This report details our experience and technique for addressing massive uncontained defects of the glenoid during revision in reverse total shoulder arthroplasty. The glenoid reconstruction was performed in a two-stage approach, with the initial stage involving the removal of all implants and the grafting of allogenic femoral head bone into the glenoid defect. Following confirmation of bone block consolidation on a CT-scan, the second stage entailed the implantation of the glenoid base over the bony block. Our results show no cases of loosening, implant failures, dislocations, periprosthetic fractures, or infections in any of the patients. This technique is considered reproducible and relies on readily available and familiar materials.
Level of evidence: Level IV, Case Series, Treatment Study
Allograft, Bone loss, Glenoid defect, Reverse shoulder arthroplasty
Treatment of glenoid bone loss in shoulder arthroplasty is challenging because of the increased risk of malposition of the glenoid component, increased rate of component loosening, and possible resorption of the bone graft [1-3]. The semi-constrained nature of reverse shoulder arthroplasty poses increased stresses on glenoid, which may lead to its glenoid component loosening and eventually failure [4-8]. Small glenoid bony defects may be filled with cancellous chips or tricortical iliac crest bone graft (TICBG), but larger uncontained defects need more substantial substance to support a baseplate implant [9]. Hence, providing a stable glenoid with sufficient bone stock in which to implant a glenoid base plate poses a difficult problem during reconstruction of uncontained glenoid bone loss [3,10]. Several techniques have been described in the literature to reconstruct severe bone loss of the glenoid, including staged revisions as well as the use of auto grafts and allografts. However, all these techniques have their inherent drawbacks, yet no ideal approach has been identified so far. The aim of this article is to present our experience in dealing with massive uncontained glenoid bone loss through a 2-stage technique for glenoid reconstruction using Femoral head allograft.
Between 2020 and 2022, 4 revision surgeries with severe glenoid bone loss have been addressed at our institute through a two-stage operation with glenoid reconstruction using femoral head allograft. The procedure was reproduced under general anaesthesia with an interscalene block in a semi beach chair position. A deltopectoral approach was performed in all shoulders. After the subscapularis release, complete metal removal was performed, and the glenoid was initially reamed slightly to provide a smoother concentric surface for the graft. Small holes were drilled in the glenoid surface to facilitate blood flow and potentially enhance incorporation of the graft. After the femoral head allograft was contoured with a high-speed burr to the desired shape and size, the graft was implanted into the glenoid and typically secured within the defect using three to five (3.5 mm) cannulated screws. To maintain the length of the humeral bone, as well as to protect the bone graft, a cement spacer shaped like the humeral head was inserted into the humerus. 2-4 months after the initial operation, CT scan was conducted to assess the bone union between the allograft and the glenoid. Once bone consolidation was confirmed, the second operation was performed to implant the reverse prosthesis: After removing the cannulated screws from the implanted graft, a 25-mm peg was used for the glenoid baseplate implantation. This was done to ensure that the baseplate extends into the native glenoid by at least 10 mm, ensuring both immediate secure fixation and early in growth. After removal of the spacer, the humeral stem was then implanted in a standard fashion (Figure 1 and Figure 2). A shoulder brace was used for 6 weeks post-op, at 3 weeks postoperatively, a rehabilitation program was started; rehabilitation comprised passive ROM exercise for 2 weeks, and then active assistive and active exercises.
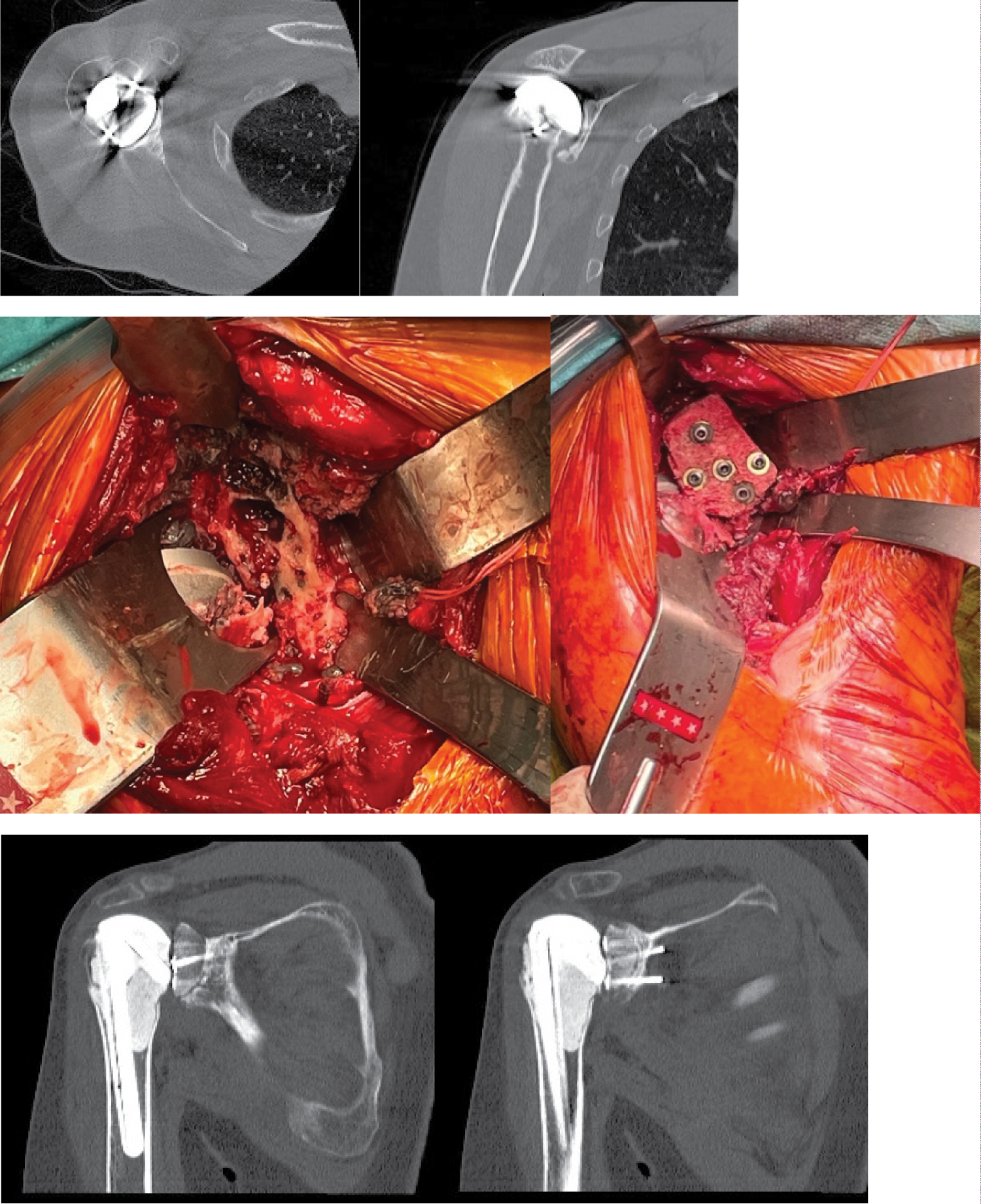 Figure 1: This is a case involving a 57-year-old female patient who presented with severe and progressive shoulder pain, along with evidence of severe loosening of the hemiarthroplasty. After the removal of the prosthesis, the femoral head allograft was prepared using a saw to closely match the anatomy and securely attach it as the new glenoid with the use of 5 cannulated screws. After a span of 4 months, a CT scan revealed the successful consolidation of the bone block with the glenoid. At this point, the second stage of the procedure was performed, which included the removal of the screws and the implantation of the reverse total shoulder arthroplasty.
View Figure 1
Figure 1: This is a case involving a 57-year-old female patient who presented with severe and progressive shoulder pain, along with evidence of severe loosening of the hemiarthroplasty. After the removal of the prosthesis, the femoral head allograft was prepared using a saw to closely match the anatomy and securely attach it as the new glenoid with the use of 5 cannulated screws. After a span of 4 months, a CT scan revealed the successful consolidation of the bone block with the glenoid. At this point, the second stage of the procedure was performed, which included the removal of the screws and the implantation of the reverse total shoulder arthroplasty.
View Figure 1
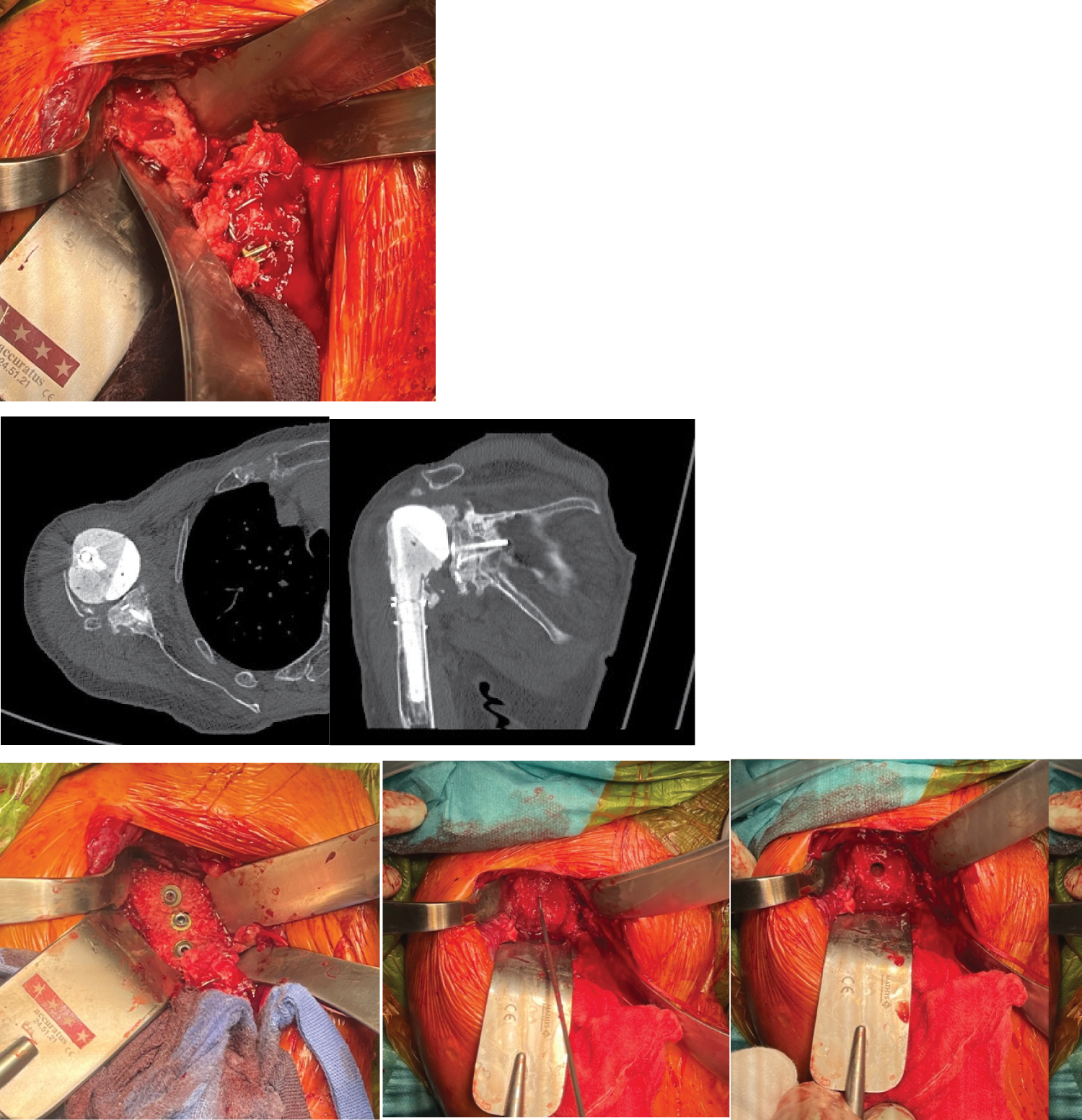 Figure 2: This is a case of a 76-year-old female patient who presented with significant loosening of a reverse prosthesis and a severe glenoid defect. After the complete removal of the prosthesis, the femur head allograft was sized and securely placed within the glenoid defect using cannulated screws. Three months later, a CT scan confirmed the successful consolidation of the bone block with the glenoid. Subsequently, the second stage of the procedure was performed, which involved the removal of the screws and the implantation of the reverse total shoulder arthroplasty.
View Figure 2
Figure 2: This is a case of a 76-year-old female patient who presented with significant loosening of a reverse prosthesis and a severe glenoid defect. After the complete removal of the prosthesis, the femur head allograft was sized and securely placed within the glenoid defect using cannulated screws. Three months later, a CT scan confirmed the successful consolidation of the bone block with the glenoid. Subsequently, the second stage of the procedure was performed, which involved the removal of the screws and the implantation of the reverse total shoulder arthroplasty.
View Figure 2
Revision shoulder arthroplasty often necessitates the management of glenoid bone defects, with up to 38% of patients undergoing reverse shoulder arthroplasty (RSA) requiring interventions to address significant glenoid bone loss [2,11]. A range of approaches have been used to address glenoid wear include hemiarthroplasty, eccentric reaming, reinforced implants, custom-made reverse shoulder arthroplasty, pyrocarbon interposition shoulder arthroplasty, and the use of autografts derived from the humeral head or iliac crest [1,3,9,12,13]. In cases involving more significant bone defects, allografts sourced from the femoral head have also been utilized [1,3,14]. Additionally, a combination of allograft with cancellous autograft has been considered as an alternative approach to address severe glenoid bone loss [9,10]. Nevertheless, the optimal choice of graft for glenoid deformity reconstruction in arthroplasty remains controversy [5,14-16].
Wagner, et al. [14] found that shoulders receiving bone grafts during revision surgeries experienced higher rates of glenoid component loosening, implant failure, and lower two and five-year survival rates compared to those without bone grafts. However, despite these challenges, the procedure provided pain relief, improved shoulder function, and stability, which led to its continued recommendation [14].
Gupta, et al. [2] concluded that addressing severe glenoid bone loss can be accomplished effectively with a one-stage bone allograft procedure combined with RSA. However, a two-stage approach is also advised when encountering difficulties in achieving primary baseplate stability or when there are concerns about intraoperative glenoid stability [2].
In our clinical practice, we prefer employing femoral head allografts in a two-stage procedure due to several advantages. First, the generous size of the femoral head allograft allows for easy customization to match the natural architecture of the glenoid. Second, the two-stage procedure ensures adequate consolidation of the bone graft, contributing to long-term baseplate stability. While no implant failures were observed in our study, it's essential to acknowledge the limited number of cases and the short follow-up period.
The use of femoral allografts, however, comes with certain drawbacks, including technical complexities, fixation challenges, and the potential for graft resorption leading to component loosening. Furthermore, there are logistical issues such as the need for advanced graft ordering, limited availability in every operating room, and associated expenses, which may not be practical in all clinical settings, particularly as the demand for revision arthroplasty continues to grow [3].
This case study demonstrates the effectiveness of a two-stage procedure involving allogenic bone grafting as a viable solution for addressing baseplate loosening and glenoid bone defects following reverse shoulder arthroplasty (RSA), leading to favourable functional outcomes.