The Stafne bone cavity (SBC) is classically described as an asymptomatic unilateral depression or concavity localized on the medial surface of the posterior mandible between the inferior alveolar canal and inferior border. The authors present a rare case report of the Stafne bone cavity (SBC) in the bilateral ramus of the mandible that has not been previously reported in the English medical and dental literature. The bilateral anatomic location proved to be a diagnostic challenge using plain film radiography. Imaging studies such as cone beam CT scans can assist the clinician in the definitive diagnosis without surgical intervention.
Stafne bone cavity (SBC), Rare, Bilateral, Ramus, Anatomic variant, Cone beam CT scan
Stafne bone cavity (SBC) is classically described as an asymptomatic unilateral depression or concavity localized on the medial surface of the posterior mandible between the inferior alveolar canal and inferior border [1]. It is considered a pseudocyst as the lesion does not have an epithelial lining. It is hypothesized that during embryological development of the mandible from Meckel's cartilage, the submandibular gland tissue is entrapped that leads to an osseous concavity on the medial surface of the mandible [1,2]. The authors present a case report of the Stafne bone cavity (SBC) in the bilateral ramus of the mandible observed on panoramic radiography and cone beam computed tomography (CBCT) that has not been previously reported in the English medical and dental literature.
Radiographic features (Figure 1) of the SBC are a well-circumscribed unilocular, round or elliptical shaped radiolucency in the posterior mandible that are approximately 10 to 30 mm in length [1,3,4]. The radiographic lesion is often incidentally discovered when the patient completes a routine panoramic radiograph at the dentist office and does create concern for the dentist as it can mimic a cystic lesion [3,5,6].
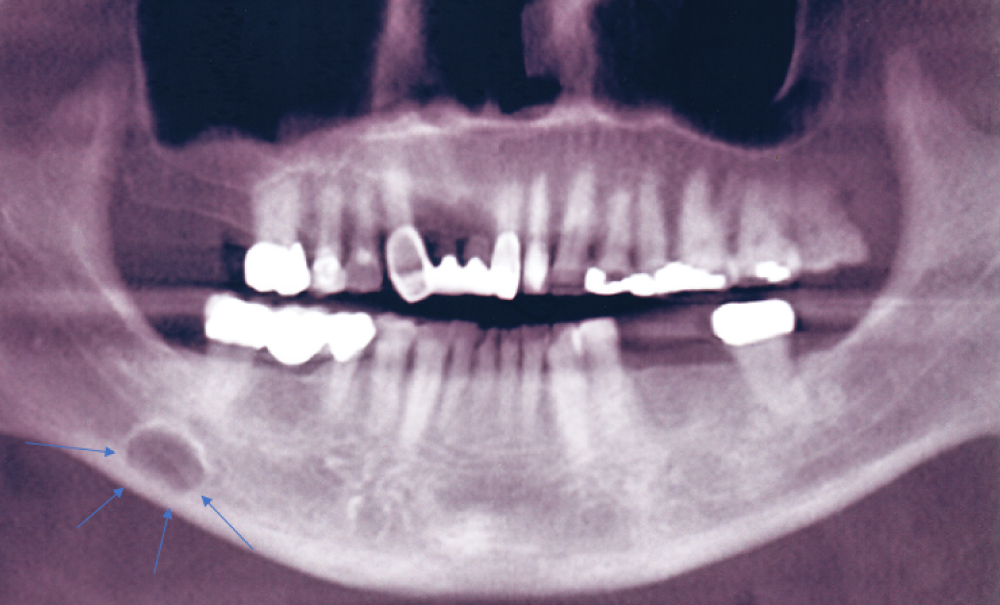 Figure 1: Panoramic radiograph of classically described SBC of the right posterior mandible illustrates the well-defined unilocular radiolucency in the right posterior mandible between the inferior alveolar canal and the inferior border of the mandible (Blue arrows).
View Figure 1
Figure 1: Panoramic radiograph of classically described SBC of the right posterior mandible illustrates the well-defined unilocular radiolucency in the right posterior mandible between the inferior alveolar canal and the inferior border of the mandible (Blue arrows).
View Figure 1
The SBC can be difficult to diagnose when the lesion is localized to a different anatomic area of the mandible. Philipsen, et al. described four variants of the SBC based on anatomic location of the mandible. The most common location is the medial surface of the posterior mandible from the first molar to the angle [1,3,4]. An atypical location of the SBC other than the posterior mandible on a panoramic radiograph may present a diagnostic challenge regarding osseous pathology. The incidence of the SBC has been reported to range from 0.1 to 6.06% [7].
This case report describes the presence of the SBC of the bilateral ramus of the mandible during completion of a panoramic radiograph and CBCT in preparation for dental implant surgery [8].
A 40-year-old asymptomatic Caucasian female presented to the office upon referral from her dentist for dental implant consultation. The treatment plan is to replace endodontically fractured and infected tooth #30. The patient's medical history was unremarkable.
Maxillofacial examination was unremarkable. No facial swelling, masses or asymmetry was observed. The TMJ examination was normal. No pain or tenderness to digital palpation was observed in the bilateral preauricular region. Other than tooth #30, the oral examination was negative for soft or hard tissue pathology. The formal dental implant workup included imagining studies consisting of a panoramic radiograph and cone beam CT scan (120 kVp, 5 mA, 7.4 sec). The panoramic radiograph revealed two, well-circumscribed radiolucent areas in the right ramus of the mandible and a unilocular radiolucent lesion in the left ramus of the mandible (Figure 2). Further evaluation utilizing cone beam CT scan imaging (i-CAT FLX, Imaging Sciences, Hatfield, PA) revealed three well-defined unilocular, elliptical shaped radiolucent lesions in the bilateral ramus of the mandible at the level of the sigmoid notch (Figure 3, Figure 4A and Figure 4B). Based on imaging studies, the diagnosis was consistent with Stafne bone cavity of the bilateral ramus of the mandible and not a pathological condition. The patient was informed of the diagnosis and no treatment indicated for this rare anatomic variant of the SBC.
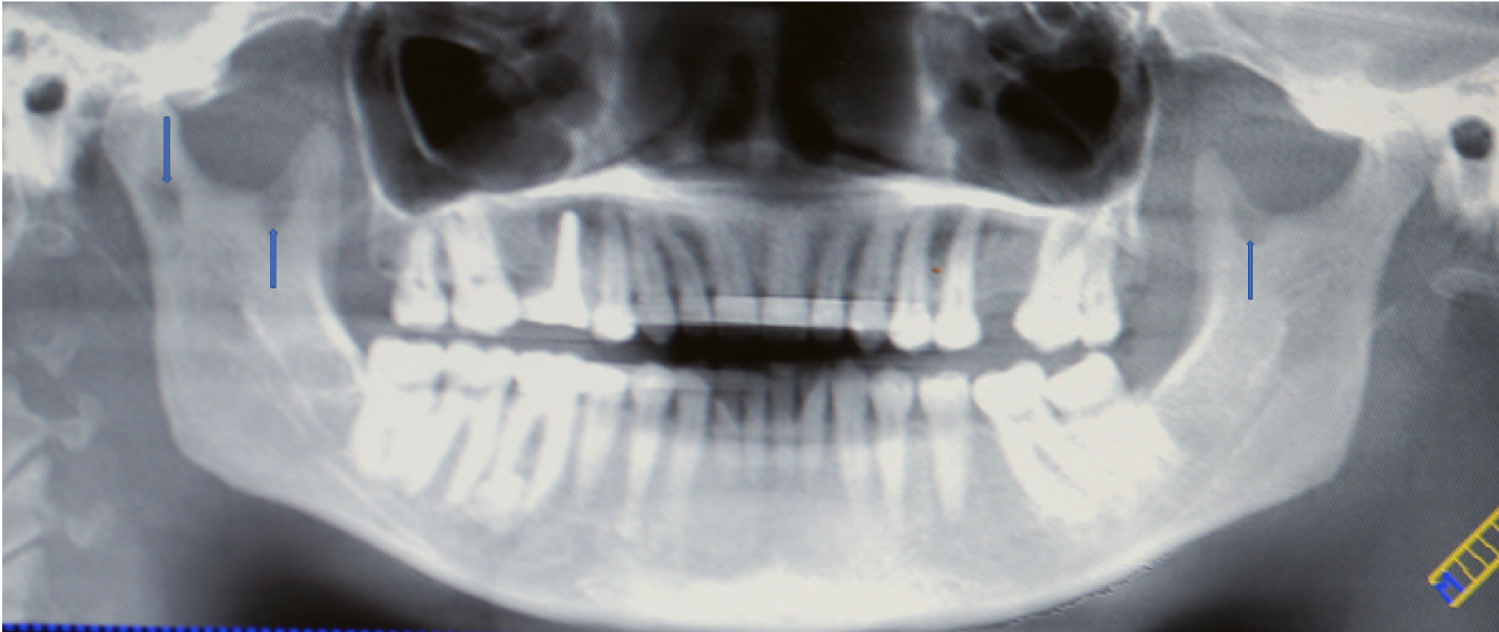 Figure 2: Panoramic radiograph reveals radiolucent lesions in the bilateral ramus of the mandible (Blue arrows).
View Figure 2
Figure 2: Panoramic radiograph reveals radiolucent lesions in the bilateral ramus of the mandible (Blue arrows).
View Figure 2
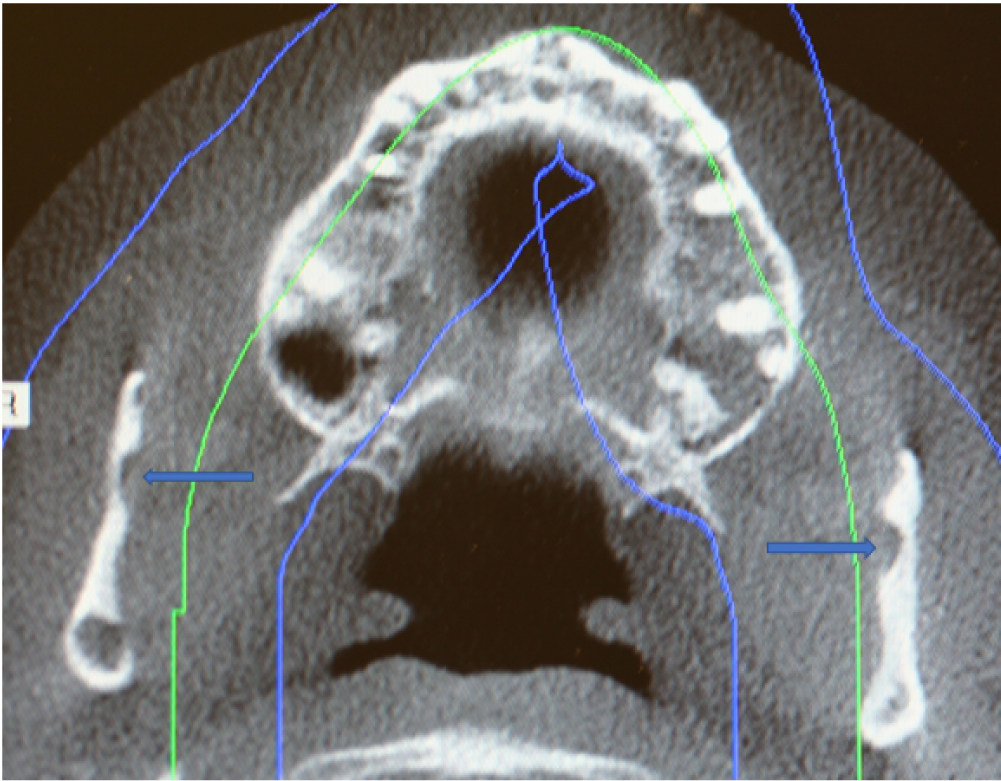 Figure 3: Axial cone beam CT scan showing SBC (Blue arrows) with herniation of soft tissue of the bilateral ramus of the mandible.
View Figure 3
Figure 3: Axial cone beam CT scan showing SBC (Blue arrows) with herniation of soft tissue of the bilateral ramus of the mandible.
View Figure 3
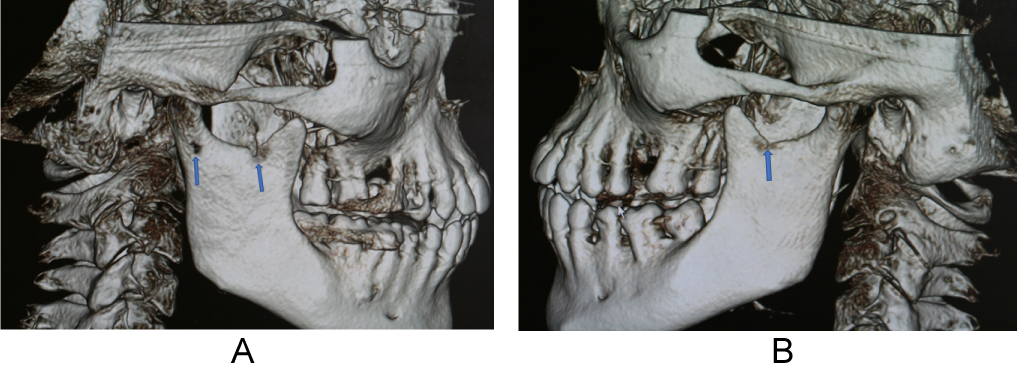 Figure 4: (A) 3D cone beam CT reconstruction images showing two SBC in right ramus (Blue arrows); (B) 3D cone beam CT reconstruction images showing SBC in left ramus (Blue arrow).
View Figure 4
Figure 4: (A) 3D cone beam CT reconstruction images showing two SBC in right ramus (Blue arrows); (B) 3D cone beam CT reconstruction images showing SBC in left ramus (Blue arrow).
View Figure 4
There is a paucity of published case reports of SBC in the subcondylar or ascending ramus of the mandible in the English world medical and dental literature [9-19]. Ertas, et al. [14] described two SBC localized to the right ramus in their case report. An atypical variant in the subcondylar region of the mandible near the parotid gland was first reported by Wolf [9] and later Barker [10]. Both authors described the variant as a "parotid or ramus" variant of the Stafne bone cavity. In 2004, Campos, et al. [11] using cone beam CT scan technology reported a parotid gland variant of the SBC as a salivary gland defect. Using computed tomography Sisman, et al. [3] showed that the SBC is due to the presence of aberrant submandibular gland tissue entrapped within the osseous defect on the medial surface of the mandible. Based on these findings, the authors of this report hypothesize that in our patient parenchymal tissue of the bilateral parotid gland became entrapped in the developing ramus of the mandible that could lead to a similar osseous concavity (Figure 3) [20]. Based on the number of cases reported, SBC localized to the unilateral ramus is considered a rare variant. To the best of our knowledge, there are less than twelve case reports of SBC localized to this area of the mandible. In our reported case, bilateral ramus involvement is even rarer.
Intraosseous radiolucency's in the ramus are rarely observed and diagnosis can be challenging and lead to unnecessary surgery. The differential diagnosis of SBC may include the following: odontogenic cyst, aneurysmal bone cyst, traumatic bone cyst, osteoporotic bone marrow defect, ameloblastoma, myxoma, hemangioma, multiple myeloma, giant cell tumor and metastatic disease [5,21,22]. However, deposition of fat, vascular, and salivary glandular tissue herniated into the osseous concavity should also be considered in the differential diagnosis. Based on the anatomic location and imaging results in our asymptomatic patient, the diagnosis was consistent with a rare variant of the SBC localized to the bilateral ramus of the mandible. No treatment is indicated for this anatomic variant of the SBC. However, when the diagnosis is uncertain, magnetic resonance imaging and biopsy should be considered [3,20,21].
Unilateral Stafne bone cavity (SBC) of the mandibular ramus is a rare clinical entity. Bilateral ramus involvement is even rarer and proved to be a diagnostic challenge in our patient. Knowledge of clinical anatomy and adjunctive 3D imaging studies such as cone beam CT scan helped confirm the diagnosis of SBC in the bilateral ramus of the mandible in our patient.
None declared.