Lymphangiomas are benign hamartomatous tumors which are characterized by abnormal proliferation of lymphatic vessels. They are lymphatic malformations which are localized to head and neck region. They are rare located in the oral cavity. Tounge, lips, buccal mucosa, soft palate and floor of the mouth are affected in the oral cavity. However buccal mucosa is infrequent in litarature. In this report report, a rare case of lymphangioma of the left buccal mucosa of retromlar area in a 30-year-old female patient has been treated by surgical excision is presented.
Lymphangioma, Buccal mucosa, Lymphatic vessels
Lymphangioma is a benign hamartomatous tumor caused by congenital malformation of lymphatic system. Lymphangiomas are usually present at birth, and aproximately 80% cases are present by age of 2 years. They are commonly found head and neck region. The most common area of head and neck reigon is the submandibular region and also parotid gland [1]. The oral cavity can be affected by these lesions. They usually seen at the anterior two thirds of tounge followed by palate, gingiva, lips, alveoler ridge of mandibule and rarely buccal mucosa [2]. Various treatment modalities have been used for the cure of lymphangioma. Surgical excision, radiotion, laser therapy, and sclerotherapy can be used for the treatment of lymphangioma [3] . In this report, a rare case of lymphangioma of the left buccal mucosa of retromolar area in a 30-year-old female patient has been treated by surgical excision is presented.
A 30-year-old woman was referred to the Department of Oral Maxilofacial Surgery with a chief complaint of growth and blisters on buccal mucosa of mandibular left retromolar region of and halitosis. Patient also complains discomfort during feeding. There is no systemic disease in the medical history of patient.
On intraoral examination, discolorization was seen in left buccal mucosa of retromolar region. The lesion was exophtic with color ranging from reddish purple to yellow was seen (Figure 1). On palpation, the lesion soft and nontender. Diascopy test was carried out which was negative. There was no evidence of adjacent bone and tooth involvement on orthopanthomographic examination. On the basis of history and clinical features a provisional diagnosis of lymphangioma was made and an excisional biopsy under local anaesthesia was planned. The lesion was excised by surgical (Figure 2) and wound was sutured primary (Figure 3). The excised lesion (Figure 4) was sent for histopatholigical examination and diagnosed as lymphangioma. Microscopic examination showed numerous dilated lymphatics lined by endothelium (Figure 5) Some of the section revealed the precense of chanells filled with red blood cells (Figure 6). There were also many of accumulation of lymphocytes. .The patient was discharged after 6 months (Figure 7) and 1 year with normal looking buccal mucosa . There was no evidence of recurrence of the lesion on follow up of 1 year.
 Figure 1: The view of lesion that is located in buccal mucosa left retromolar region.
View Figure 1
Figure 1: The view of lesion that is located in buccal mucosa left retromolar region.
View Figure 1
 Figure 2: The view of buccal mucosa after excision of the lesion.
View Figure 2
Figure 2: The view of buccal mucosa after excision of the lesion.
View Figure 2
 Figure 3: Closure of the wound.
View Figure 3
Figure 3: Closure of the wound.
View Figure 3
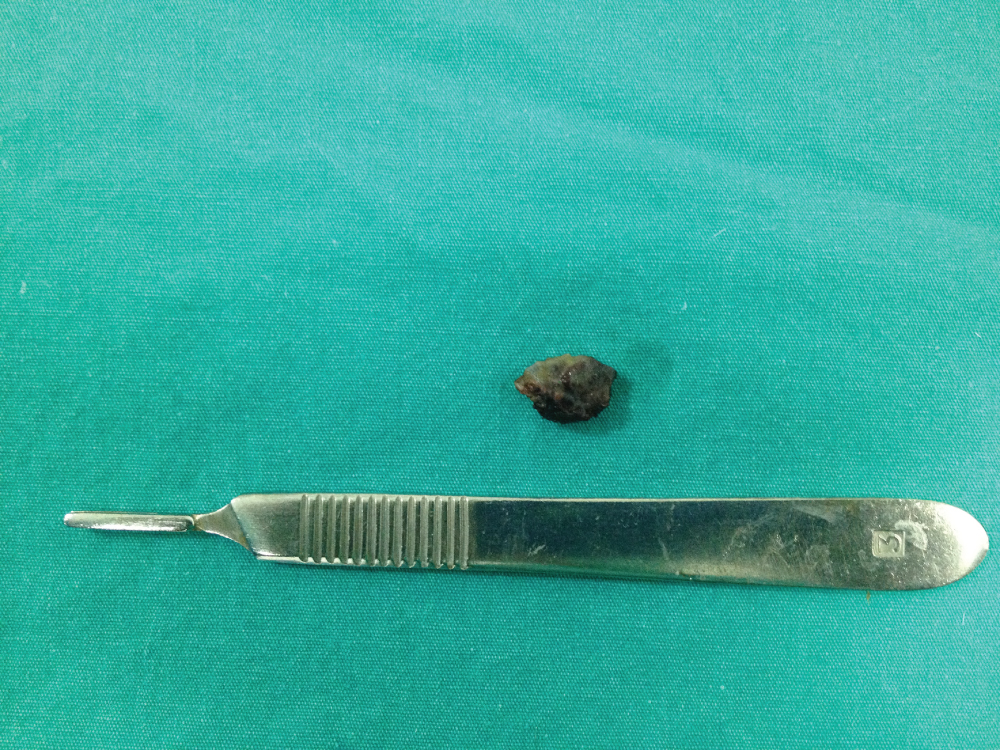 Figure 4: Excised surgical specimen.
View Figure 4
Figure 4: Excised surgical specimen.
View Figure 4
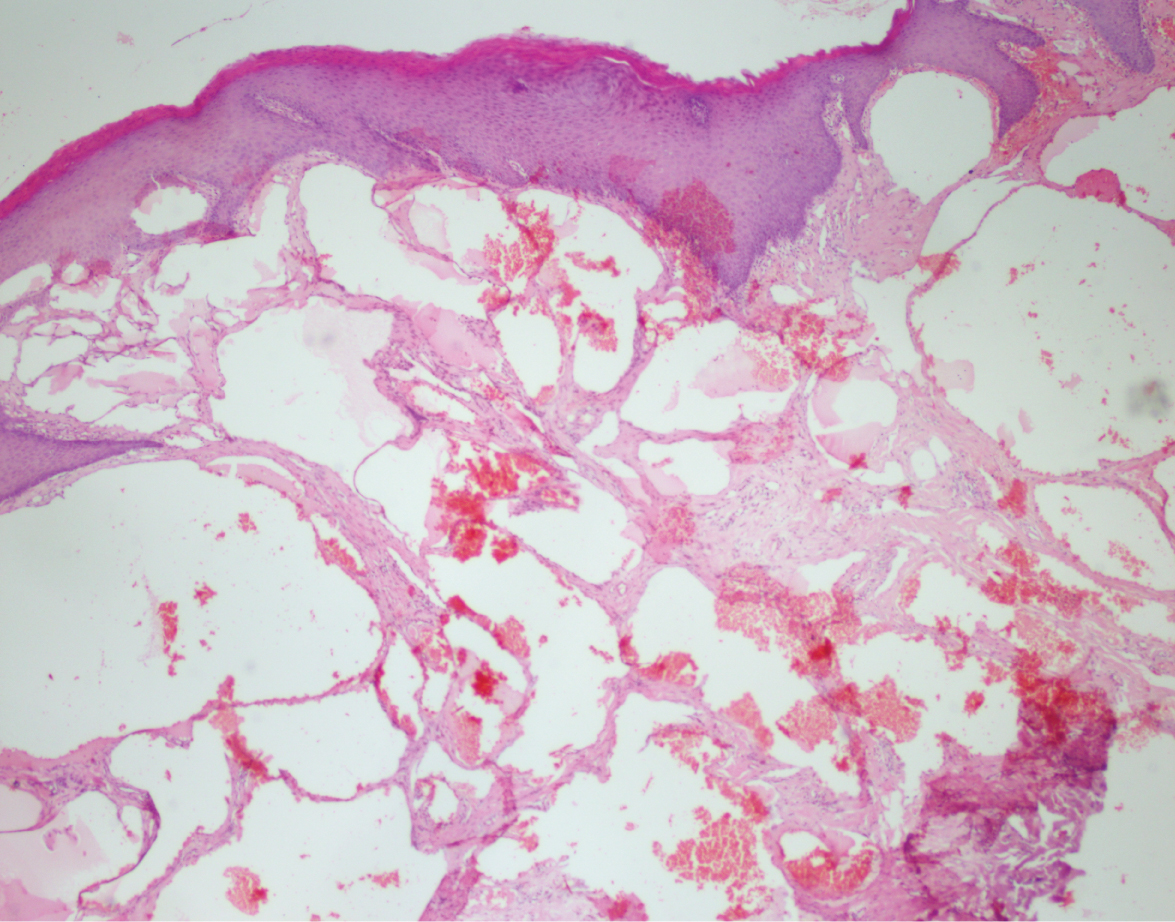 Figure 5: Numerous dilated lymphatics.
View Figure 5
Figure 5: Numerous dilated lymphatics.
View Figure 5
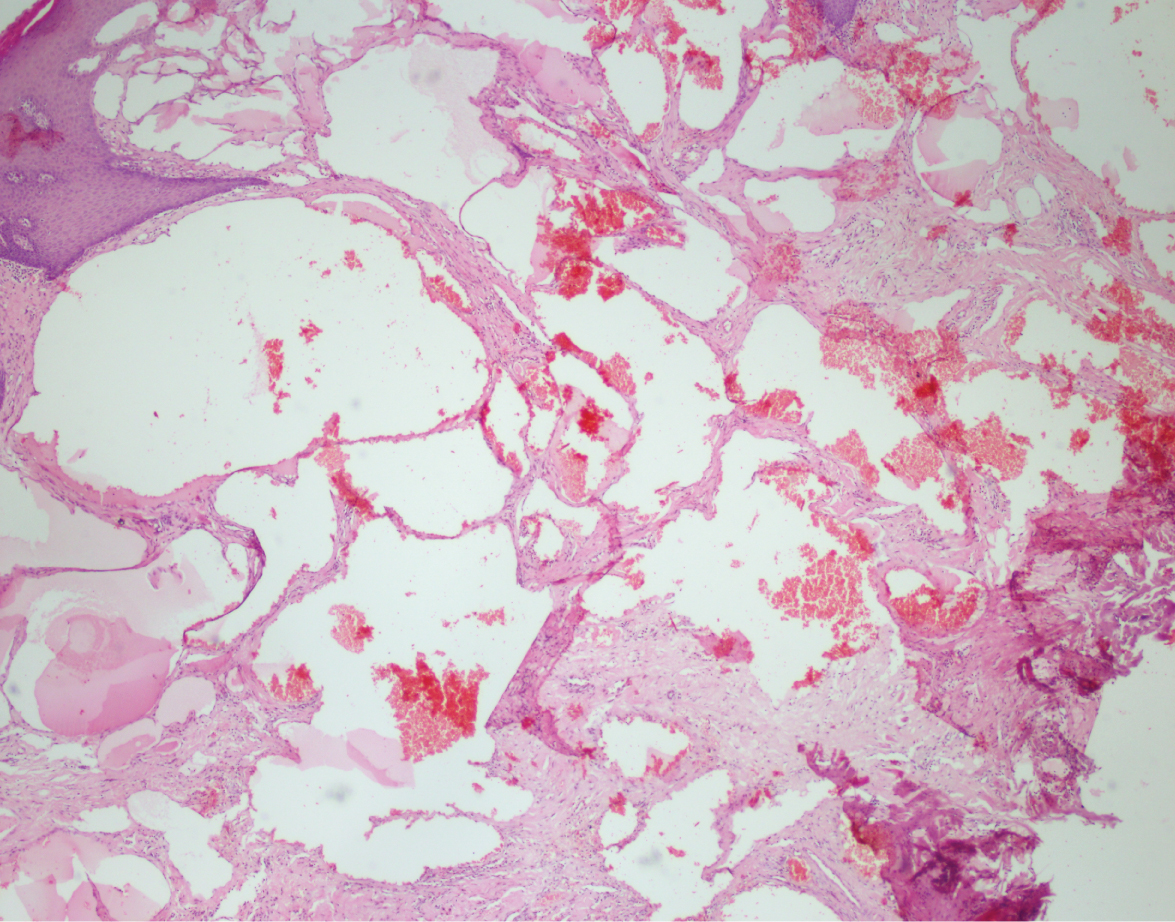 Figure 6: Some of the section revealed the precense of chanells filled with red blood cells.
View Figure 6
Figure 6: Some of the section revealed the precense of chanells filled with red blood cells.
View Figure 6
 Figure 7: A 6-month follow-up.
View Figure 7
Figure 7: A 6-month follow-up.
View Figure 7
Lymphangioma is congenital vascular abnormality of the lymphatic system which is rare bening lesion. Lymphangioma was first defined by Virchow in 1854 [3]. Several theories have been proposed for pathogenesis of lymphangioma. The first theory is that lymphatic system developes from five primitive sac arising from the venous system. Concerning the head and neck, endothelial outpouching from the jugular sac spread centrifugally to form the lymphatic system. Another theory proposes that the lymphatic system develops from mesenchymal clefts in the venous plexus reticulum and spread centripetally towards the jugular sac. Lastly, lymphangioma develops from congenital obstruction or sequestration of primitive lymphatic enlargement [4]. These lesions are frequently reported at birth (60%) and 90% grow by 2 years of age. Lymphangioma is rare present in adults [5]. In this case, a 30-year-old female reported.
De Serres, et al. offered a clasification of the lymphangioma of head and neck based on of the spread the anatomical involvement [6].
• Stage/Class I: Infrahyoid unilateral lesions
• Stage/Class II: Suprahyoid unilateral lesions
• Stage/Class III: Suprahyoid and infrahyoid unilateral lesions
• Stage/Class IV: Suprahyoid bilateral lesions
• Stage/Class V: Suprahyoid and infrahyoid bilateral lesions
Lymphangiomas, aproximately 75% cases, are located in head and neck region. The oral cavity is rarely affected site including tounge, lips, buccal mucosa, hard and soft palate, gingiva [4]. Tounge is commonly affected by the lymphangioma in the oral cavity. Brennan, et al. reported 49 cases of oral lymphangioma and 17 cases were located in tongue while only one case was placed at retromolar region and one at soft palate [7]. Buccal mucosal lesions of lymphangioma are exactly uncommon in the litarature [8].
Clinically, lymphangiomas are divided into three types which are microcystic, macrocystic and mix. Macrocystic lesions are larger than 2 cm, whereas microcystic lesions are less than 2 cm.
Mix type is combining of microcystic and macrocystic types [9,10]. Morphologically, oral lymphangiomas are fairly typical. The superfacial types manifest a pebbly surface and vesicle-like feature with so called ‘frog egg’ apperance and gradually enlarge. The deep lesions usually present as submucosal mass.
Histopatologically lymphangiomas are classified as: [11,12].
• Lymphangioma simplex (composed of small thin-walled lymphatics)
• Cavernous lymphangioma (comprised of dilated lymphatics vessels with surrounding adventitia)
• Cystic lymphangioma (consisting of huge, macroscopic lymphatic spaces surrounded by fibrovascular tissue, and smooth muscle)
• Benign lymphangioendothelioma (lymphatic channels appears to be dissecting through dense collagenic bundles).
Treatment of lymphangioma alter their type, size, involvement anatomical structures and infiltration to surrounding tissues. Microcystic lesions are diffuse and difficult to remove in contrast macrocystic lesions are localized and easily excised. Various methots can be tried the treatment of lymphangiomas. Such as laser therapy, cryotherapy, surgical excision, sclerotherapy, electrocautery [3,13,14].
Oral lymphangiomas are common lesions occuring at the tounge and rarely at the buccal mucosa of retromolar region. Localized lesions can be treated by conservative surgcal excision with less recürrence rate. Therefore, the correct diagnosis and therapeutic indication of this type of lesions is crucial.