In spite of the large variety of different techniques available for their treatment, acetabular fractures still pose a formidable challenge to the orthopedic surgeon, with a close relationship having been observed between degree of reduction, radiological findings and clinical results. The purpose of this manuscript is to introduce a technical enhancement that can be resorted to following exposure of the acetabular dome when using a modified Stoppa approach to facilitate reduction of bone fragments, a potential bone grafting procedure and the restoration of joint congruity.
The Stoppa surgical access was first reported in 1989 for the treatment of inguinal hernia using a pre-peritoneal mesh [1]. The approach was subsequently modified by Hirvensalo, et al. [2] and later by Cole and Bolhofner [3], who turned it into an alternative to the traditional ilioinguinal approach proposed by Judet and Letournel [4-6] for treating the majority of acetabular fractures (anterior column, anterior wall, anterior column with a posterior hemitransverse component, T-shaped and some fractures involving both columns). The Stoppa approach consists of an intrapelvic extraperitoneal approach that allows direct visualization, reduction and fixation of the quadrilateral plate, thereby providing a degree of primary mechanical stability that can seldom be achieved with an ilioinguinal approach [7-12]. This paper describes a technical modification for cases of complex acetabular fractures exhibiting impaction or comminution of the acetabular dome, which can facilitate fracture reduction and subsequent fixation, as well as, if necessary, a potential bone grafting procedure.
With the hip in 30-45° of flexion and the surgeon sitting on the contralateral side of the lesion, an 8-10-centimeter-long horizontal incision is made two centimeters above the pubic symphysis. The linea alba is opened in a craniocaudal direction and the rectus femoris on the same side of the fracture is subperiosteally detached, exposing the pubic symphysis and the superior pubic ramus. Subsequently, the Retzius space can be accessed after reflecting the bladder to protect it from injury. From 4 to 9 cm lateral to the pubic symphysis, 50-84% of patients present with a so-called corona mortis [13-15], a vascular anastomosis between the obturator and the external iliac artery (Figure 1). This structure must be either ligated or electrocoagulated as it is a potentially dangerous source of bleeding.
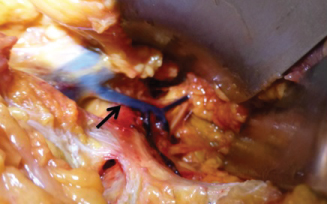 Figure 1: Cadaveric image: Corona Mortis (arrow). View Figure 1
Figure 1: Cadaveric image: Corona Mortis (arrow). View Figure 1
The iliopectineal fascia is subsequently detached at the level of the supero-lateral pubic ramus and Hohmann retractors are placed along the anterior column, at the level of the linea terminalis, from the anterior pubic ramus to the anterior sacroiliac joint. These retractors are aimed at protecting the external iliac vessels, the iliac psoas and the femoral nerve during the procedure. From that moment onwards, the fracture can be exposed in the mid-pelvic area (Figure 2). Lateral to the fracture, the obturator neurovascular bundle follows an oblique path, from superior-posterior to anterior-inferior, before it enters the obturator foramen. The bundle and the bladder must be protected by placing a blunt Hohmann retractor at the level of the greater sciatic notch. Placement of this retractor makes it possible to expose the posterior column up to the anterior sacroiliac joint, which will be the posterior fixation point of the osteosynthesis used. At that moment, full exposure of the fracture will have been achieved. As a technical enhancement, in cases where the dome has been impacted, the fractured quadrilateral plate can be further medialized with the help of a Cobb periosteal elevator. At the same time, lateral traction is applied to the proximal femur using a Schanz screw inserted in the lesser trochanter. This technical maneuver allows direct visualization of the impacted area. Disimpaction of the dome fracture is performed at the subchondral level, using a 10 mm scope or a Cobb periosteal elevator. Mobilization of the impacted dome creates a larger bone defect (Figure 3), which requires application of bone grafting to provide robust structural support to the dome area and prevent the dome from shifting back to the original position. We usually use cadaveric bone allograft. The fracture can now be reduced and stabilized by means of an infra-pectineal plate (Figure 4) (3.5 mm Low Profile Pelvic System, Synthes USA, Paoli, PA) supported directly on the quadrilateral plate. The fixation screws must be placed into the two posterior-most screw-holes, located in front of the anterior sacroiliac joint and into the two or three anterior screw-holes, located at iliac-publc level. In Figure 5 and Figure 6, we show a case of a patient with a transverse acetabular fracture before and after being operated by a modified Stoppa approach.
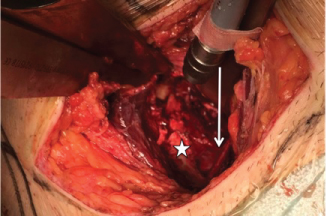 Figure 2: Intraoperative image: exposure of the quadrilateral plate (star) and obturator nerve (arrow). View Figure 2
Figure 2: Intraoperative image: exposure of the quadrilateral plate (star) and obturator nerve (arrow). View Figure 2
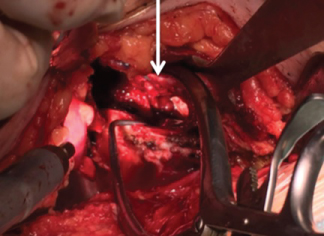 Figure 3: Intraoperative image: bone defect created with the mobilization of the impacted dome (arrow). View Figure 3
Figure 3: Intraoperative image: bone defect created with the mobilization of the impacted dome (arrow). View Figure 3
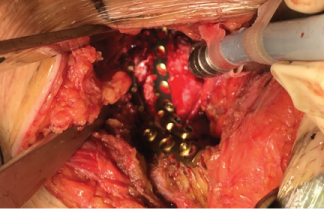 Figure 4: Reduction of the fracture and stabilisation using supra- and infra-pectineal osteosynthesis. View Figure 4
Figure 4: Reduction of the fracture and stabilisation using supra- and infra-pectineal osteosynthesis. View Figure 4
 Figure 5: Transverse acetabular fracture in a 24-years-old patient before surgery. View Figure 5
Figure 5: Transverse acetabular fracture in a 24-years-old patient before surgery. View Figure 5
 Figure 6: Radiographic control 2 years after the surgery using a modified Stoppa approach. View Figure 6
Figure 6: Radiographic control 2 years after the surgery using a modified Stoppa approach. View Figure 6
In spite of the development of many new surgical techniques to treat acetabular fractures, such fractures still pose a complex challenge to orthopedic surgeons given the complex anatomy of the acetabular area and the risk of potential complications. The mini-invasive intrapelvic extraperitoneal modified Stoppa approach allows direct visualization of the medial section of the anterior column, the quadrilateral plate and the medial area of the interior-most portion of the posterior column, [10,12] providing access to the sacroiliac joint, the sciatic spine and the greater and lesser sciatic notches, which allows direct reduction and fixation of most fractures. Earlier studies have shown that the modified Stoppa approach is particularly effective for fractures of the quadrilateral plate with medial displacement and dome impaction [7-12,16,17].
As shown by other authors, [18-20] there exists a close relationship between radiologic and clinical results. Presence of the gull sign, described by Anglen, et al., [21] is indicative of acetabular dome impaction and is often associated to a poor prognosis. Lafflame, et al. [22] correlated comminution of the dome with a less effective reduction and with progression to total hip arthroplasty. In their study, Kim, et al. [18] reported lower reduction rates, and hence poorer functional results, when 3-or-more-part fractures were present in the dome area (p = 0.03). For that reason, reconstruction of the acetabular weight bearing area is a prerequisite for satisfactory clinical results. A modified Stoppa approach used in combination with the technical variation proposed in this article could allow reduction of impacted dome fragments and restoration of joint congruity. Subchondral bone grafting can also be used to prevent re-impaction of the fragments, thereby minimizing the negative effects of the presence of dome comminution on clinical patient outcomes.