Osteomas are benign neoplasms that produce well-differentiated mature bone tissue. There are three clinical varieties: Central, peripheral, and extra-skeletal osteoma. In the craniofacial region, cases have been reported in different bones, with its location in the mandible being less prevalent, especially at the condylar level. Generally, they present in isolation, however, when their presentation is multiple, they can be associated with Gardner's Syndrome. The presence of symptoms is rare, and will depend on both the location and the size achieved by the osteoma. Depending on a number of factors, there are several treatment modalities for osteomas, with an excellent prognosis. Recurrences are rare and malignant transformation has never been described. We report a case of a 36-year-old woman with long-standing multiple mandibular osteomas not associated with Gardner's Syndrome, the treatment performed, and evolution over time.
Mandibular osteoma, Peripheral osteoma, Osteogenic tumor, Oral pathology, Facial asymmetry, Mandibular condyle
Osteomas are benign, slow-growing and progressive neoplasms (caused by the activity of either the periosteum or the endosteum), that form well-differentiated mature bone tissue [1]. Depending on their origin, three clinical varieties of the same pathology have been described; central, peripheral and extra-skeletal osteoma, with the peripheral variety being the most common [2]. The etiopathogenesis of the osteomas is unknown, however, various authors have pointed out a possible causal relationship with a history of trauma, chronic infection, excessive muscular activity, and embryogenic or endocrine alterations [3,4].
In the craniofacial region, peripheral osteomas are more frequent in the nasal bones and paranasal sinuses [5]. In the maxillary bones, its presentation is rare, and leaving the maxillary sinus aside, the mandible is the most frequently affected place, particularly the region of the angle and basilar border, with the mandibular ramus and condyle being the least affected areas [6]. They have also been described in the external auditory canal, the orbital region, the temporal bone, and the pterygoid process [5-9].
Osteomas usually present in isolation. However, it is possible to find cases of multiple osteomas, with the risk that the patient has other underlying conditions, such as Gardner's Syndrome [10,11]. This is why other clinical signs associated with it should be investigated, such as digestive polyps (possible malignant evolution), cutaneous tumors, exostosis of the skull, and supernumerary teeth [6].
Peripheral osteomas appear as unilateral, mobile, pedicled, and well-defined masses, with an average diameter between 10 to 40 mm [2]. They do not have a predilection for sex or age, although they are more frequently found between the third and fourth decades of life [4]. Generally, they are asymptomatic, and the main reason for consultation being facial asymmetry produced in more advanced cases. In addition, in the case of compromising or compressing the path of some nervous element, they could cause a certain degree of paresthesia [6].
Radiologically, they are seen as well-defined radio opaque areas, circular or oval in shape, attached through a pedicle to the underlying bone tissue. In occlusal radiographs the peripheral osteoma of the mandible is classically well-circumscribed, oval, radiopaque with a narrow contact area at the vestibule and with a density similar to normal bone [9,12]. The use of multiplanar and three-dimensional imaging such as computed axial tomography allows for a complete preoperative evaluation and adequate therapeutic planning. Histologically, osteomas can be compact or cancellous, depending on the number of bone trabeculae and medullary spaces present. Osteoid tissue contains cells like osteoblasts from normal nuclei with no signs of cell atypia or malignancy [8]. As differential diagnoses, several inflammatory and neoplastic pathological entities should be considered, such as complex odontoma, ossifying fibroma, fibrous dysplasia, Paget disease, chronic focal sclerosing osteomyelitis, chondroma, osteoid osteoma, osteoblastoma, Pindborg tumor, and low-grade osteosarcoma [1,4].
The treatment of peripheral osteoma is the surgical excision with complete removal of the lesion and bone remodeling. The prognosis is excellent, recurrences are rare (< 1%), and malignant transformation has never been described in the literature [5,10]. The purpose of this article is to present a rare case of multiple mandibular osteomas, and to analyze its clinical, radiographic, histopathological characteristics, and treatment.
36-year-old female patient, without relevant medical history, was referred to the Maxillofacial Surgery Unit of the Hospital del Salvador (Santiago, Chile), for progressive increases in volume (six years of evolution) at the level of the mandibular body and left preauricular area, painless, well defined and of hard consistency (Figure 1). The patient complains of paresthesia at the level of the left labial commissure, and sounds in the left temporomandibular joint when she eats. The mouth opening is normal, without deviations, and no significant occlusal discrepancies were detected. The skin and oral mucosa of the affected areas appear healthy. A history of local trauma, infection, or some other causal factor was ruled out. A craniofacial computed tomography scan is requested, which shows the presence of three hyperdense areas with net edges and pedicled base, each one with an average size of 20 mm in diameter, compatible with peripheral mandibular osteomas. One is located at the level of the left mandibular body, very close to the exit of the mental nerve, another is located on the lateral aspect of the left mandibular condyle and finally the other is located on the internal aspect of the left mandibular condyle. Cortical perforation and periosteal reaction are not observed (Figure 2).
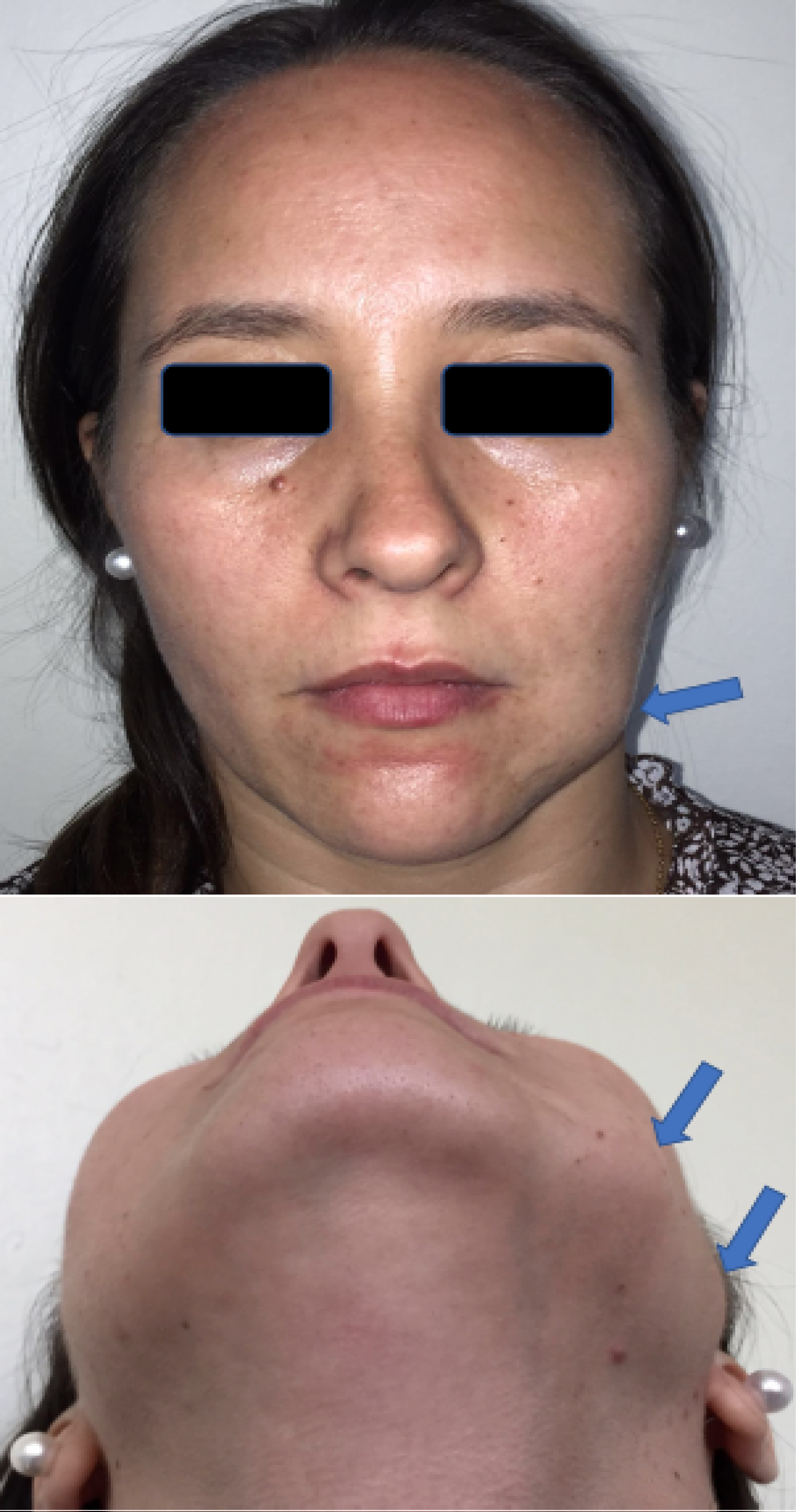 Figure 1: Pre-operative clinical photography. Note the increase in volumen at the level of the mandibular body and left preauricular area (arrows) caused by osteomas.
View Figure 1
Figure 1: Pre-operative clinical photography. Note the increase in volumen at the level of the mandibular body and left preauricular area (arrows) caused by osteomas.
View Figure 1
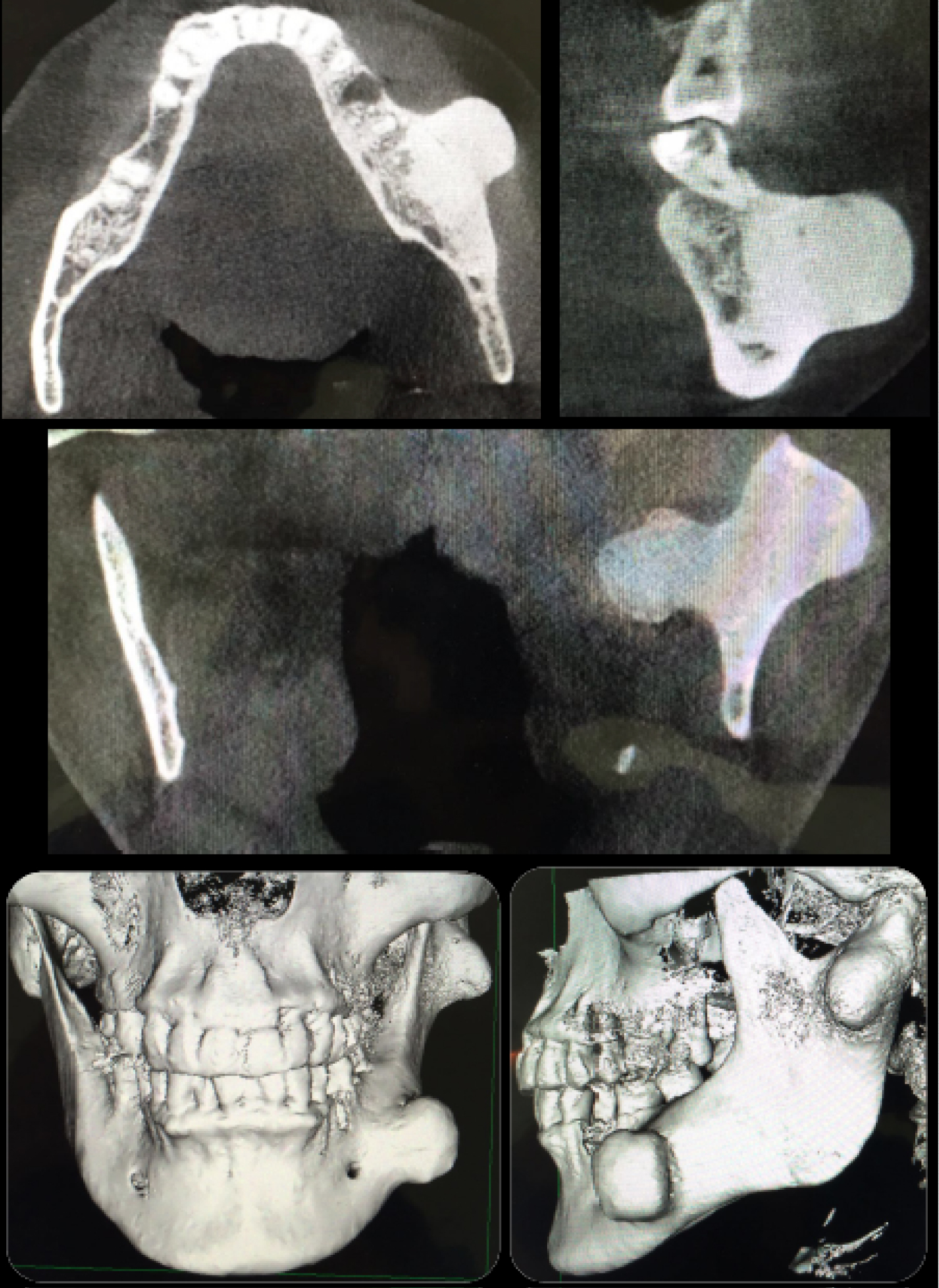 Figure 2: Pre-operative study. Axial and coronal sections of computed tomography show the different osteomas, both at the body level and the left mandibular condyle. Frontal and lateral views of three-dimensional reconstruction, showing the size and exact location of the mandibular osteomas.
View Figure 2
Figure 2: Pre-operative study. Axial and coronal sections of computed tomography show the different osteomas, both at the body level and the left mandibular condyle. Frontal and lateral views of three-dimensional reconstruction, showing the size and exact location of the mandibular osteomas.
View Figure 2
Due to the presence of multiple osteomas, a study was performed to rule out association with Gardner Syndrome. An interconsultation for colonoscopy examination was performed, which did not detect the presence of intestinal polyps. Furthermore, the patient denied symptoms such as abdominal pain, diarrhea and rectal bleeding. On the other hand, the patient did not present epidermoid cysts, fibroids, supernumerary teeth or odontomas. The same clinical investigation of signs and symptoms related to Gardner's Syndrome was carried out on the patient's direct family, not finding any relationship with the disease.
Based on the clinical and imaging history obtained, complete resection of osteomas by intraoral approach is planned. Under general anesthesia, vestibulotomy was performed at the level of the left mandibular body, identifying and separating the mental nerve, and then using the PiezoART III® piezoelectric system (Dowell dental products, USA), performed an osteotomy at the base of the lesion in order to resect it (Figure 3). An intraoral approach was also performed to access the external and internal aspects of the mandibular ramus to reach the other two osteomas. Once identified and isolated, they were resected through osteotomies at the base of the lesion and sent for histopathological study. At the end of the procedure, the surfaces in relation to the osteomas were remodeled (osteoplasty) with a round bur. After hemostasis control, a wash with physiological serum and closure of the approaches with catgut 4-0 are performed. Compressive facial dressings were installed at the end of the procedure.
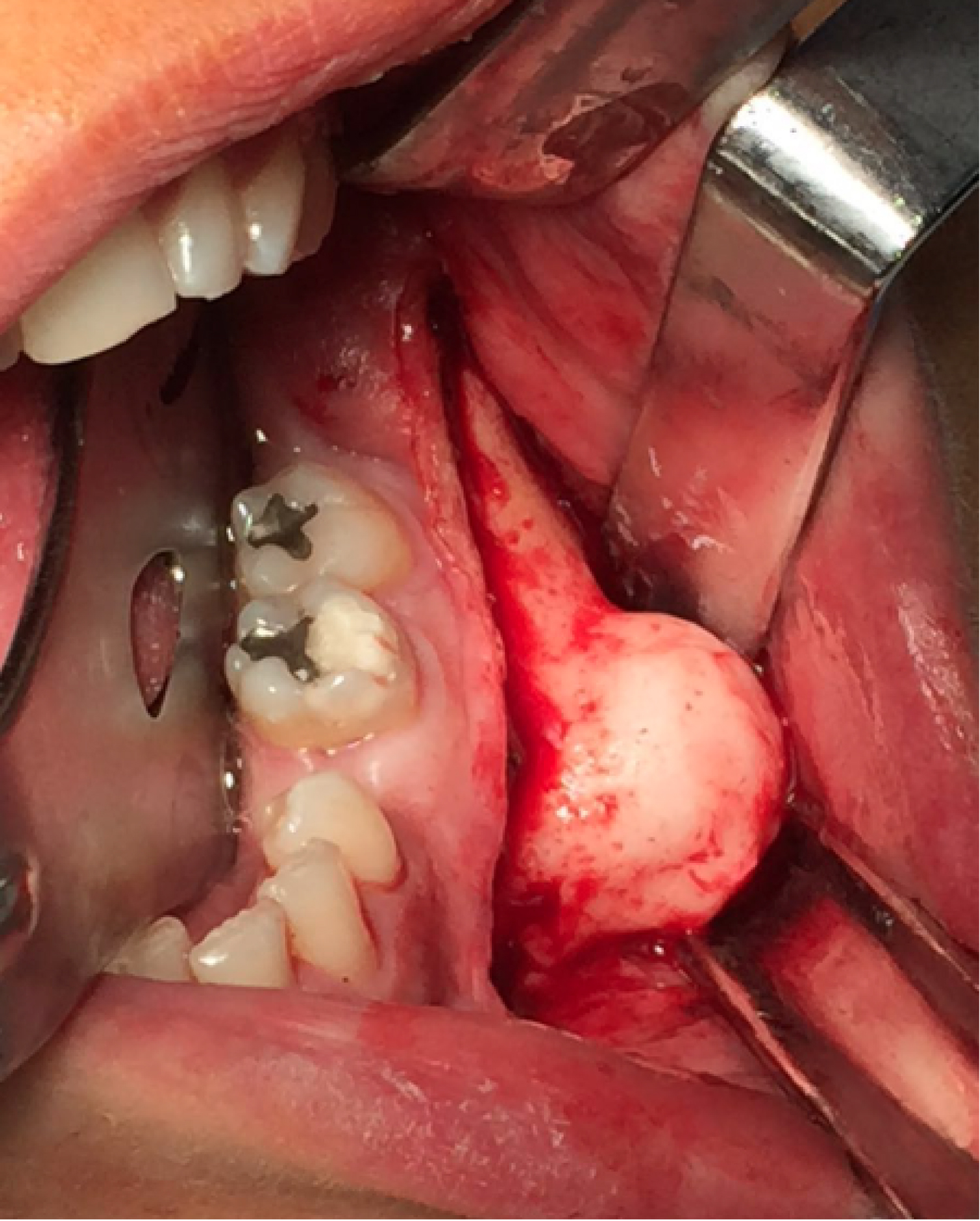 Figure 3: Vestibulotomy performed at the level of the left mandibular body. A well identified osteoma is observed near the exit of the mental nerve.
View Figure 3
Figure 3: Vestibulotomy performed at the level of the left mandibular body. A well identified osteoma is observed near the exit of the mental nerve.
View Figure 3
The delayed biopsy confirmed the diagnosis of compact peripheral osteomas, where a benign osteogenic lesion was observed through staining with hematoxylin and eosin, which contained large areas of highly compact lamellar bone deposition, proliferation of irregular trabeculae, with few osteons and spaces marrow, containing hematopoietic marrow tissue with cellular connective tissue, fibroblast-like spindle cells, and some blood vessels (Figure 4). The day after surgery, the patient was discharged, with the indication of periodic controls. One year after clinical and radiographic controls, an improvement in symptoms was observed, as well as a correction of facial asymmetry (Figure 5). In addition, a normal anatomy is observed in the control scanner, with no signs of recurrence (Figure 6).
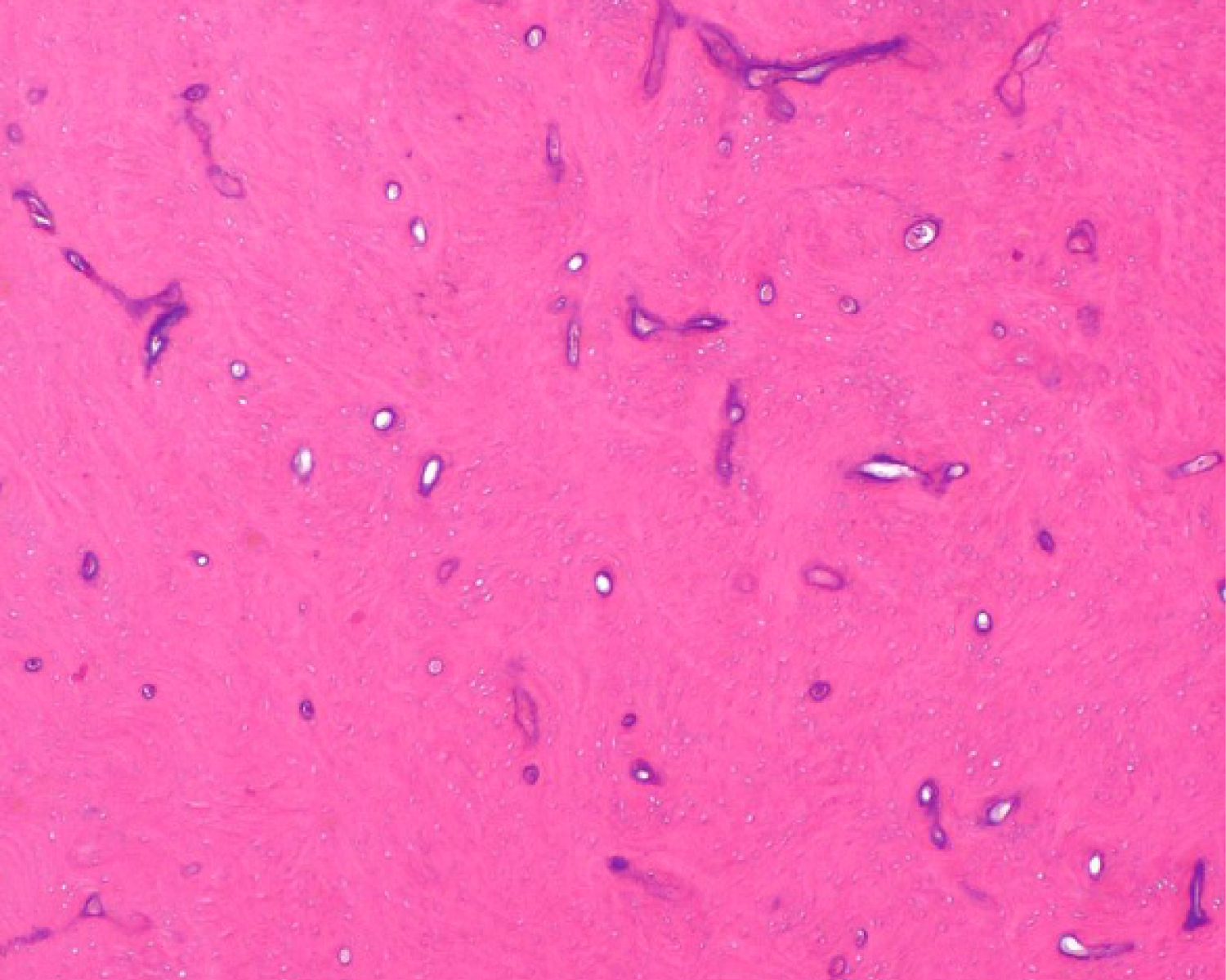 Figure 4: Histopathological analysis. The typical microscopic charcteristics of a peripheral osteoma are observed, with large areas of highly compact lamellar bone deposition, proliferation of irregular trabeculae, with few osteons and spaces marrow, and some blood vessels (haematoxylin-eosin staining; original magnification X40).
View Figure 4
Figure 4: Histopathological analysis. The typical microscopic charcteristics of a peripheral osteoma are observed, with large areas of highly compact lamellar bone deposition, proliferation of irregular trabeculae, with few osteons and spaces marrow, and some blood vessels (haematoxylin-eosin staining; original magnification X40).
View Figure 4
 Figure 5: Clinical control 12 months post-operative. An adequate correction of the facial asymmetry caused by the osteomas is observed.
View Figure 5
Figure 5: Clinical control 12 months post-operative. An adequate correction of the facial asymmetry caused by the osteomas is observed.
View Figure 5
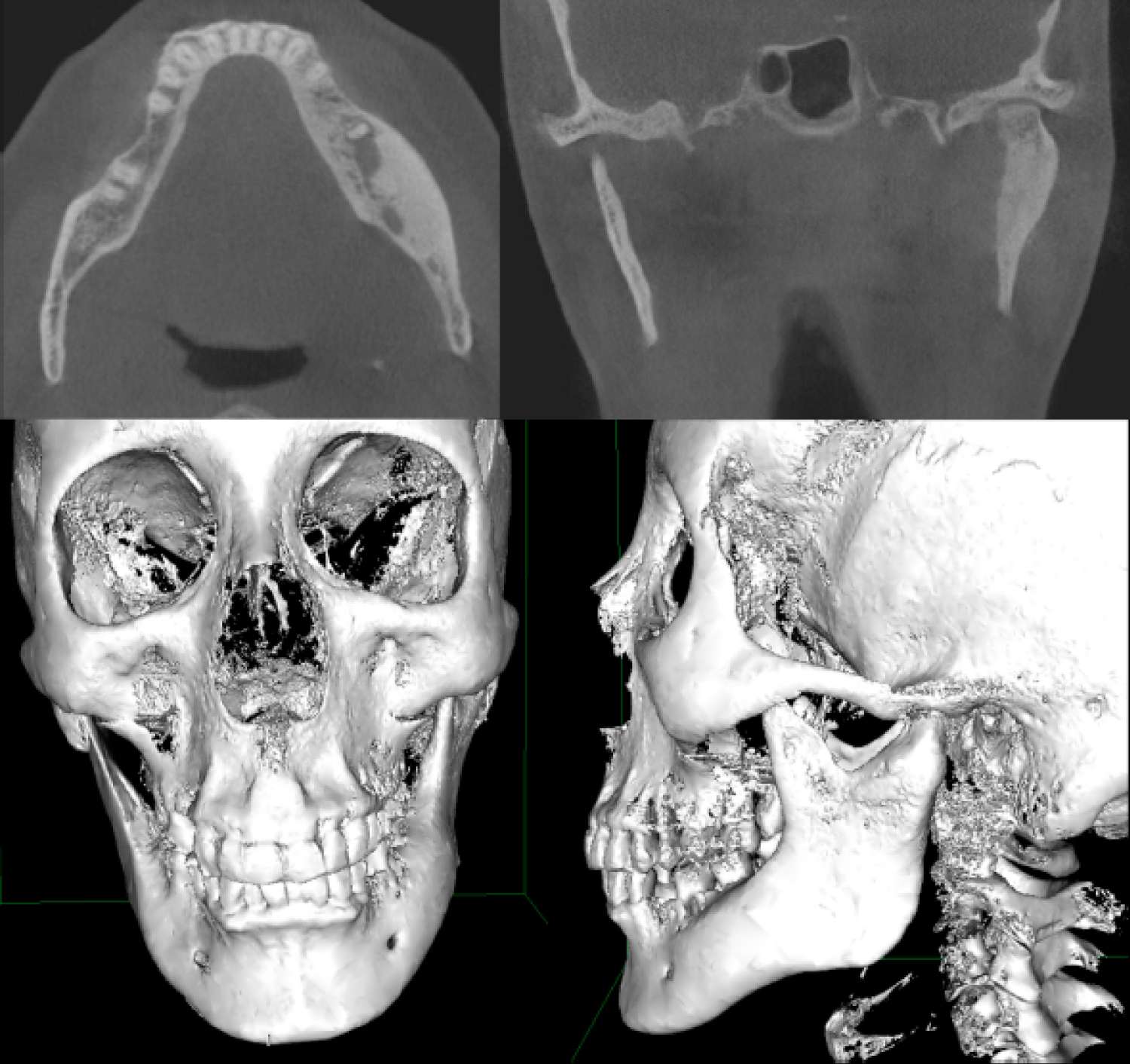 Figure 6: Post-operative study. Axila and coronal sections of the CT, and three-dimensional computed tomography reconstruction (12 months post-operative). Front and lateral view, where a complete restoration of the normal mandibular anatomy is observed, without radiographic signs of recurrence.
View Figure 6
Figure 6: Post-operative study. Axila and coronal sections of the CT, and three-dimensional computed tomography reconstruction (12 months post-operative). Front and lateral view, where a complete restoration of the normal mandibular anatomy is observed, without radiographic signs of recurrence.
View Figure 6
The clinical, radiographic and microscopic features of the case described in this article support a diagnosis of multiple peripherals osteomas of the mandible. Osteomas are benign, slow growing bone tumors characteristic of the craniomaxillofacial region. Its actual incidence and prevalence are unknown, since most cases are asymptomatic [5]. Because of this, when they are located in the jaw, the main reason for consultation is usually the facial asymmetry that they cause as they grow. Other later symptoms that can occur, and that are closely related to their size and location, are neuralgia and paresthesia [6].
Although the etiopathogenesis of osteomas is unknown, a number of causal factors have been described [4]. Another fact to be considered is that osteomas are usually found in regions close to the muscular insertions, which leads to the proposition of a possible mechanism involved of muscular traction that, associated with a bleeding or subperiosteal edema, would elevate the periosteum, resulting in an osteogenic process [3]. Patients with multiple osteomas should be evaluated for Gardner's syndrome [11]. These patients may present with symptoms of rectal bleeding, diarrhea, and abdominal pain. The triad of colorectal polyposis, skeletal abnormalities, and multiple impacted or supernumerary teeth is consistent with this syndrome [13]. In this case, Gardner syndrome was ruled out due to a negative colonoscopy, the lack of gastrointestinal and skin manifestations, and the absence of a family history related to the disease. Also, there is no history of trauma or previous infection. We believe that the formation of the osteomas presented in this case could be related to the presence of small repetitive microtrauma, which are imperceptible to the patient, so they are often not remembered. These microtraumas would have the ability to trigger an inflammatory process under the periosteum, causing an osteogenic process.
Osteomas that affect the temporomandibular joint are scarce, and they can cause anatomical and functional alterations, such as facial asymmetries and temporomandibular dysfunction [14]. In the case presented, the patient had three mandibular osteomas, one at the level of the left mandibular body, and two at the level of the left mandibular condyle. In a review of 106 craniofacial osteomas, only six were located in the mandibular condyle. Furthermore, only 26 cases had more than one osteoma [5]. On the other hand, a more recent review shows that there are only 23 cases reported in the literature of mandibular osteomas located in the condyle [15]. Literature review from the authors found a total of 27 mandibular osteomas in 26 patients, 16 females (61.5%) and 10 males (38.5%), with 17 cases in females (62.9%) and 10 cases in males (37.1%), while the age average was 39-years-old in females, and 38-years-old in males. These data were obtained through a computerized review of the literature in Pubmed (MEDLINE) and Clinically search engines, using the search terms: "mandibular osteoma" and "temporomandibular joint osteoma", finding a total of 36 articles, of which 14 were eliminated for being only in "abstract" format and those that didn't provide enough information (age, gender, symptoms, treatment, etc.), selecting a total of 22 articles for the revision.
Various treatments have been reported for mandibular and condylar osteomas, and the choice of one or the other will depend on many factors that must be evaluated together to be able to choose the best treatment for each patient. The choice of treatment is directly related to the presence of signs and symptoms, location, pattern of proliferation, extension and size of the lesion [15]. The treatment of asymptomatic osteomas is controversial, with a conservative approach recommended in most cases, leaving surgical treatment for symptomatic cases [4,5]. In our review, the most common were trismus (69.2%), malocclusion (26.9%), facial asymmetry (30.7%), swelling in TMJ area (7.6%) and pain (57.6%). In the case presented, the patient consulted for facial asymmetry, paresthesia, and joint sounds, which affected his quality of life, so we decided to perform surgical treatment.
Surgical resection may be indicated in some cases when the osteoma causes functional or aesthetic discomfort (facial asymmetry and occlusal changes), pain, trismus, traumatic ulcers, or periodontal disorders [6,16]. In addition, the type of approach selected should allow adequate viewing and access for the amount of tissue to be removed, and an optimal aesthetic result [7]. The choice of a resection must also consider the potential risks related to the surrounding anatomical structures (nerves and blood vessels) [3]. Regarding the anatomical structures close to the lesion, in this clinical case, one of the osteomas was very close to the exit of the mental nerve. The presence of a lesion close to this area, many times implies the need for transposition or lateralization of the same nerve. However, with the use of the piezoelectric system and correct visualization and separation of the lesion, it was not necessary to perform this procedure [17,18].
Depending on size, location, and growth vector, condylar osteomas (like condylar hyperplasia) can generate facial asymmetries, manifested by asymmetric mandibular prognathism and altered occlusion [19]. Condylar osteomas can be classified according to their proliferation pattern in central and peripheral [16]. In general, peripheral osteomas are usually pedicled and respect the shape of the condyle since their proliferation pattern does not imply a condylar replacement, so facial and occlusal changes will depend on the location of the osteoma [20]. As they are generally located in the lateral or medial pole, these alterations will be absent, requiring a more conservative resection [16]. However, central type condylar osteomas generate a replacement of the mandibular condyle, causing an alteration of the condylar anatomy and as a consequence facial and occlusal alterations, requiring a major resection through a condylectomy [15]. Also, it is possible to carry out a bone remodeling, but it increases the risk of a recurrence. In these cases, orthodontic treatment is also indicated for better results on occlusal function and facial appearance. Regarding the location and extent of osteomas, there are reports that the proximity to important anatomical structures, such as blood vessels and nerves, growth towards the middle cranial fossa, or the location on the articular surface of the mandibular condyle indicate the surgical resection of the lesion [19,21,22]. Size is another factor to consider. A large osteoma will involve a large resection and the need for subsequent reconstruction, unlike a smaller osteoma where removal of the lesion will enough [23-25].
Other treatments described are arthroplasty alone or with interposition of adipose tissue or temporal muscle flap between the bone articular surfaces [15]. For cases of large condylar osteomas, recurrences, or ankylosis, where a more aggressive resection involves loss of anatomy and masticatory function, joint reconstruction should be considered as the first option [19,26,27]. There are different methods to reconstruct, among them we have the use of autologous iliac crest or costochondral bone grafts fixed with reconstruction plates, or the use of joint prostheses (stock or customized) for total joint replacement [24,27].
Different mechanisms have been described to facilitate the surgical treatment of this pathology. Among them, endoscopically assisted removal (in cases of paranasal sinus osteomas or in areas of reduced visibility) and the use of the piezoelectric system [7,18,28,29]. The piezoelectric system has also been described for the resection of osteomas, presenting a series of advantages over conventional rotary devices, such as a more precise cut, which avoids the use of a chisel in the final stages of osteotomy, better hemostasis, less coagulative necrosis in the surrounding bone tissue, better visibility, and less damage to the anatomical structures close to the injury. This has allowed a significant decrease in complications associated with surgery [18,29].
Based on what has been discussed, and the clinical characteristics of the case presented (associated symptoms, growth pattern, location and size of the osteomas), we believe that the selected treatment is appropriate, since, as we saw, resection with condylar preservation as the only treatment is indicated for moderately sized osteomas associated with symptoms, where the location and pedicled shape facilitate resection, without generating significant alterations in anatomy, occlusion and masticatory function. In conclusion, mandibular osteomas are rare benign lesions that can significantly affect the quality of life of the patient. The importance of this case lies in the complete and sequential evaluation of all the factors that affect the choice of treatment. Osteomas can be part of a syndrome that is associated with gastrointestinal cancer, therefore, we must rule out its presence. The correlation of clinical history and imaging tests allow a correct planning of the surgical intervention, increasing the safety and success of the procedure. On the other hand, histological diagnosis is essential to establish the final diagnosis. Despite the low recurrence, long-term clinical follow-up is important, since recurrences have been reported after nine years.
The authors have no commercial or financial associations that might create a conflict of interest with the information presented in this manuscript.
The authors declare an equal participation in the preparation of this article.