately nine months after the primary intervention [14]. In the first case, the patient had a peripheral tear in the posterior horn of the medial meniscus repaired in a vertical mattress fashion via three FasT-Fix implants. In the second case, the patient had medial and lateral posterior meniscal capsular junction lesions repaired by an anchor in a horizontal mattress fashion in the medial compartment, and with two anchors in a vertical mattress fashion to reduce the tear on the lateral meniscus. Both reported cases underwent concomitant anterior cruciate ligament (ACL) reconstruction (hamstring technic). Patients with this type of rare complication usually present in the late-post-operative phase complaining of sudden localized pain and a clicking sensation and were able to pinpoint the area where the anchors were settled. In all described cases, MRI was not conclusive in excluding failure of the suture material, where the arthroscanner was able to differentiate between implant failure and re-lesion. However, we were neither able to diagnose the cause of the symptoms nor determine the anchor location using both MRI and arthroscanners. This might be related to the size of the anchor, atypical position of the anchor, or unusual clinical presentation. In contrast, echography of the knee was sufficient to identify the impinged anchor on the medial collateral ligament.
The biomechanical properties of FasT-fix anchors have been well described in the literature, and studies have shown a high load to failure and stiffness at the repair site of these anchors regardless of suture application fashion [15-17]. We emphasize the accurate positioning of the implants and the use of an accompanying depth limiter and depth probe to control the desired depth limit, as this may affect the stabilization of the anchor. We aimed to provide awareness of this rare complication to allow for early diagnosis and appropriate management. During meniscal repair, it is important to evaluate all techniques to obtain the strongest, most durable suture. Inside-out or outside-in repair techniques should also be considered, depending on the area of injury. These may have the advantage of simply using thread.
Meniscal repair is currently preferred to meniscectomy, especially in young, active, and otherwise healthy patients, owing to the decreased risk of knee osteoarthritis [18]. All-inside meniscal repair is simple and often sufficient for meniscal healing. Nevertheless, they can be a source of specific complications that need to be highlighted and be aware of in order to avoid revisions for unjustified meniscectomies.
Patients who experience sudden onset pain and functional disability should be aware of implant disengagement and impingement with the surrounding soft tissue. Echography of the knee should be considered during clinical presentation for better identification and proper management.