Facial infiltrating lipomatosis (FIL) is a rare and underreported clinical entity. Presence since birth and hemifacial swelling and asymmetry is always present along with dentoskeletal hypertrophy. Clinical management varies from conservative liposuction at an early age to aggressive subtotal resection in adulthood.
A 21-year-old female patient, operated 3 times before for unilateral facial swelling presented with massive diffuse swelling on the right side of the face. Contrast CT showed infiltrating lipomatosis with the complete fatty replacement of ipsilateral parotid gland and masseter muscle. The case was managed in our unit by staged resection of swelling and minor cosmetic corrections.
Management of facial infiltrating lipomatosis in adult patients can be done with staged resection of the lesion and cosmetic corrections for residual deformities but ideal outcome and prevention of recurrence is difficult.
Facial infiltrating lipomatosis, Facial asymmetry, Esthetic facial surgery
Facial infiltrating lipomatosis (FIL) is a distinct and rare clinical entity with less than fifty reported cases [1-17]. Slavin, et al. in 1983 described the typical histopathological features and named the disease as congenital infiltrating lipomatosis of the face [18,19]. The pathogenesis is still unclear till now though some somatic mosaicism has been implicated in a series of cases [20]. The clinical history and phenotype are widely variable [20,21]. Facial asymmetry usually in the cheek region, some deficit of facial nerve branches, mucosal neuromas and pain in buccal mucosa are always present [20]. Dental and skeletal changes like macrodontia, supernumerary tooth and periosteal apposition of involved facial bones have been reported in the literature [22,23]. Some authors have hypothesized FIL as a form of hemifacial hyperplasia [14]. Treatment options range from liposuction to radical surgical resection. Timing and choice of treatment vary among clinicians [19].
Here we present a case of a 21-year-old female with massive right-sided swelling of the face which has been operated three times before and there was scarring from previous operations. There was a deficit of facial nerve branches and binocular diplopia. Binocular diplopia has not been reported until now by other case series and reports of facial infiltrating lipomatosis as this lesion usually spares orbits and skull base structures. This clinical presentation can be confused with some other lesions hence a brief attempt at differential diagnosis has been made.
A 21-year-old female patient was seen in the department of oral and maxillofacial surgery, College of Medical Sciences Teaching Hospital, Bharatpur, Nepal with regards to facial asymmetry and pain in buccal mucosa on right side of the face. She reported a past diagnosis and had undergone at least three surgical procedures from her childhood at the age of three, nine and fourteen. She remembers that her appearance had improved after last surgery but the asymmetry recurred again to the present state.
On presentation, she had diffuse swelling over the right side of face extending from preauricular to lateral nasal area mediolaterally and from the lower eyelid to the corner of mouth superioinferiorly. She complained of pain and ulceration in her posterior right oral mucosa and loose teeth in the right upper jaw. She complained of diplopia in lower gaze, which is a unique presentation and has not to been reported. There was no gross abnormality of any other oral tissue and she didn't complain of any functional problems with speech, swallowing and breathing. There were no apparent cutaneous lesions or signs on the affected side but there was the presence of ipsilateral coarse facial hair on the cheek and upper lip (Figure 1). On facial nerve examination, she had a House Brackmann grade VI deficiency of marginal mandibular branch. All other branches had no deficiency, with normal eyelid closure and appearance of forehead wrinkles as well as nasolabial folds on the affected side. She had no complaints of dry mouth and subjective clinical examination was not conclusive for xerostomia.
 Figure 1: Clinical presentation of gross facial asymmetry, coarse facial hair and deficit of facial nerve branches.
View Figure 1
Figure 1: Clinical presentation of gross facial asymmetry, coarse facial hair and deficit of facial nerve branches.
View Figure 1
CT scan soft tissue window is a good modality for evaluation of facial mass and its extension into adjacent soft tissue structures [10]. Ultrasonography has good contrast resolution but very low spatial resolution and is not recommended for determination of deep soft tissue lesions with extensions [24]. MRI has the best contrast resolution for soft tissue lesions and is considered the gold standard but lacks the spatial resolution provided by CT scan [24]. Delineation of extension and infiltrations are very important information to plan a surgical resection hence contrast-enhanced CT scan was considered the best radiographic alternative for the lesion [25]. Contrast-enhanced Computed tomography (CECT) was obtained which demonstrated a diffuse lipomatous mass infiltration in the subcutaneous tissue on the right side of the face and temporal region and involvement of eyelids, temporal and infratemporal fossa (Figure 2). There was hypertrophy of right masseter and temporalis muscle with fatty changes and fat stranding between the muscle fibres. Right parotid gland couldn't be visualized suggestive of complete fatty replacement. There was no intracranial, nasal or orbital extension. No extension in deep or superficial neck spaces could be seen. There was the presence of focal cortical thickening and periostitis in the right maxilla and zygoma (Figure 3). Haematological investigations were within the normal range. After an incisional biopsy, histopathology showed lobules of mature adipocytes separated by fibrocollagenous septa and absence of any cellular atypia which suggests negative for malignancy.
 Figure 2: CECT soft tissue window showing diffuse lipomatous infiltration of subcutaneous tissue, masseter muscle and complete obliteration of parotid gland.
View Figure 2
Figure 2: CECT soft tissue window showing diffuse lipomatous infiltration of subcutaneous tissue, masseter muscle and complete obliteration of parotid gland.
View Figure 2
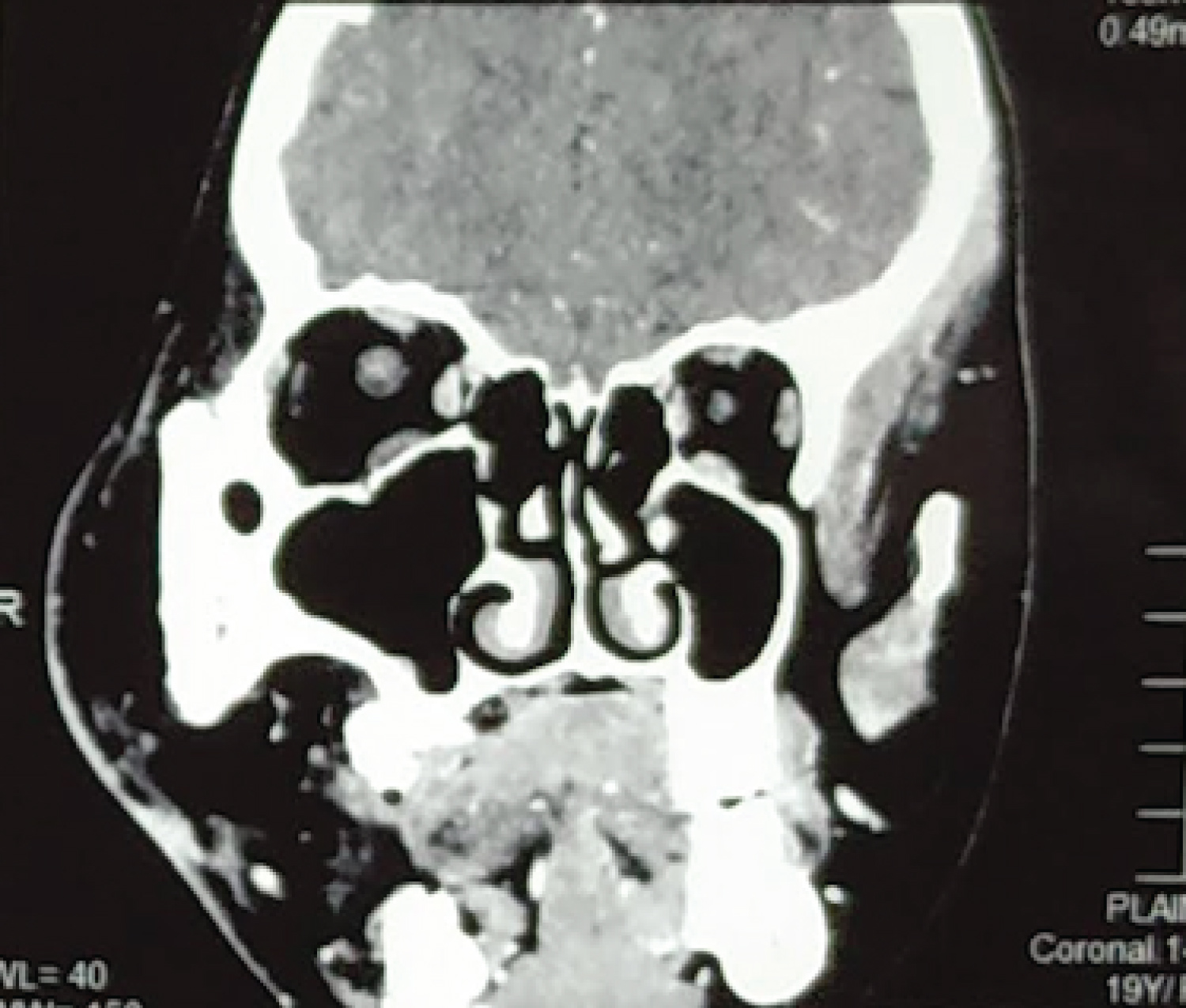 Figure 3: CECT showing periosteal reaction and hypertrophic zygomatico maxillary complex involving a lateral nasal wall, infraorbital rim and body of zygoma.
View Figure 3
Figure 3: CECT showing periosteal reaction and hypertrophic zygomatico maxillary complex involving a lateral nasal wall, infraorbital rim and body of zygoma.
View Figure 3
The natural history, presentation, CT findings and histopathological report confirmed the diagnosis of congenital infiltrating lipomatosis of the face. Two surgical resections were performed, the first stage consisted of radical resection of parotid and masseter, temporalis muscle infiltration along with subtotal resection from cheek through a preauricular and intraoral approach. Surgical recontouring of the hypertrophied maxilla and zygoma was performed with rotary burs and irrigation. The second stage consisted of resection of fatty mass from right eyelid, lips, corner of mouth, buccal mucosa and lateral nasal area with midtarsal, intraoral and lateral nasal incisions. Excess skin tissue was trimmed and incisions closed with sutures in cosmetically less visible shadow of lateral nasal area and eyelid with 6-0 Prolene sutures. The right corner of the mouth and buccal mucosa were resuspended at a more superior position with a 2-0 nylon suture to obtain a static suspension.
Immediate postoperative period showed flushing and exaggerated swelling of the right side of the face which subsided after 15 days of follow up (Figure 4). There was an improvement in the symmetry of the face, better lip competence during speech and resolution of diplopia. The patient was satisfied with the treatment at six months follow up though she was advised regarding prognosis, recurrence and possible requirement of further interventions. At one year follow up through telecommunication as the patient has moved abroad and has planned to return for clinical follow up only after few years, she is satisfied with the correction of facial asymmetry, diplopia and painful buccal neuromas but the static suspension of the angle of mouth and lip has relapsed and is disconcerting. She is advised for dynamic lip suspension and facelift in the next stage (Figure 5).
 Figure 4: Immediate postoperative result of debulking subtotal resection of the tumour, trimming of excess skin, static suspension of the corner of mouth and sulcoplasty of the right lip and oral vestibule.
View Figure 4
Figure 4: Immediate postoperative result of debulking subtotal resection of the tumour, trimming of excess skin, static suspension of the corner of mouth and sulcoplasty of the right lip and oral vestibule.
View Figure 4
 Figure 5: Post-operative photograph: Frontal view at 6 months follow-up.
View Figure 5
Figure 5: Post-operative photograph: Frontal view at 6 months follow-up.
View Figure 5
Slavin, et al. first described and characterised the disease in detail and provided the term congenital infiltrating lipomatosis of the face in 1983, these include infiltration of fat into surrounding tissue and bony hypertrophy; absence of malignant features; absence of lipoblasts; the presence of fibrous elements; increased blood vessels, exhibiting unifocal thickened muscular walls; an increased number of nerve bundles associated with focal fibrosis [18]. Clinically distinguishing features are a presence at birth, unilateral facial involvement without the involvement of any other body part and presence of mature adipocytes [25]. There is also hypertrophy of dentoskeletal tissue on the affected side and presence of oral mucosal neuromas with painful ulcers on the affected side [9,19,22]. There are cases reported with macroglossia, macrodontia and early eruption of primary and secondary dentition (Table 1) [23].
Table 1: Review of published cases of facial infiltrating lipomatosis. View Table 1
The differential diagnosis for the presentation of unilateral facial symmetry can be ipsilateral hemifacial hyperplasia or contralateral atrophic diseases like Parry Romberg disease or Hemifacial macrosomia [26]. Fatty swelling on the face can be presenting signs in angiolipoma or facial angioma though these lesions are more localised and associated with cutaneous signs as well as an absence of mucosal neuromas and dentoskeletal hypertrophy [27]. Facial asymmetry of Neurofibromatosis will present with classic cafe au lait spots and is clinically distinct [27].
Liposarcoma and lipoblastomatosis are malignant conditions characterised by signs of malignancy and immature lipoblasts on histopathology [21]. Lymphangiomas also present with diffuse soft tissue swelling but these are commonly present in the cervical region and easily distinguished on a CT/MRI [10].
The pathogenesis of FIL is not completely understood. Some authors believe it has a hormonal association which might account for multiple recurrences in adolescence [28]. Presence of ipsilateral male pattern coarse hair might be due to associated hormonal imbalance. Neoangiogenesis has been implicated in its growth and anti-angiogenic medications have been tried for management. Association with Cytomegalovirus was also seen in few reported cases but the viral aetiology could not be confirmed [3]. A recent hypothesis is that congenital infiltrating lipomatosis of the face is a lipomatosis of the trigeminal nerve and nerve-territory overgrowth [29].
Maclellan, et al. in 2013 studied parallel sequenced libraries enriched for coding sequences from genes involved in pathways that control cell growth using targeted capture in 4 patients and identified a different missense mutation in PIK3CA in each patient's affected tissue. PIK3CA encodes the catalytic subunit of the enzyme phosphoinositide-3-kinase (PI3K), which promotes cell growth [30]. Somatic mosaic mutations in PIK3CA cause FIL and similar mutations have recently been identified in patients with other overgrowth disorders including Congenital Lipomatous Overgrowth, Vascular Malformations, Epidermal Nevis, Spinal/Skeletal Anomalies/Scoliosis (CLOVES) syndrome, hemimegalencephaly, and segmental fibroadipose hyperplasia. PIK3CA inhibitors are currently in clinical trials for cancers containing PIK3CA mutations; they may be efficacious in patients with FIL and other PIK3CA-associated overgrowth syndromes [17,31].
Conservative management with liposuction and subtotal resections are favoured to prevent facial nerve injury at an early age and allow the completion of facial growth [32]. These patients undergo attempted resections at some point during their early adulthood with an average of 3 surgeries till they reach their third decade of life [20]. Surgical resections are always limited by facial nerve and diffuse infiltrating nature of the lesion. Surgical recontouring of hypertrophied bones is performed at the same time. High probability of recurrence and requirement for further surgeries should be communicated to the patient. Along with resection, static suspension of the corner of the mouth and upper lip, sulcusplasty and cosmetic trimming and redraping of excess facial soft tissue can give partially acceptable results [9]. This disease has a good prognosis as it is not life-threatening and combined surgical techniques can result in average to good aesthetics but the high and early recurrence combined with facial nerve deficits makes complete ablation and absolute correction of facial asymmetry impossible [19,21]. Interdisciplinary management with adjunctive targeted therapy and customized to the individual disease have been attempted with Thalidomide and Imatinib [28]. Imatinib was famously designed to treat the BCR-ABL fusion protein of chronic myelogenous leukaemia and competitive inhibitor of any protein with an ABL type tyrosine kinase. Imatinib is generally well tolerated with very few adverse effects [28].
Here we presented a case of 21 years female with facial symmetry which was radiographically and histopathologically confirmed as facial infiltrating lipomatosis and managed with two-stage surgery. This is an extremely rare disease. We present the case and our surgical method of treatment to add evidence for the management of this disease. Early and staged surgeries targeted at debulking and sparing the facial nerve along with targeted adjunctive gene therapy or chemotherapy may be helpful to control the lesion. Late presentation of recurrence after multiple surgeries with facial nerve deficits and bony involvement is difficult to correct.
The authors declare that the report is free of any conflict of interest.
Informed and written consent was obtained from the patient regarding using her photographs and clinical data for research purpose by the primary author himself.
We acknowledge the interns posted in our unit for the photographs.