To evaluate of the effectiveness of rehabilitation in patients following mandibulectomy and free fibula flap reconstruction with further endosteal implants. The patient cohort consisted of 27 patients years (14 males and 13 females) with lower jaw defects due to resection for tumors, were reconstructed with fibula-free flaps in a 6-year period (2015-2020). All patients underwent a thorough clinical laboratory, radiological examination according to a generally accepted scheme. Patients were evaluated by preoperative and postoperative outcome using computed tomography scan evaluation. The surgical procedure included: Segmentar resection of the lower jaw, reconstruction with fibula free flap. The implants were evaluated with measures of Resonance Frequency Analysis (RFA) during the follow-up periods using Osstell Mentor at time of implant placement, after 3 months. The mean RFA recordings of all 134 implants were 65 ISQ at implant placement respectively 73 ISQ after 3 months. After 4-6 months of healing, 152 dental implants were placed in non-irradiated fibular bone. Dental prosthetic rehabilitation was performed after 3-4 months of submerged healing. Patients had received implant-bridge and hybrid denture that provided ideal facial balance and occlusion. Postoperative clinical and radiographic controls were made regularly, the criteria for implant success were assessed.With dynamic observation, clinical and radiological indices were stable, of the 152 implants installed, 2 failed to osseointegrate and 5 after years of loading (peri-implantitis). Success rate of implants 5 years after was 96.1%.
The reconstruction of the lower jaw defects after ablation of tumors with fibular flaps is a reliable method with good long-term results. In all 27 patients, fibula flaps provided adequate bone stock for implant placement. Implants placed in the reconstructed areas were demonstrated to integrate normally. The results showed that implant treatment is effective to improve patients’ masticatory efficiency and an acceptable quality of life to the patient.
Free fibula flap, Reconstruction of the lower jaw, Endosteal implants, Prosthetic rehabilitation, Bone metabolism markers
The mandibular resection resulting from treatment of malignant tumors, aggressive odontogenic tumors, or trauma can cause extensive composite defects including bone, oral lining mucosa, muscles, and teeth, with a significant decrease in the patient quality of life. After removal of the tumors the segmental bone defects initially cause a disruption of the muscular attachments, impair mastication and speech, and can lead to inadequate lip closure [1]. There are various methods available for reconstruction of mandibular defects: Non-vascularized bone grafts, titanium reconstructive splints or microsurgical techniques that allow the use of vascularized bone.
Every reconstructive technique must satisfy the following key objectives: 1) Obliteration of the defect; 2) Restoration of function; particularly speech and mastication; 3) Structural support for reconstruction of external facial features; and 4) Aesthetic reconstruction of these external facial features [2]. The goals of mandibular reconstruction are to re-establish the form of the lower third of the face and to restore the patient’s ability to eat in public, be intelligible to both trained and untrained listeners, and to maintain an unencumbered airway that allows the freedom to perform all activities [3]. Loss of mucosa from the floor of mouth is critical in the assessment of whether to restore this component of the defect with non-native tissue.
In cases of lesions of the lower jaw, segmental resection and reconstruction of the defect using a free flap of the fibula is a solution to restore the functions and aesthetics of the face resulting in a poor quality of life [4-6].
In 1989, Hidalgo became the first to report the transfer of fibular bone to reconstruct a segmental defect of the mandible [7].
Fibula is the most common donor site in both the vascularized and non-vascularized groups. Simple anatomy and accessibility of the fibula caused the popularity of this transplant in reconstructions of the lower jaw. The bone is available with enough length to reconstruct any mandible defect. A 22 to 25 centimeters segment of fibula bone may be harvested in the adult patient, permitting reconstruction of near-total mandibular defects with a single flap. During harvest, distally at least 5 cm of fibula should be left to prevent angle instability. It characteristics such as the thick and long cortical bony component (average width is 2.5 cm 3 cm, thickness approximately1.5 cm) provide a good rigidity to withstand physiological stress during mastication. The peroneal artery and vein are usually of good quality and caliber and ideal for microsurgical anastomosis. Post ablative lower jaw defects with neoplasm resection can be performed in a single stage. It is considered the gold standard for the reconstruction of these types defect [8-10]. While surgical restoration of lower jaw has advanced dramatically with free-flap techniques, restoration of oral function requires advanced approaches. Restoration of oral functions requires not only reconstruction of the mandibular defect, but also dental rehabilitation [11-13].
In the field of fibula graft, dental implants have been widely used in recent decades [14-16]. Among the researchers, there is an unequivocal opinion about the timing of implantation. Some authors prefer the simultaneous installation of implants in the autograft, noting that the implants did not have a negative on the autotransplant remodeling process [17,18].
In the case of a two-stage method, implants are placed 4-6 months after the autograft. According to many authors, the two-stage method is more predictable and reliable, because during this period, the regenerate occurs in the area of the autograft, which has good blood circulation, the autograft matures, converges in the recipient's area [19-23].
In the case of a larger defect, there is a risk of resorption due to the autograft to the implant or after orthopedic constructions [24].
Аfter transplantation of a vascularized fibular graft, the use of dental implants to restore chewing function is one of the solutions to this problem [25,26].
Objectives to evaluate of the effectiveness of rehabilitation in patients following mandibulectomy and free fibula flap reconstruction with further endosteal implants.
The patient cohort consisted of 27 patients years (14 males and 13 females) 26 and 63 presenting with lower jaw defects due to resection for tumors, were reconstructed with fibula-free flaps in a 6-year period (2015-2020).
The study was reviewed and approved by the Ethics Committee of the of the Yerevan State Medical University after M. Heratsi (protocol N12, 05.9.17) and in accordance with those of the World Medical Association and the Helsinki Declaration’, this sentence could be a first sentence of the material-methods sections.
Clinical data included demographic and clinical variables: Gender; age; neoplasm type; location of the lower jaw defect (Table1, Table 2 and Figure 1).
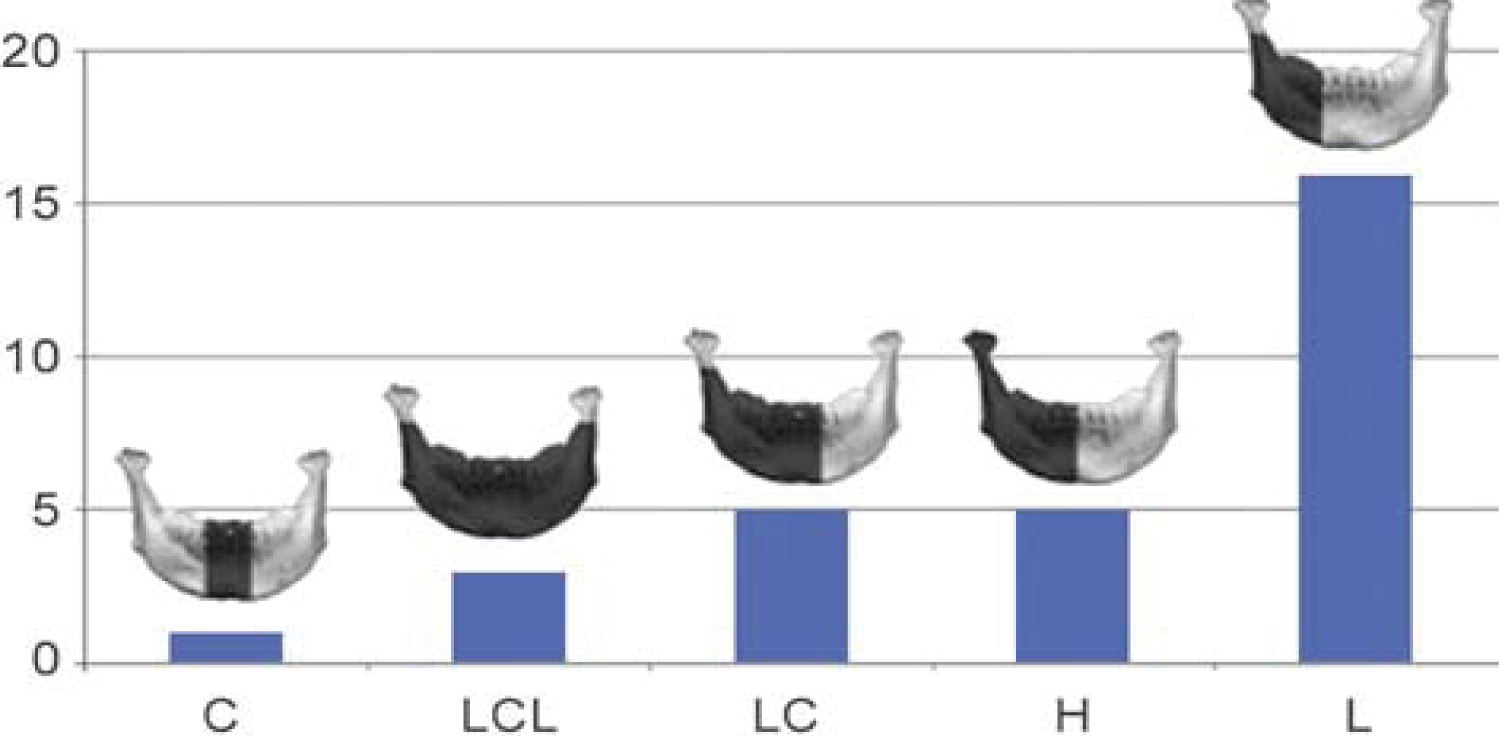 Figure 1: Lower jaw defects according to DD Jewer's classification model.
View Figure 1
Figure 1: Lower jaw defects according to DD Jewer's classification model.
View Figure 1
Table 1: Patients gender, age, neoplasm type, reconstructed with fibula-free flaps. View Table 1
Table 2: Distribution of patients according to the location of the lower jaw defect. View Table 2
The Jewer DD և co-authorship classification model was used in the treatment of lower jaw bone defects [27].
Lower jaw defects according to Jewer DD 1) Central defect C = central defect; 2) Bilateral defect LCL = bilateral defect; 3) Central և lateral defect LC = central and lateral defect; 4) Hemimandibulectomy H = hemimandibulectomy and 5) Lateral defect L = lateral defect (Figure 1).
Patients with jaw lesions had different locations, the size of the lesion ranged from 2 cm to 23 cm (Table 3).
Table 3: Free fibula used according to the length of the defect. View Table 3
To assess the degree of osseointegration and determine the timing of the functional load of dental implants installed in free vascularized bone autografts, a Resonance-Frequency Analysis (RFA) of the stability of implants using Osstell Mentor (Osstell instrument, Integration Diagnostics AB, Gothenburg, Sweden) at time of implant placement, after 3 months. All patients presented functional and esthetic complaints. All patients underwent a thorough clinical laboratory, radiological examination according to a generally accepted scheme. Patients were evaluated by preoperative and postoperative outcome using computed tomography scan evaluation using CT Galileos (Sirona, German) (Figure 2, Figure 3, Figure 4, Figure 5 and Figure 6). Biopsy of the lesion was obtained in all cases. The choice of surgical treatment is determined by the type of lesions and the sizes of jaw defect.
 Figure 2: (Patients 1) Preoperative CT scan showing Low differential osteosarcoma (stage T4N0 M0).
View Figure 2
Figure 2: (Patients 1) Preoperative CT scan showing Low differential osteosarcoma (stage T4N0 M0).
View Figure 2
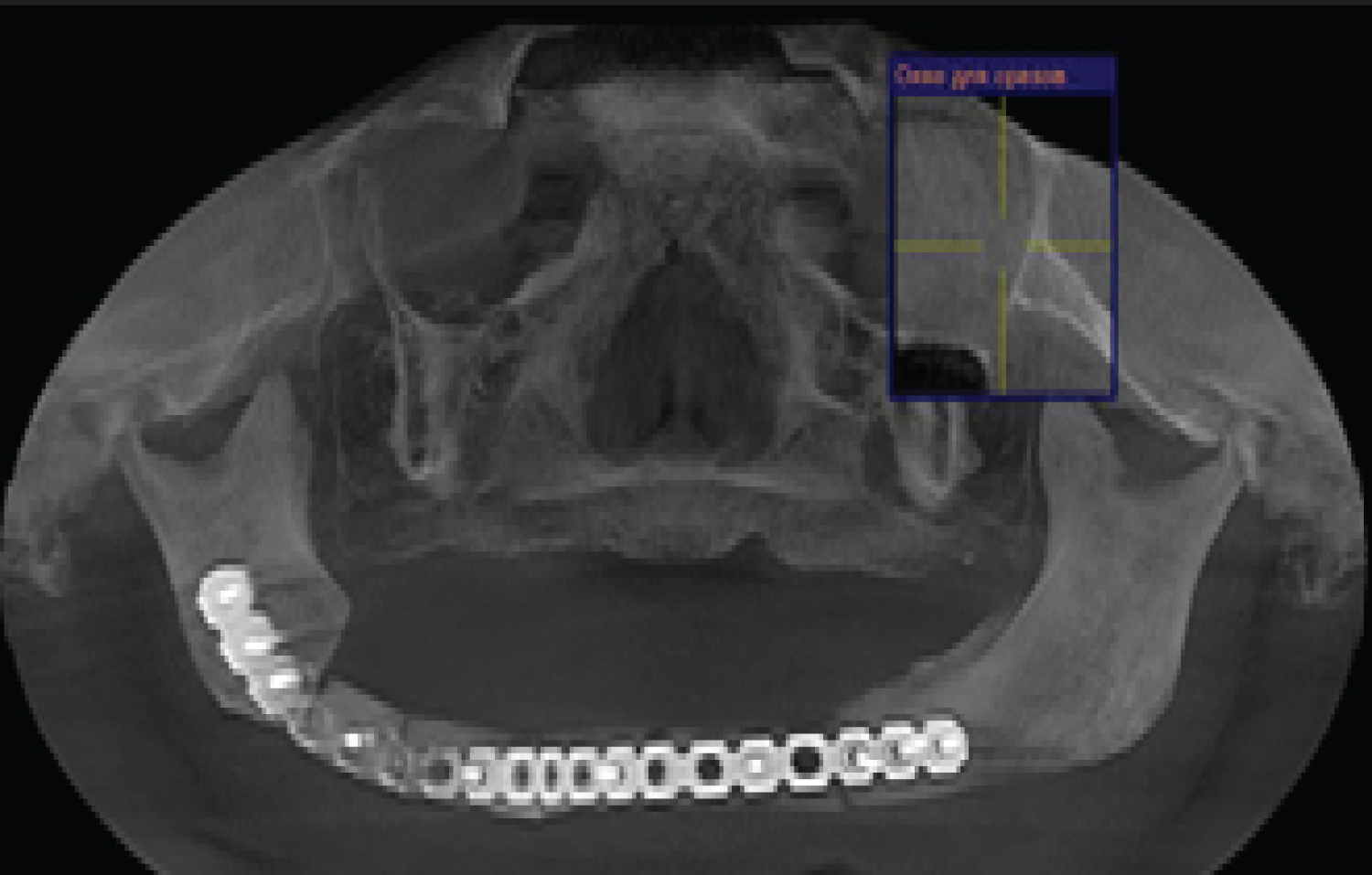 Figure 3: (Patients 1) CT scan after fibula transplant surgery.
View Figure 3
Figure 3: (Patients 1) CT scan after fibula transplant surgery.
View Figure 3
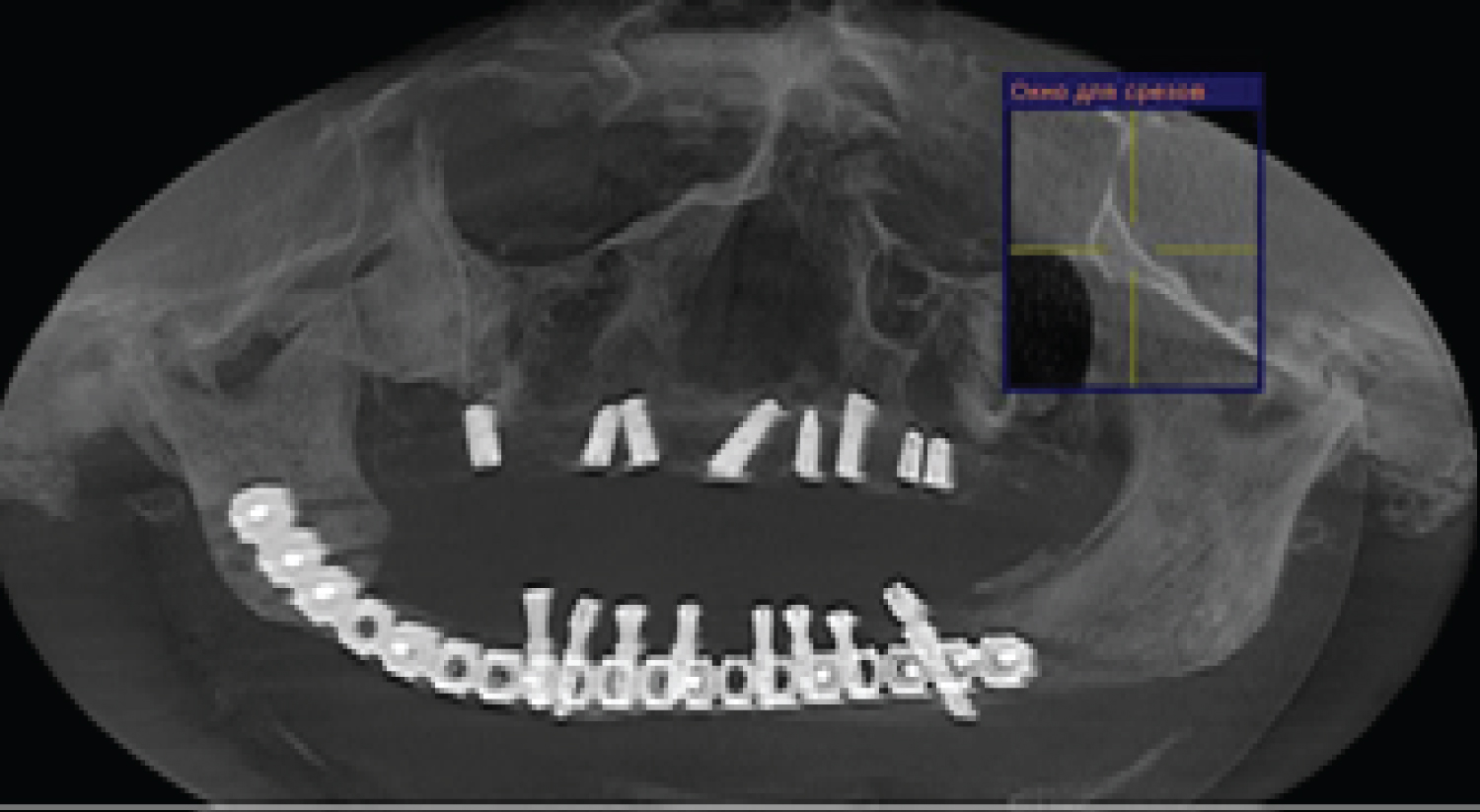 Figure 4: (Patients 1) CT scan showed well integrated dental implants in fibula transplant before prosthetic rehabilitation.
View Figure 4
Figure 4: (Patients 1) CT scan showed well integrated dental implants in fibula transplant before prosthetic rehabilitation.
View Figure 4
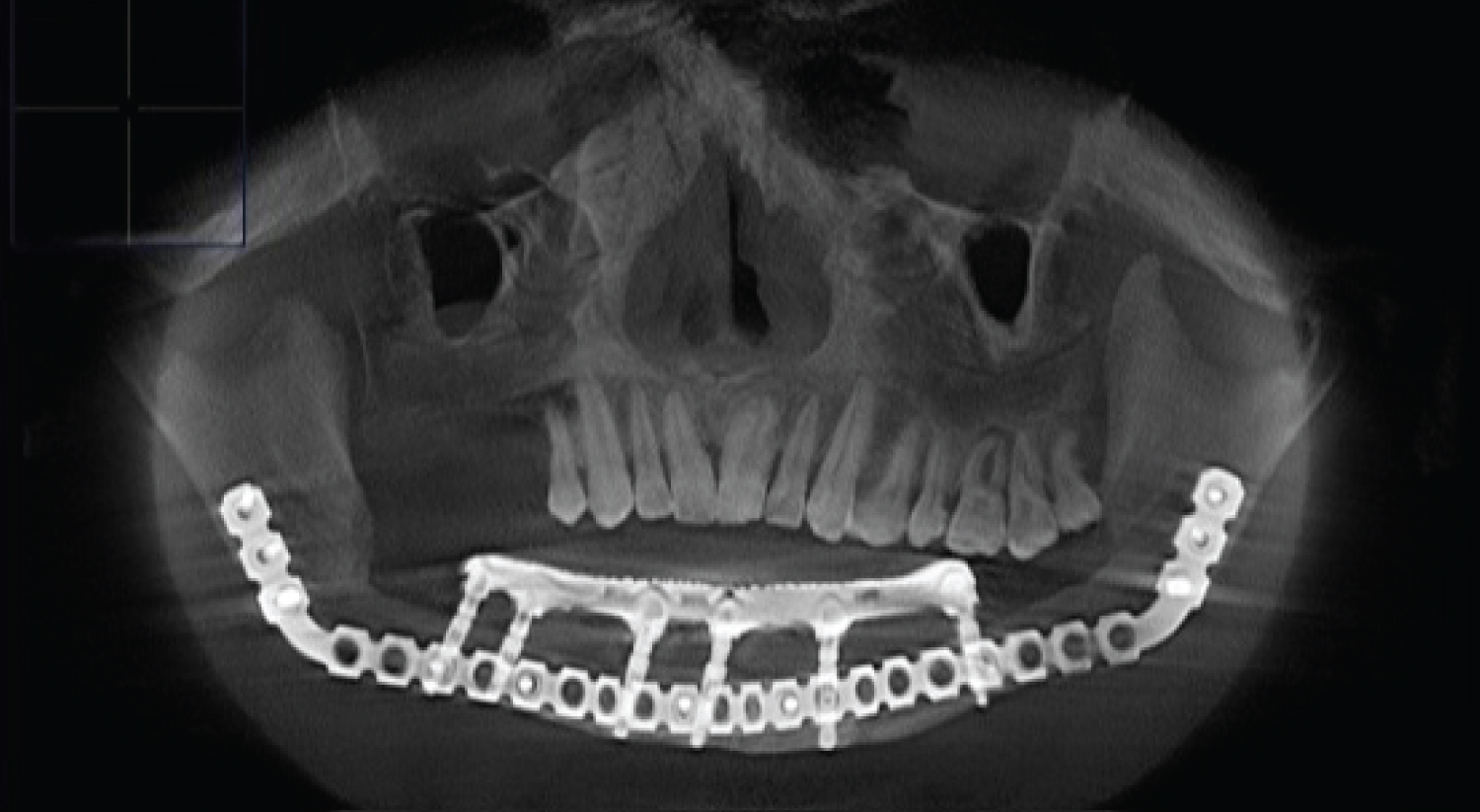 Figure 5: (patients 2) CT scan showed well integrated dental implants in fibula transplant after prosthetic rehabilitation.
View Figure 5
Figure 5: (patients 2) CT scan showed well integrated dental implants in fibula transplant after prosthetic rehabilitation.
View Figure 5
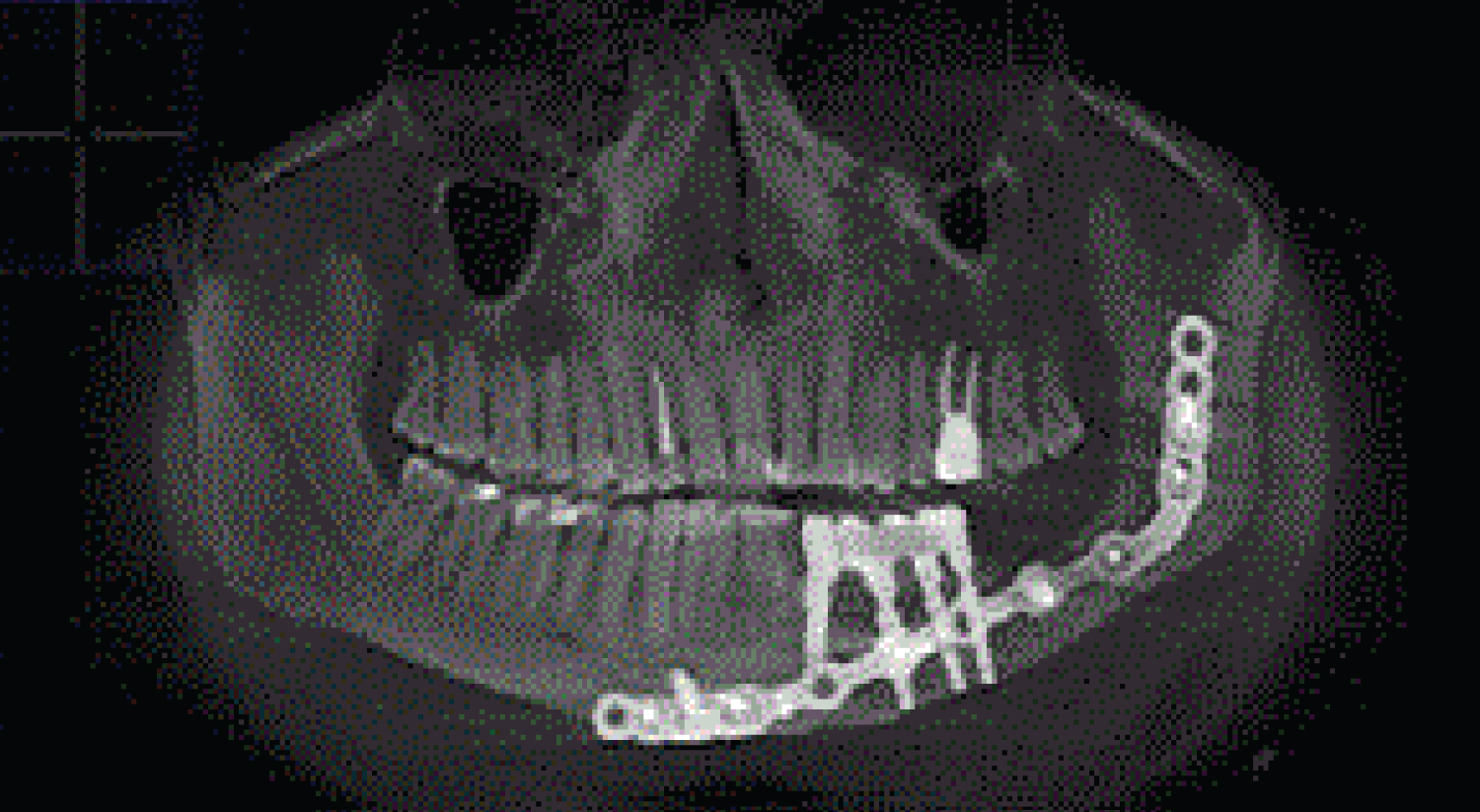 Figure 6: (Patients 3) CT scan showed well integrated dental implants in fibula transplant after prosthetic rehabilitation.
View Figure 6
Figure 6: (Patients 3) CT scan showed well integrated dental implants in fibula transplant after prosthetic rehabilitation.
View Figure 6
Two teams were involved in the surgery. The maxillofacial team resected the lesions of the lower jaw and further reconstruction with the fibular flap, the microsurgical team simultaneously harvested free vascularized flap of the fibula and performed an anastomosis of the arteries and veins of the fibula flap on the donor site. The surgical procedure included: Segmentar resection of the lower jaw, reconstruction with fibula free flap and implant installation 4-6 months after reconstruction (Figure 7, Figure 8, Figure 9 and Figure 10).
 Figure 7: (Patients 1) Design skin island contour at harvest site of fibula bone.
View Figure 7
Figure 7: (Patients 1) Design skin island contour at harvest site of fibula bone.
View Figure 7
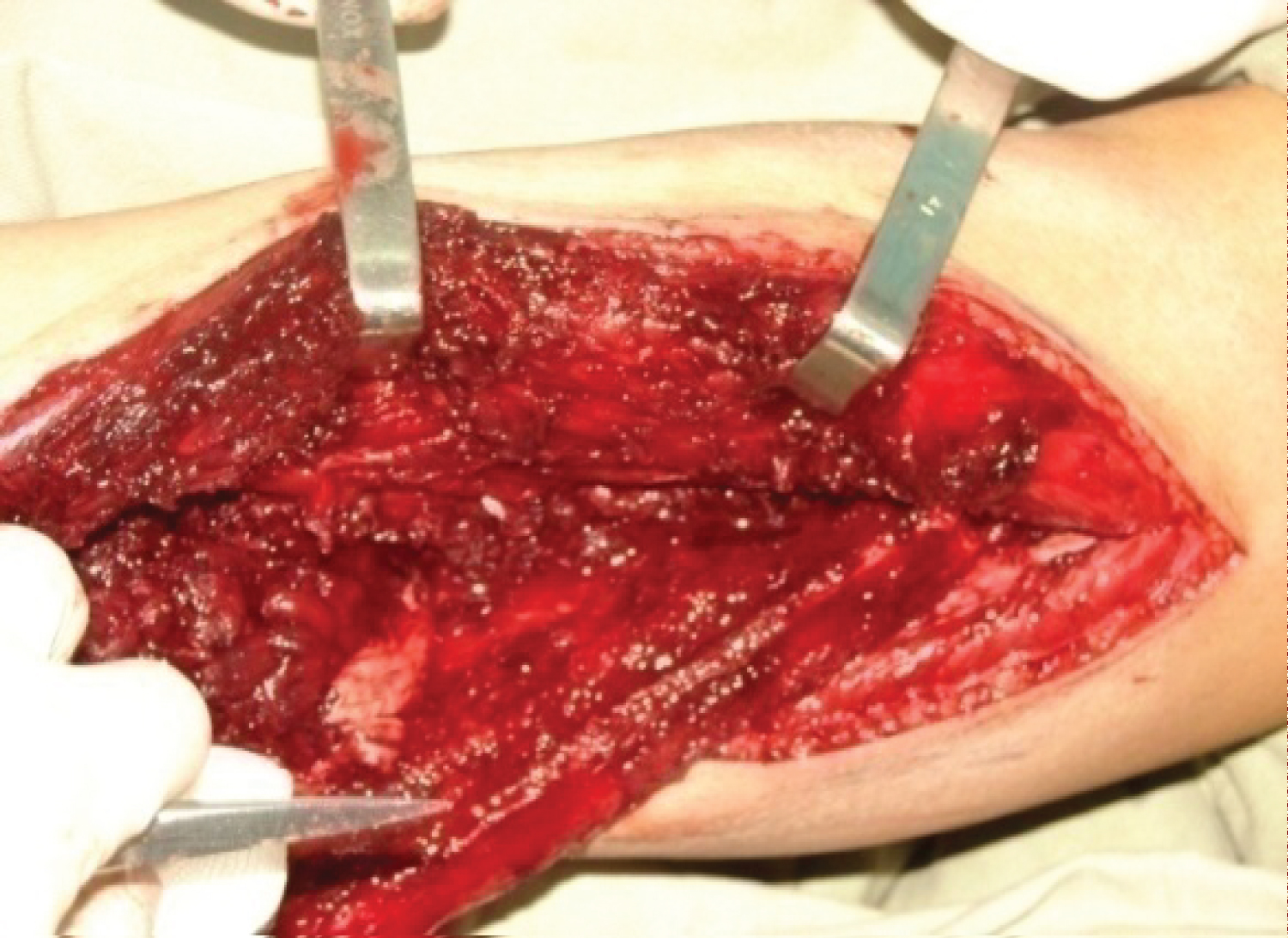 Figure 8: (Patients 1) Intraoperative photograph during harvesting the free fibula flap.
View Figure 8
Figure 8: (Patients 1) Intraoperative photograph during harvesting the free fibula flap.
View Figure 8
 Figure 9: (Patients 1) The contoured fibula graft fixation with the titanium reconstruction plate.
View Figure 9
Figure 9: (Patients 1) The contoured fibula graft fixation with the titanium reconstruction plate.
View Figure 9
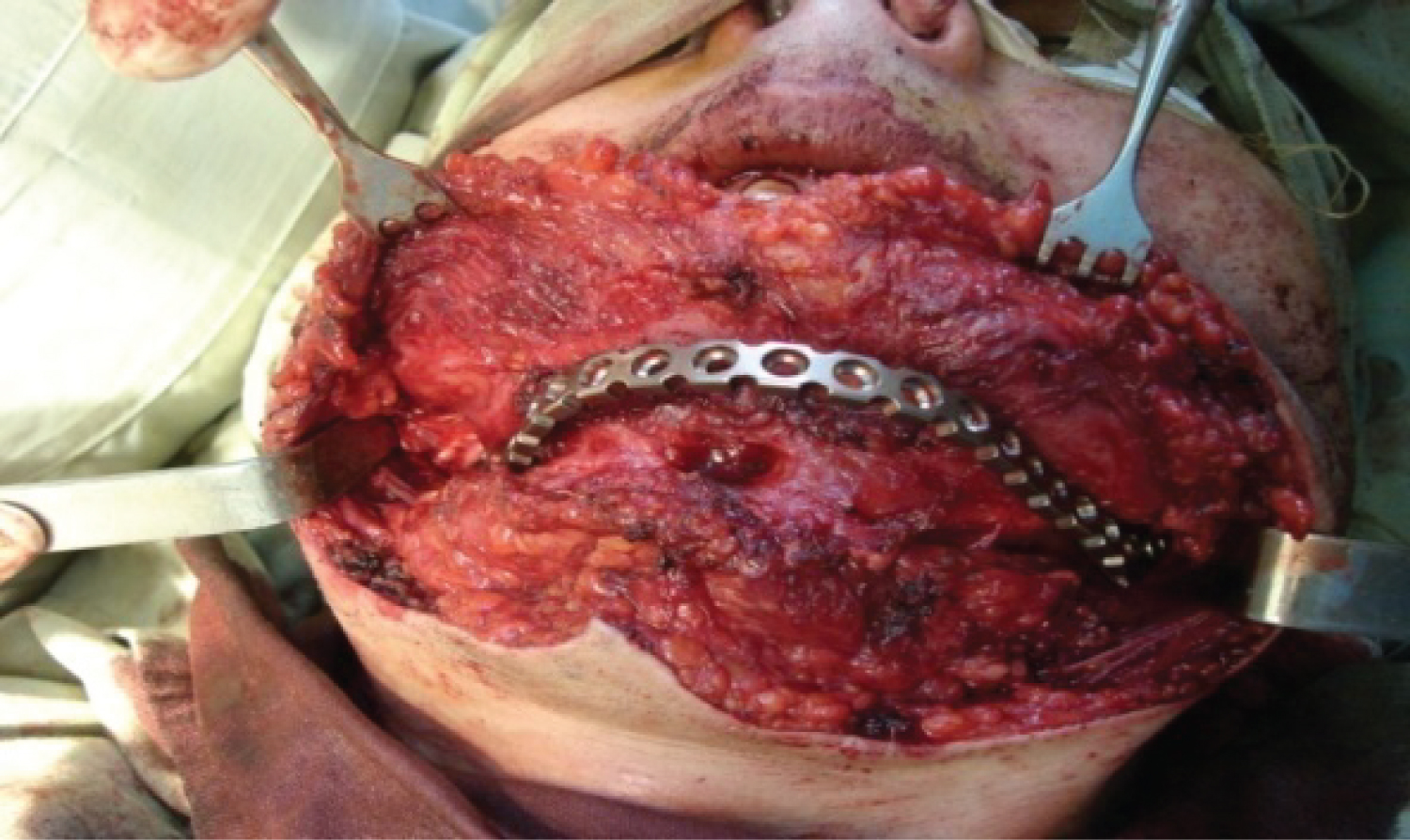 Figure 10: (Patients 1) Contoured fibula graft placed at recipient site and fixed to the mandibular bone by titanium plate and screws and imposition of the vascular anastomosis with a/v facialis.
View Figure 10
Figure 10: (Patients 1) Contoured fibula graft placed at recipient site and fixed to the mandibular bone by titanium plate and screws and imposition of the vascular anastomosis with a/v facialis.
View Figure 10
The protocol for functional reconstruction of mandibular defects consisted of several stages:
1. Resection of the tumor,
2. Reconstruction of the newly formed defect of the lower jaw using a fibula flap with free edges together with defects of the lower jaw,
3. 6 months after resection of the mandible and reconstruction with a fibula flap installation of dental implants,
4. Above the installation of a denture 4 months after the installation of the implant.
The average length of the free fibula flap was 20-25 cm, the thickness was 1.0 cm, and the length of the vascular section was 10 cm. The resulting free vascularized flap of the fibula was, if necessary, subjected to an osteotomy according to the size of the missing bone removed. The number of free fibula sections depended on the location of the bone defect և was performed according to the scheme shown (Figure 11).
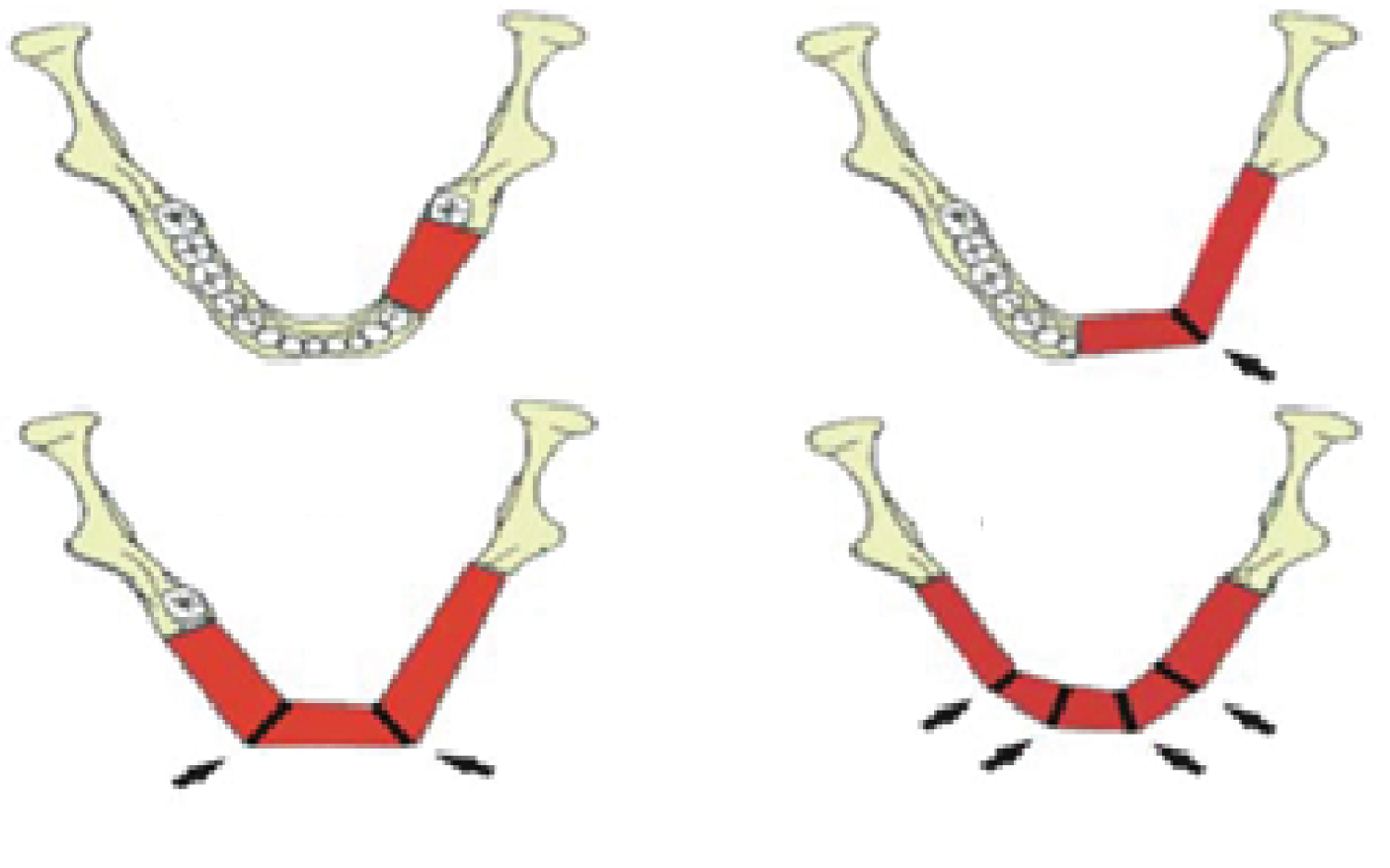 Figure 11: Free vascularized flap of the fibula segmentation scheme.
View Figure 11
Figure 11: Free vascularized flap of the fibula segmentation scheme.
View Figure 11
The simulated fibula autograft was fixed to the reconstructive bow with 1.2 mm diameter micro-screws.
The patient not received postoperative radiation therapy or chemotherapy. Postoperative clinical and radiographic controls were made regularly, using serial CT scan (Figure 3). After 4-6 months of healing, 152 dental implants were placed in the reconstructed mandible. Implants were uncovered 5-6 months after implantation. Before stage II surgery, a panoramic radiograph was taken to assess the stability of the bone level surrounding the implants and to ensure that there were no infections. Reconstructive and implant-prosthetic planning took using CT scan data and computer aided design (CAD) software.
Patients had received implant-bridge and hybrid denture that provided ideal facial balance and occlusion (Figure 5). The types of prostheses used varied among patients, depending on the need, occlusion and the number of implants that may be posted.
Successes of oral implant rehabilitation were: prosthesis success; implant success; complications; marginal bone loss (MBL).
Radiograph was used to detect any bony abnormality and evaluate alveolar bone around each implant and made as average value. Postsurgical change in marginal bone level was assess by digital x-ray were taken immediately (base line for comparison) and 3 months after implant installation, after prosthesis loading, 1 year, 3 years, and 5 years after implant installation (Figure 5, Figure 6 and Figure 12).
 Figure 12: (Patients 1) Clinical appearance after prosthetic rehabilitation.
View Figure 12
Figure 12: (Patients 1) Clinical appearance after prosthetic rehabilitation.
View Figure 12
Statistical analyses were performed using SPSS software ver. 22.0 (IBM, Armonk, NY, USA), and MedCalc program for Windows, p values < 0.05 were considered statistically significant.
Clinical observations have shown that in some patients included in the study, the surgical period passed without serious complications, and some patients developed various complications in the early postoperative period and later, as shown in Table 4 and Table 5. In the recipient area after fibula transplantation, all patients had swelling and pain in 7 patients, hematoma was observed.
Table 4: Early complication area after fibula transplantation. View Table 4
Table 5: Delayed complications area after fibula transplantation. View Table 5
The treatment objective was to achieve adequate esthetics profile, and to construct biomechanically favorable prosthesis to provide efficient masticatory function. No serious intraoperative or immediate postoperative complications were noted.
The first radiographic changes of the remnants of the remaining bone fragments and the transplant appear 50-70 days after transplantation and were completed 180 days after transplantation.
CT data on the state of the bone tissue after bone restoration surgery show that over time, bone tissue undergoes changes, gradually increasing in density over six months. In all 27 patients, fibula flaps provided adequate conditions for implant placement. Clinical investigation condition of the soft tissue the gingival, oral mucosa before implantation surgery is normal with sufficient thickness of the keratinized gum. The implants were osseointegrated, all the implants were stable and in good function with no post-operative complications.
After 6 months, the crestal bone loss of implants was evaluated by standardized periapical radiographs, the marginal bone loss (MBL) was 0.54 mm after 6 months, 0.97 mm after 12 months, after 36 months 1.23 mm, after 60 months 1.43 mm (Table 6).
Table 6: The marginal bone loss (MBL) after fibula transplantation. View Table 6
With dynamic observation, clinical and radiological indices were stable, of the 152 implants installed, 2 failed to osseointegrate and 5 after years of loading (peri-implantitis). Success rate of implants 5 years after was 96.1%.
The analysis of the close-to-long-term results of implant-reconstructive operations performed in this work suggests that a one-stage reconstructive operation, including dissection of the affected jaw, "simultaneous restoration of the defect with a vascular autograft", is a reliable method of reconstruction and makes it possible to orthopedic restoration of missing teeth using dental implants. The results of the study showed that there was a complete fusion of the two bone segments. The placement of an implant in the reconstructed bone site after reconstruction of the dissected part of the jawbone prevented unpredictable disintegration of the autograft made it possible to carry out orthopedic rehabilitation using implant-based structures.
Current trends in mandibular reconstruction are aimed at restoring a viable mandible to the proper shape and the need for invasive autogenous graft production. Many reconstruction methods have been attempted and reported for the reconstruction of the mandible, which include reconstruction rods with or without pedunculated musculocutaneous flaps, alloplasts, and free grafts including partial or cortical bone, osteomyocutaneous pedicle flaps, and many free vascularized bone grafts. However, it should be noted that no method is ideal for the reconstruction of a mandibular defect [1,28].
Оptimal reconstruction of the mandibular defects remains controversial with regard to reconstructive options, which include donor site selection, timing of surgery, and recovery method [29].
The ideal timing for mandibular reconstruction is widely discussed, and today it is widely believed that immediate reconstruction can be performed without the risk of late diagnosis of disease recurrence [30].
Prior to the advent of microsurgical techniques, delayed reconstruction was critical for the maturation of the wound bed for nonvascular bone grafting [31,32].
Immediate reconstruction has advantages over delayed mandibular reconstruction. Health-related quality of life (QOL) studies have demonstrated that immediate reconstruction significantly improves quality of life and that the majority of patients prefer immediate reconstruction [33,34].
Boyd, et al. has shown in his work that patients who underwent reconstruction using vascularized bone grafts lost an average of 4 days of life due to secondary procedures, compared with 35 days for patients who underwent reconstruction with a soft tissue graft and flap [35].
The fibula can be used up to 25 cm of bone, and the bone supply is sufficient to support dental implantation. With this length of bone, the entire mandible can be reconstructed with vascularized bone if needed. Multiple osteotomies can be performed to reshape the fibula to restore the anterior arch, body, angle, or ramus of the mandible, provided the periosteum of the fibula is intact [1]. The skin on the lower side of the leg is thin and pliable, with quite a lot of available skin, and can be tolerated in a sensitive manner. The smaller skin blades can be used to close the defect first.
The leg of the free fibular flap is the peroneal artery, a branch of the tibial trunk of the fibula. The peroneal artery passes with paired comitant veins along the entire length of the fibula; along its medial aspect. The fibula feeds on both the periosteal and endosteal blood supply. It is this double blood supply that allows multiple osteotomies and contouring to be performed to repair large defects, including those at an angle. The vascular pedicle can be lengthened by taking the more distal segment of the bone, performing a subperiosteal dissection of the soft tissue surrounding the proximal bone, and ejecting it [36].
Technological advances in medical imaging and rapid prototyping make it possible to produce 3D models. 3D modeling of the bone graft also allows the creation of templates for contour osteotomy, which saves the surgeon time and maximizes bone-to-bone contact, promoting strong bone fusion. Mandibular reconstruction using computer-aided design and computer-aided manufacturing: an analysis of surgical results [37-40].
• The basic prerequisite for successful bone grafting [41].
• Bone transplantation into healthy tissue.
• Tight contact and fixation between the adjacent bone and the graft.
• Reception area with good blood supply.
Analysis of the long-term results of implantation-reconstructive operations performed in this work suggests that a one-stage reconstructive operation, including dissection of the affected jaw, "simultaneous restoration of the defect with a vascular autograft, is a reliable method of prevention, much lower." The number of traumatic operations hides the continuation of treatment and makes it possible to orthopedic restoration of missing teeth with dental implants.
Performed bone-restoration surgeries all patients had a positive result, fibula autograft adhesion to the residual jawbone was observed.
The bone segment obtained as a result of the use of fibula autogenous bone grafts with its quantitative-qualitative parameters was sufficient for the use of intraosseous implants.
Out of 196 implants, 7 implants were removed at different times (3 during osteointegration, 1 after surgery, 2 after 3 years, 1 after surgery) 96.5%. The reason for the removal of the implants was periimplantitis, which was registered in patients who were left out of the dispensary control.
The results of the study showed that there was no disturbance in the nutrition of the remnant bone fragments of the small-vessel vascular transplant և complete fusion of the two bone fragments. Implant placement in the reconstructed area of the bone after reconstructing the dissected part of the jaw prevented the unpredictable destruction of the autograft և enabled orthopedic rehabilitation to be performed using implant-based structures.
The reconstruction of the lower jaw defects after ablation of tumors with fibular flaps is a reliable method with good long-term results. The results showed that implant treatment is effective to improve patients’ masticatory efficiency and an acceptable quality of life to the patient. The multidisciplinary approach proved to be effective in overcoming the challenges.
The author declares that he has no conflict of interest and there was no external source of funding for the present study. None of the authors have any relevant financial relationship(s) with a commercial interest.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
The work was not funded.