Depending on the time that has elapsed since extraction, the placement of one or more implants in the maxilla or mandible will be determined directly by the clinical and radiographic characteristics of the implant bed. In the case of multirooted teeth, placing an implant immediately after extraction is more complex due to the anatomical sites involved. In the literature, there are very few studies reporting the use of 3D printed surgical guides for the placement of immediate post-extraction single implants. The aim of this article is to describe an alternative technique for guiding the placement of a post-extraction implant and achieve the ideal position using a digitally designed surgical guide. This technique can allow clinicians to obtain a more reliable placement of the implant and thus, a better long-term functional and aesthetic outcome.
Dental Implant, Post-extraction, Surgical Guide, Immediate placement
3D: Three-Dimensional; CBCT: Cone Beam Computed Tomography; STL: Standard Triangle Language; PRF: Platelet-Rich Fibrin
The insertion of dental implants immediately after teeth extractions has become a routine clinical procedure in implant dentistry. Tooth extraction results in a reduction of the bone quantity, which may prevent placement of an implant because of the decreased bone volume. Several studies have reported that successful osseointegration is possible when implants are inserted immediately after tooth extraction, with similar survival rates when compared to implants inserted in healed sites [1]. Regarding the posterior regions of the jaws, the immediate placement of implants can imply a series of clinical difficulties due to the anatomical aspects of the site. The presence of intraseptal bone can facilitate or sometimes interfere with the direction of the drilling. The gaps created between the implant and the socket walls can be disadvantageous if no primary stability is achieved [2]. Taking into consideration all these factors, an exhaustive preoperative plan is a fundamental step for the success of implant dentistry in this type of cases, and different three-dimensional imaging techniques, including CBCT scans and dental scans allow clinicians to collect the necessary data to achieve the proposed goals [3]. With these tools, a complete digital implant workflow can be elaborated.
The ideal functional and cosmetic positions of teeth can now be planned digitally, and the plan used to insert the implants accurately in three dimensions to achieve the desired outcome. Planning begins with the construction of the ideal functional and aesthetic restorative outcome with respect to any remaining teeth and potential implant sites. Implants can then be digitally placed in the optimal locations for functional, biological, and aesthetic requirements [4]. The plans can also help to identify the risk of potential complications such as collateral damage to vital structures or the need for additional grafts. The use of computer-aided implant surgery with digitally designed surgical guides has been advocated to enable accurate placement of implants in the planned locations [5].
The purpose of this study is to present a technique where an implant is immediately placed in a post-extraction socket using a digitally designed surgical guide, allowing for a better surgical, periodontal and prosthetic outcome.
A 29-year-old female patient attended the Oral and Maxillofacial Surgery Unit of University Hospital of Maracaibo, Venezuela, presenting pain in the posterior left mandibular region. Her medical record was unremarkable. On clinical examination, the inferior left first molar (#36) presented with endodontic treatment which had been performed in two previous opportunities due to the persistence of associated pain on vertical and transversal percussion. A panoramic X-ray was requested, and the endodontic treatment with a partially fractured crown was observed in the aforementioned tooth, with no radiolucent images associated (Figure 1). Due to these findings, the final diagnosis of cracked tooth syndrome was decided and thus, the treatment plan chosen was to extract the tooth and place an implant using a surgical guide in the same surgery along with guided bone regeneration. The patient's mandibular cast was scanned using an extraoral scanner (Ceramill Map 300, Amann Girrbach, Austria) (Figure 2) and the STL file was obtained and edited in order to eliminate the crown of the tooth using MeshMixer program (Autodesk, Canada) (Figure 3). The edited denture scan was aligned to the mandibular CBCT scan of the patient in Blue Sky Plan (Blue Sky Bio, USA) to allow for prosthetically driven implant planning. Implant placement simulation was carried out in the software aiming for the site with the most surrounding bone while being prosthetically acceptable (Figure 4) and a surgical guide was designed and printed in a desktop 3D printer (AnyCubic Photon, China) (Figure 5 and Figure 6). Under moderate sedation and local anesthesia, the molar was a traumatically extracted, the surgical guide was held in position (Figure 7) and a 4.0 × 13 mm IS II active implant (NeoBiotech, Korea) was placed using the NeoBiotech Naviguide system. Subsequently, the alveolar gaps were filled using cortico-cancellous bone allograft (Ossogen, Lattice Biologics, USA) (Figure 8) and two Platelet-Rich Fibrin (PRF) membranes made using the protocol described by Choukroun [6] (Figure 9). Simple sutures using 3-0 polyglactin 910 (Vicryl, Ethicon, USA) were used for closure.
 Figure 1: Preoperative panoramic x-ray.
View Figure 1
Figure 1: Preoperative panoramic x-ray.
View Figure 1
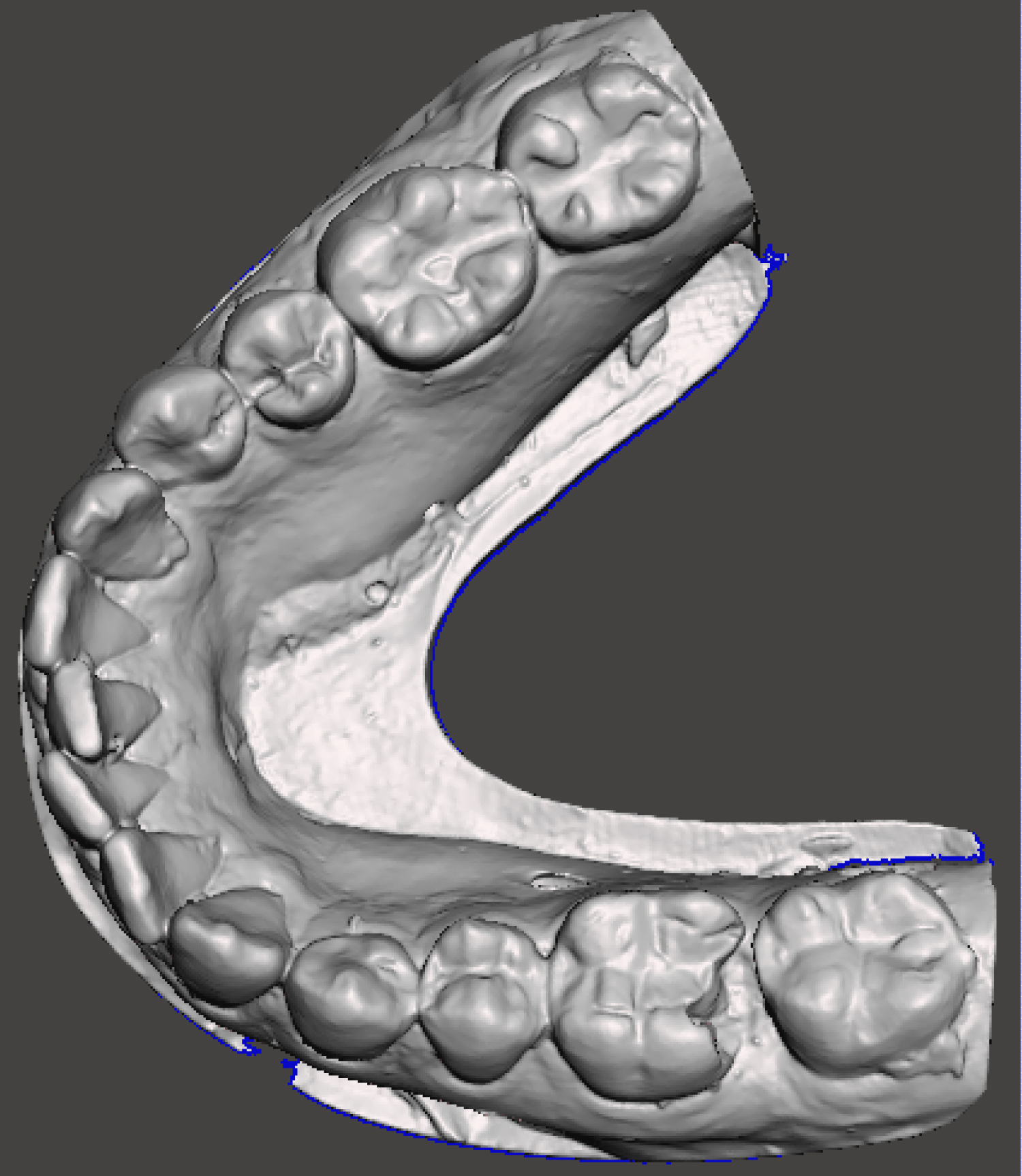 Figure 2: Unedited digital cast of the patient.
View Figure 2
Figure 2: Unedited digital cast of the patient.
View Figure 2
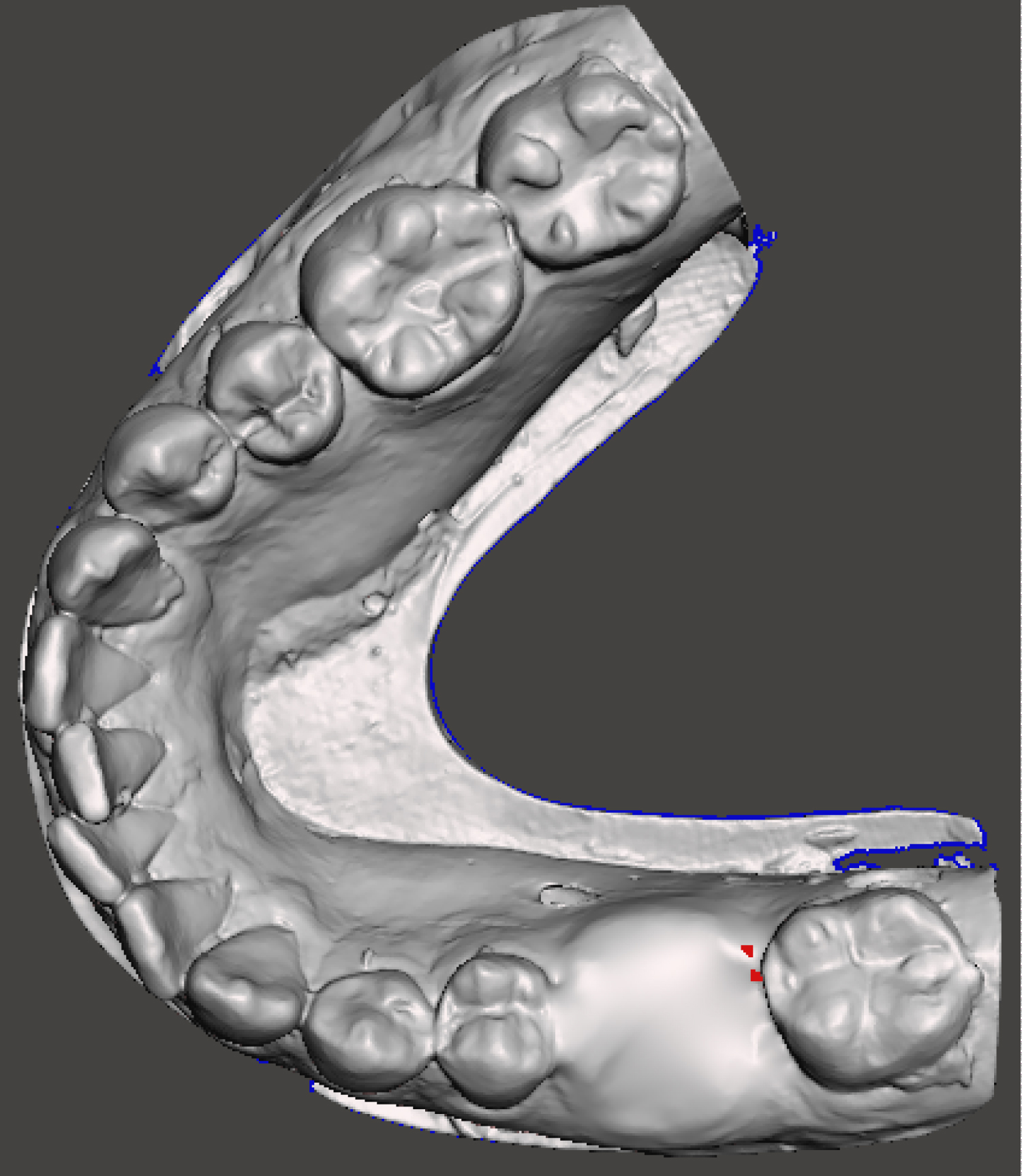 Figure 3: Digital cast of the patient after editing out the crown of the tooth to be extracted.
View Figure 3
Figure 3: Digital cast of the patient after editing out the crown of the tooth to be extracted.
View Figure 3
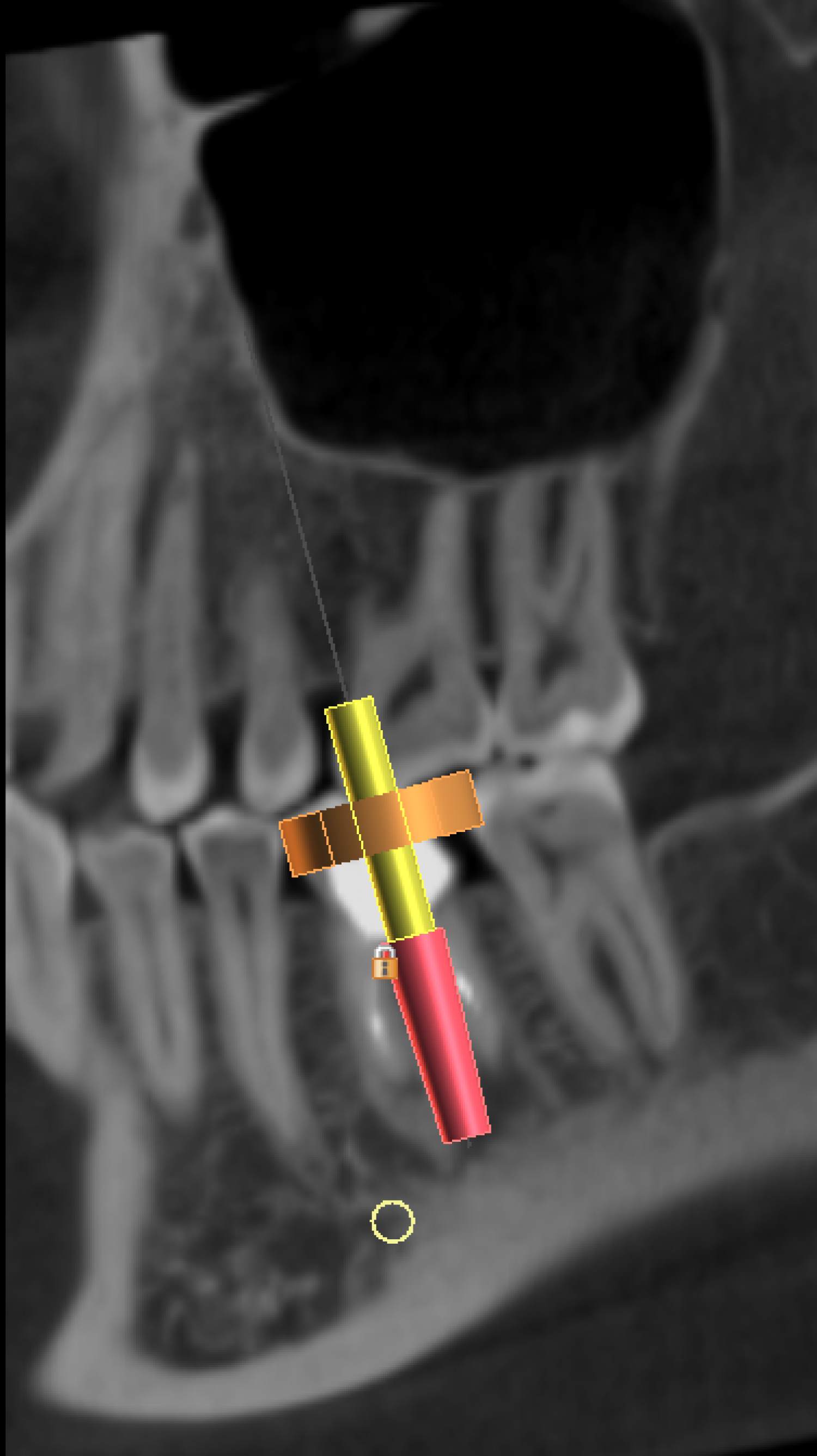 Figure 4: Three-dimensional positioning of the implant, achieving good prosthetic and anatomical outcomes.
View Figure 4
Figure 4: Three-dimensional positioning of the implant, achieving good prosthetic and anatomical outcomes.
View Figure 4
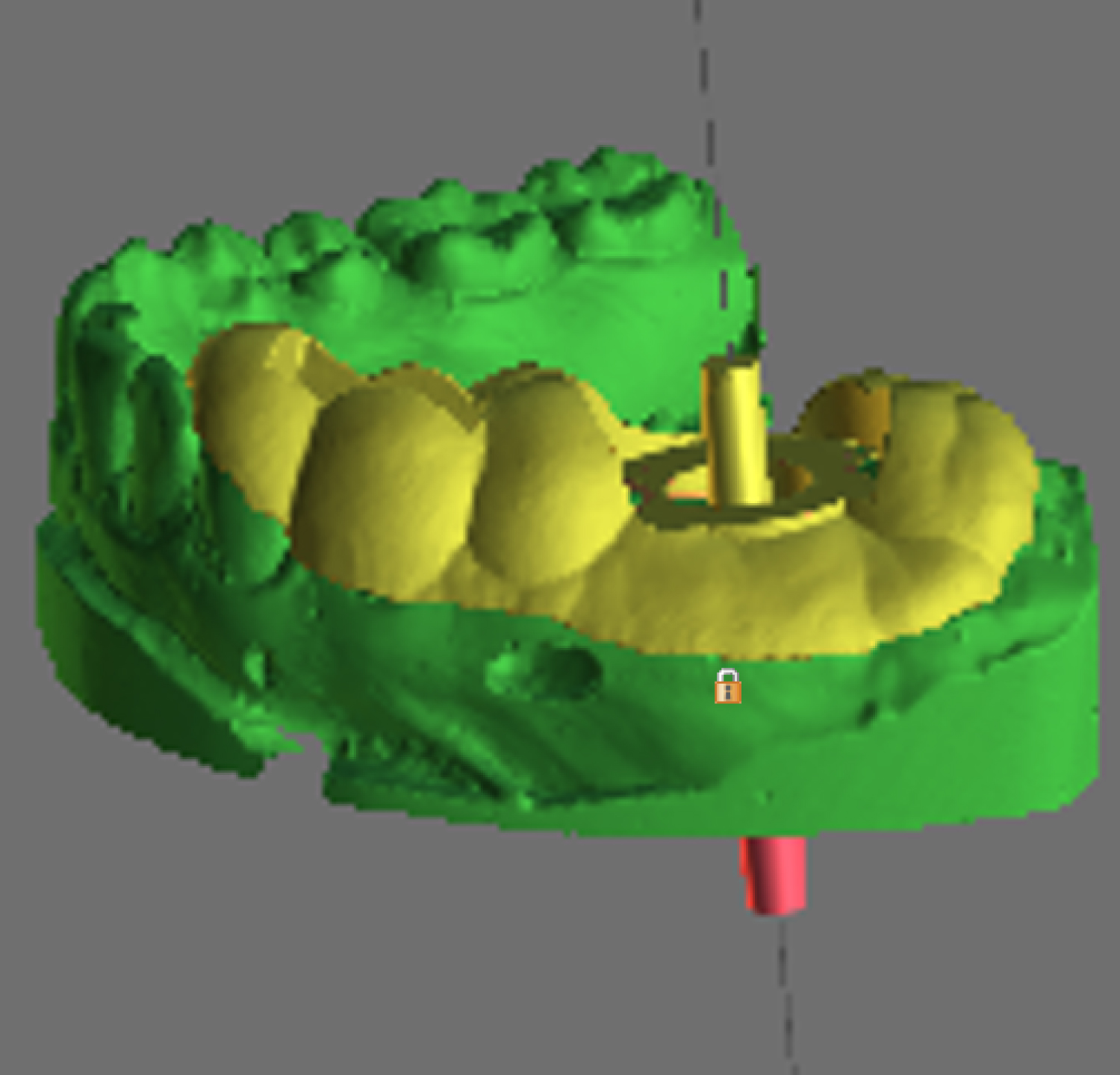 Figure 5: Digital design of the surgical guide.
View Figure 5
Figure 5: Digital design of the surgical guide.
View Figure 5
 Figure 6: Digitally designed surgical guide placed on the patient's conventional cast.
View Figure 6
Figure 6: Digitally designed surgical guide placed on the patient's conventional cast.
View Figure 6
 Figure 7: Surgical guide accurately fitting intraorally after the extraction.
View Figure 7
Figure 7: Surgical guide accurately fitting intraorally after the extraction.
View Figure 7
 Figure 8: Use of cortico-cancellous bone allograft to fill the gaps of the socket.
View Figure 8
Figure 8: Use of cortico-cancellous bone allograft to fill the gaps of the socket.
View Figure 8
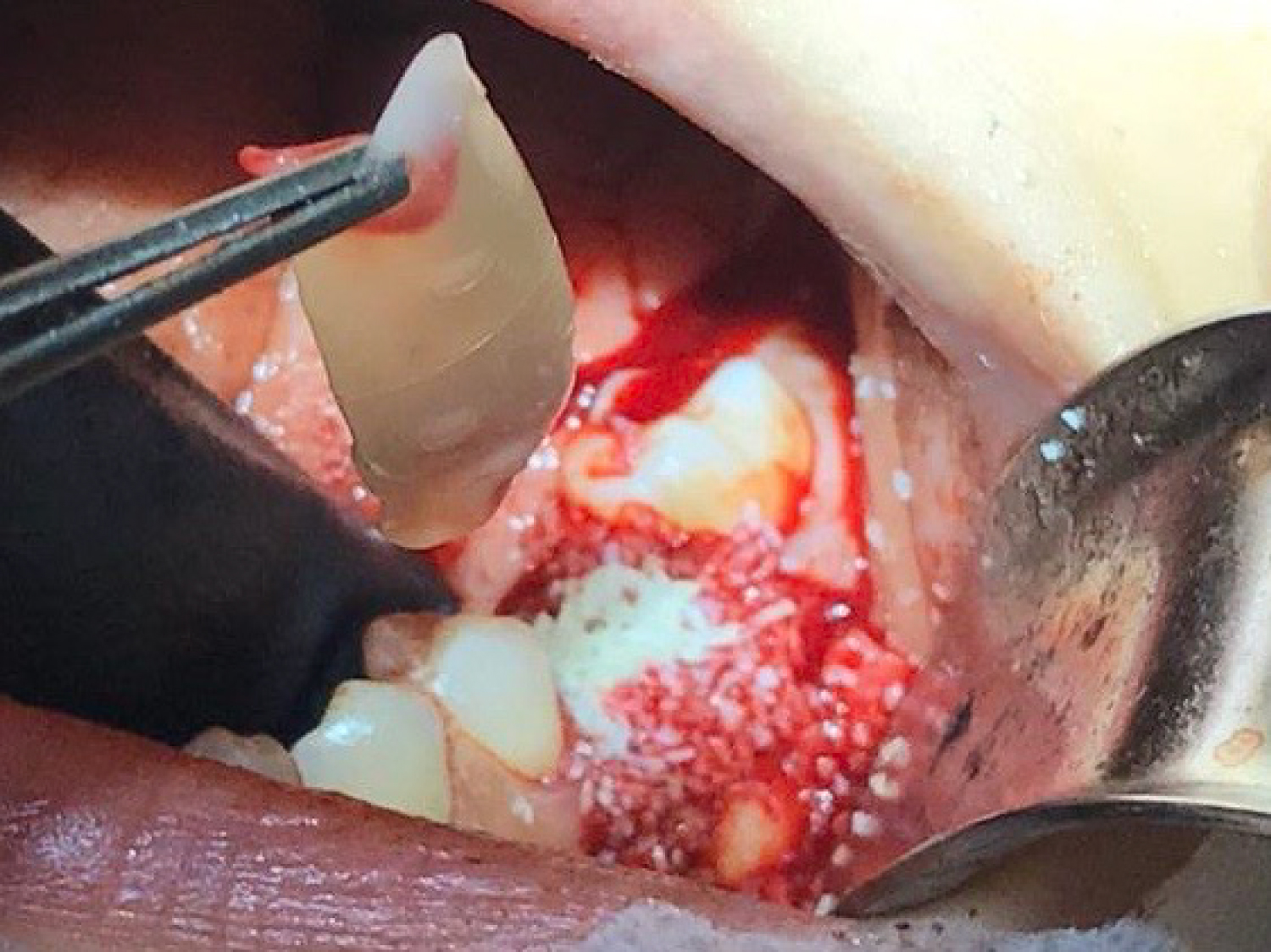 Figure 9: Use of PRF membranes on top of the bone graft.
View Figure 9
Figure 9: Use of PRF membranes on top of the bone graft.
View Figure 9
In the seventh postoperative day, the patient referred an uneventful course, with minimal pain and swelling. A panoramic X-ray was obtained where the correct placement, angulation and depth of the implant could be observed (Figure 10).
 Figure 10: Postoperative panoramic x-ray showing the correct position of the implant after 7 days.
View Figure 10
Figure 10: Postoperative panoramic x-ray showing the correct position of the implant after 7 days.
View Figure 10
The question whether immediate implants are more at risk for failure than implants placed in mature bone has received increasing attention in the previous years. At the beginning of the century, a review of immediate placement of single-tooth implants by Vignoletti and Sanz [7] concluded that immediate placement, even with grafting procedures, is still not fully validated with no clear evidence of consistent clinical outcomes. These authors also mention some important factors that must be taken into account in order to achieve a successful outcome when placing immediate implants, including: 1) Substantial thickness and integrity of socket walls; 2) Adequate vertical and horizontal position of the implant; 3) Gingival thickness and integrity and 4) Patient factors such as hygiene and smoking. One of the biggest issues when placing an implant in a fresh socket is the potential lack of surrounding bone. A systematic review and meta-analysis conducted in 2015 comparing implant placement in fresh extraction sockets versus healed sites concluded that the insertion of dental implants in fresh extraction sockets affects the implant failure rates. However, it does not affect the marginal bone loss or the occurrence of postoperative infection [1]. A more recent study also concluded that defective buccal walls in extraction sockets might reduce the success rate of immediate implant placement [8]. It is known that part of the blood supply of the facial plate of the socket comes from the periodontal ligament, thus, facial plates that are 1 mm or less can be expected to resorb away necessitating some type of grafting. Allografts are considered a good material to place in the socket gap to avoid late-term resorption [9,10]. More so, numerous studies have been conducted in which PRF has been used at different sites including implants, extraction sockets, and bone grafts, concluding that PRF helps accelerate and improve healing [11].
In order to overcome these issues and achieve better long-term results, different technologies have been developed for the placement of implants. One of the most globally accepted methods is the use of digitally designed surgical guides. To ensure an adequate and predictable long-term outcome, modern implant treatment requires prosthodontically driven, systematic 3-dimensional assessment and planning. Digital dental workflows can optimize the process, providing valuable diagnostic information and facilitating backward planning to improve safety and efficiency, which contribute to a more predictable outcome. Several systematic reviews have reported that static surgical guides reproduce the digitally planned position of the implant with adequate levels of accuracy [5]. Guided surgery is generally performed quicker; it also allows improvement in the aesthetic results and satisfaction of the patient and compared with conventional placement, the incidence of bacteremia is considerably lower [12-14].
Despite of all this evidence, there appears to be no literature related to the use of surgical guides for the immediate placement of single-tooth post-extraction implants. Therefore, this study pretends to describe a technique where this can be achieved in a successful manner. It is of worth mentioning that the conclusions hereby made should be taken with caution due to the limited number of studies related to this specific technique. By following the described protocol, we conclude that a shorter, more reliable and more conservative surgery can be performed, improving the postoperative results, and allowing for a better prosthodontic predictability.
This study was approved by the University Hospital of Maracaibo IRB.
Patient's consent for publication was acquired.
The authors declare that they have no competing interests.
No funding was received.
Not applicable.