Bilateral traumatic dislocation of the hip joint is very rare but not new; Marquardt in 1936 reported the first case; only 51 cases have been reported so far. We report a case of bilateral dislocation divergent hip with 6 months follow-up period.
Traumatic bilateral hip dislocation is very rare; 56 cases have been reported in the literature so far, the first in 1936 by Marquardt. We report a case of bilateral divergent dislocation of the hip with 6 months of follow-up.
Dislocation, Cephalic necrosis, Hip, Bilateral divergent
Traumatic hip dislocations represent 2 to 5% of all dislocations [1]. Bilateral forms are very rare. Their mechanism remains rather particular. Reduction must be urgent to minimize the risk of head necrosis. Our observation illustrates this unusual lesion.
This is a 78-year-old man with Parkinson's who was admitted to the emergency room after a domestic accident: a fall from his height on his back while the patient was squatting. On examination in the emergency room, the left hip was in adduction-internal rotation, and the right hip in adduction-external rotation. Neurovascular examination was unremarkable, including no sciatic paralysis.
The radiographic assessment objectified a posterior dislocation of the left hip, and anterior on the right side, with no visible acetabular or femoral fracture (Figure 1). A CT scan of the pelvis was requested urgently which objectified a posterior dislocation of the left hip, and anterior on the right, without acetabular or femoral fracture, nor visible intra-articular foreign body (Figure 2), So it is a divergent bilateral dislocation of the two hips.
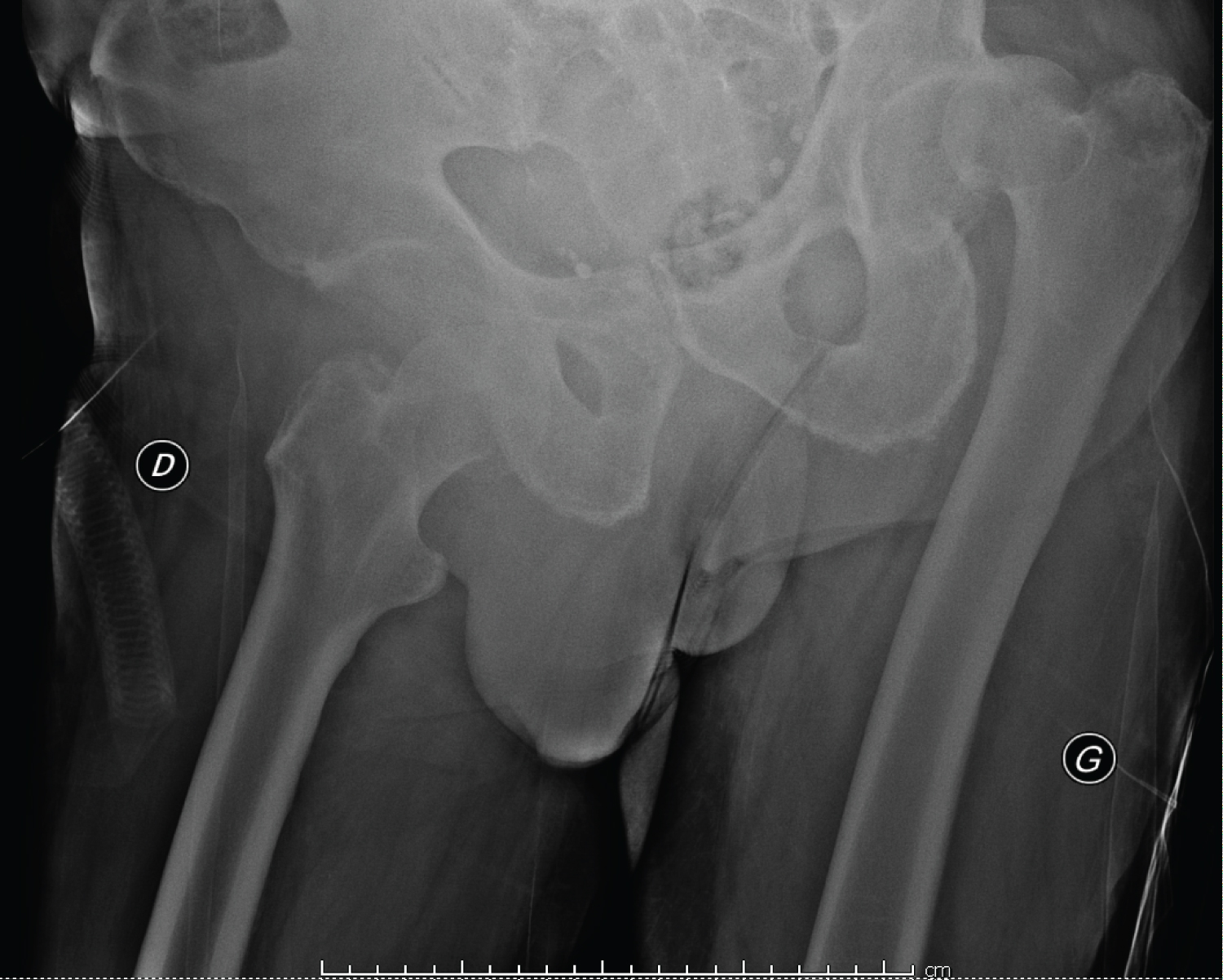 Figure 1: Radiological appearance of bilateral hip dislocation.
View Figure 1
Figure 1: Radiological appearance of bilateral hip dislocation.
View Figure 1
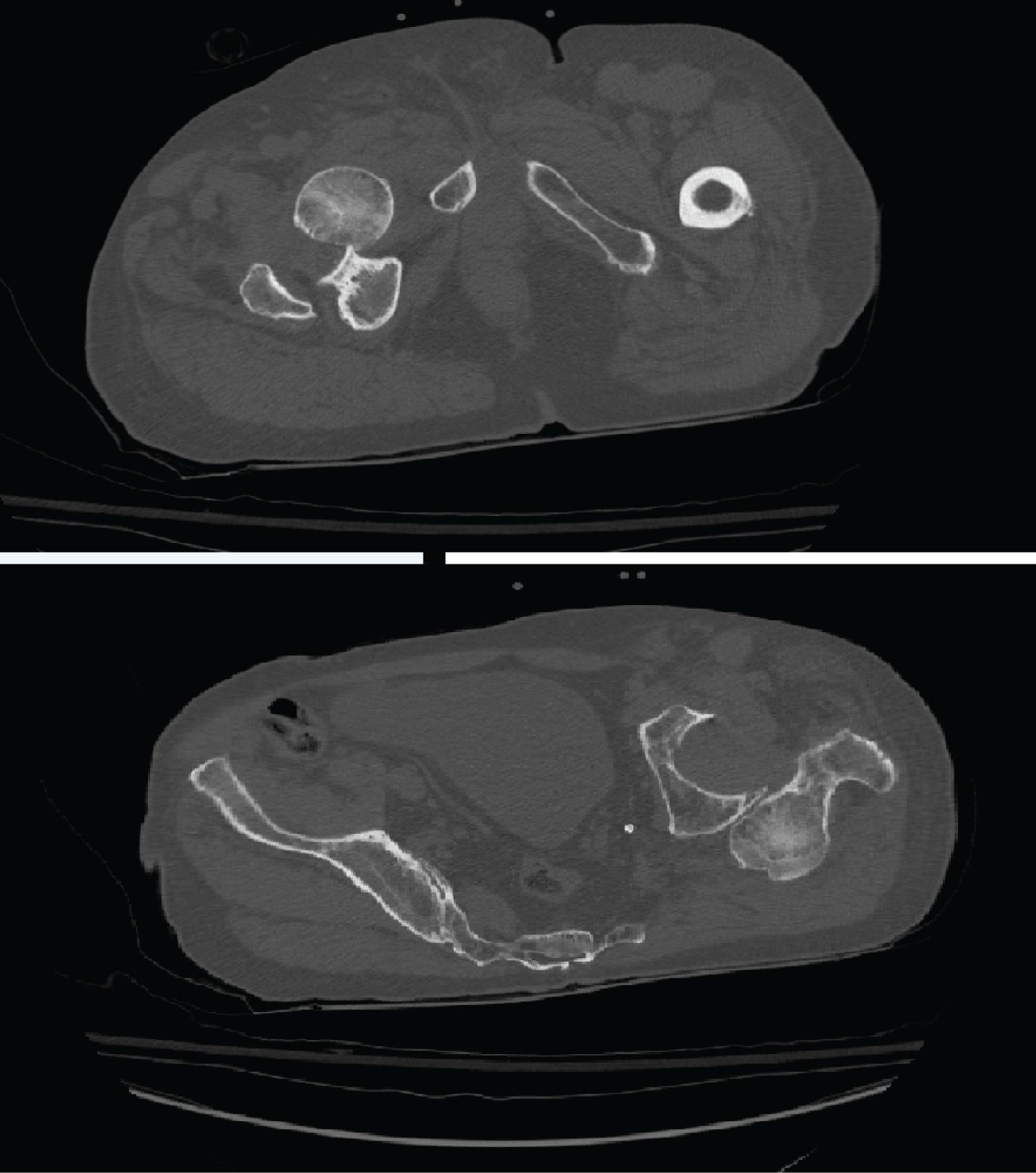 Figure 2: CT appearance of bilateral divergent dislocation of the hip (posterior dislocation of the left hip, and anterior on the right).
View Figure 2
Figure 2: CT appearance of bilateral divergent dislocation of the hip (posterior dislocation of the left hip, and anterior on the right).
View Figure 2
Reduction by external maneuver of the two dislocations was performed under sedation. Radiographic control confirmed the reduction (Figure 3). Immobilization with a Zimmer splint on both sides was applied for 3 weeks. Followed by gradual weight-bearing for another six weeks. 6 months after the accident, both hips remained stable with no signs of head necrosis (Figure 4).
 Figure 3: Control X-ray after reduction under general anesthesia.
View Figure 3
Figure 3: Control X-ray after reduction under general anesthesia.
View Figure 3
 Figure 4: Control X-ray after 6 months follow-up.
View Figure 4
Figure 4: Control X-ray after 6 months follow-up.
View Figure 4
Bilateral hip dislocations are relatively common in congenital varieties. This bilaterality is rarely encountered in a normal adult pelvis. Public road accidents are most often involved, rarely sports accidents. The mechanism is frequently indirect, producing the classic dashboard syndrome; the indirect mechanism, as in our case, is very rare.
The position of the limb at the time of impact will condition the type of dislocation. Posterior dislocations. Usually occurs on hips fixed in flexion-adduction-internal rotation. Concerning anterior dislocations, they are most often in extension, abduction and external rotation. Our patient reproduced the 2 types which is very rare [2,3], have also been described [1,3-6].
The reduction of the two dislocations is an absolute emergency. The six-hour period must not be exceeded [7]. Blood reduction may be necessary in case of associated surgical fracture of the acetabulum, in case of irreducibility, in neglected forms or when the sciatic nerve must be explored [3]. The risk of cephalic necrosis after these bloody reductions can reach 40% [8-10]. Maintenance of the reduction by a traction system with a relief is recommended, but its duration is highly debated. According to the teams, it varies from a few days to six weeks [1,4,6].