Antenatal care is the care given to pregnant women and adolescent girls by trained healthcare professionals. In 2017, almost 295,000 women lost their lives during, immediately after, or soon after childbirth in Ethiopia. The time of the first antenatal visit must be determined in order to enhance the health of pregnant women and their infants. The most recent Demographic and Health Survey (DHS) survey datasets from 2019 are used in this study. It will considerably hasten the nation's advancement toward Sustainable Development Goals and cut the rate of maternal mortality.
The aim of the study was to predict the factors that affect the time to the first ANC visit in Ethiopia. The 2019 EDHS served as the source of the study's data, which included information on 3938 pregnant women in the 15- to 49-year-old age range who had survived five years of the survey. The AFT and gamma-shared frailty models with Weibull, log-normal, and log-logistic baseline distributions were used to determine which model fit the date of the first ANC visit and its influencing factors the best. AIC and BIC were used to evaluate all fitted models.
The median time of the first ANC visit was 4 months. The log-logistic with Gamma shared frailty model is an appropriate model when compared with other models for a time at first ANC visit dataset based on AIC and BIC. The clustering effect was significant for modeling the determinants of the time-to-first ANC visit dataset. The final model showed that place of residence, women's education level, religion, wealth index, and sex of household head were found to be significant determinants of time at first ANC visit at a 5% level of significance.
The time at first ANC visit data set was best described by the log-logistic with gamma shared frailty model than by other models, and there was heterogeneity between the regions at the time of the first ANC initiation. Targeting women with lower socioeconomic status is important, as is providing them with access to formal education as a path to early time at their initial ANC visit.
ANC: Antenatal Care; AFT: Accelerated Failure Time; AIC: Akaike's Information Criteria; BIC: Bayesian Information Criteria; EDHS: Ethiopia Demographic and Health Survey; PH: Proportional Hazard; WHO: World Health Organization
To promote the greatest possible health outcomes for both mother and child during pregnancy, antenatal care (ANC) is the care given to pregnant women and adolescent girls by trained health-care professionals [1]. In 2017, almost 295,000 women lost their lives during, immediately after, or soon after childbirth. The vast majority of these deaths (94%) happened in areas with little resources, and the bulk of them could have been prevented [2].
Through the utilization of ANC, it is possible to identify and treat pregnancy-related complications as well as give preventative healthcare services including tetanus immunizations, malaria and worm treatments, HIV testing and counseling that leads to the Prevention of Mother to Child HIV Transmission (PMTCT) [1,3,4].
Women who begin ANC attendance early and maintain regular attendance are more likely to deliver their babies under the supervision of a skilled birth attendant than those who start ANC late and attend few visits [5-7]. Ethiopia's maternal mortality ratio, which was 353 per 100,000 live births in 2015 [8]. Nevertheless, it is still among the highest. Obstetric problems during pregnancy and childbirth are the main causes of death for women in their reproductive years in developing nations like Ethiopia [8].
The timing of the first ANC visit has been linked to a number of factors in the research. They include participation in the educational status [9-12], wealth status [13,14] parity [15,16], place of residence [12,17], maternal age [18], marital status [19]. A study conducted in Nigeria revealed that women living in urban areas start ANC visit earlier than their contemporaries in rural areas [20]. A study conducted among pregnant women in Nigeria and Uganda find out that women with higher educational level were more likely to start their first ANC visits at earlier gestational age relative uneducated [20,21]. Additionally, studies revealed that different religious groups had a distinct first ANC visit timing. It was found that Christian women were more likely than Muslim women to begin ANC earlier [20].
Hence, this study aims to investigate the possible characteristics influencing time to first ANC visit Ethiopia using the most recent Demographic and Health Survey (DHS) survey datasets conducted in 2019. The time of the first antenatal care visit among pregnant women and the factors that influence the start of the first ANC visit must be determined in order to improve maternal and child health. The purpose of this study is to examine factors that affect the timing of the first prenatal care visit among pregnant women. This study uses non-parametric, semi-parametric and parametric with (weibull, exponential, log-normal and log-logistic) gamma and inverse Gaussian shared frailty model in determining the factors which affect the time-to-first ANC visit and AFT to compare and get the best model which fits the time-to first ANC visit data appropriately by using AIC and BIC. By utilizing the most recent EDHS data to reveal new information on specific obstacles to the prompt timing of ANC for pregnant women, the study's findings may help to improve the health status of mothers in the nation as a whole. As a result, it will significantly contribute to lowering the rate of maternal mortality and accelerating the nation's progress toward the Sustainable Development Goals and the Health Sector Transformation Plan, where both the international community and the Ethiopian government place a high priority on maternal and newborn health.
The 2019 Ethiopia Mini Demographic and Health Survey (2019 EMDHS) was implemented by the Ethiopian Public Health Institute (EPHI), in partnership with the Central Statistical Agency (CSA) and the Federal Ministry of Health (FMOH), under the overall guidance of the Technical Working Group (TWG). Data collection lasted from March to June 2019. The sampling frame used for the 2019 EMDHS is a frame of all census enumeration areas (EAs) created for the 2019 Ethiopia Population and Housing Census (EPHC) and conducted by the Central Statistical Agency (CSA). The census frame is a complete list of the 149,093 EAs created for the 2019 EPHC. An EA is a geographic area covering an average of 131 households. The sampling frame contains information about EA location, type of residence (urban or rural), and estimated number of residential households. Administratively, Ethiopia is divided into nine geographical regions and two administrative cities. The sample for the 2019 EMDHS was designed to provide estimates of key indicators for the country as a whole, for urban and rural areas separately, and for each of the nine regions and the two administrative cities [22].
For this study, we have used the kids' data set and the study population was women (aged 15 to 49 years) who gave birth five years preceding the survey and attended antenatal care during their last pregnancy.
Pregnant women of age 15-49 years and whose gestational age (duration of pregnancy in weeks) was known whether they access or not for ANC visit at least once throughout pregnancy were included in the study. However, women who had ANC visit but their gestational at ANC visits was unknown (unrecorded) were excluded from this study.
The number of months between conception and the first prenatal care visit is an outcome of interest (event). Those who skipped ANC appointments throughout their pregnancies, regardless of the pregnancy's outcome, were regarded as non-attendees (censored).
The independent variables were selected based on a literature review as being factors associated with the timing of the first ANC visit and includes women's age, marital status, education level of the women, wealth index, residence, religion, sex of household head and parity.
The data were analyzed using stata version 14. Descriptive statistics and weighted percentage were used to display the distribution of ANC booked women by their characteristics. Kaplan-Meier estimation method, Cox proportional hazard model and parametric shared frailty model were used to analysis survival time to first ANC visit. Study subjects came from clustered community and hence clustered survival data correlated at the regional level. Parametric frailty models explored assuming that women with in the same cluster (region for this study) shares similar risk factors. We used Weibull, Exponential, Log logistics and Log normal distributions and based on AIC criteria, all models were compared for their performance. The lognormal inverse Gaussian model has the minimum AIC value among the models compared.
Table 1's descriptive summary of variables reveals that a total of 3,938 pregnant women from nine regions and two administrative cities were included in this study, of whom 2,894 (73.5%) had their first ANC visit (events) whereas 1,044 (26.5%) had their first ANC visit missed (right censored). The highest percentage of pregnant women in the research, 344 (11.9%), came from Oromia, and the lowest percentage, 86 (3%), came from Somalia. However, 2,044 (51.9%) of the women were uneducated. On the residence of pregnant women, 2,951 (74.9%) were from a rural setting, the 2,010 (98.3%) had ANC visits. The majority of pregnant women in terms of wealth were the poorest 1,183 (30%), followed by the richest 960 (24.4), and of these, 591 (15%) and 63 (1.6%), respectively, did not receive an ANC visit.
Table 1: Socio-demographic and obstetric characteristics of pregnant women in Ethiopia, EDHS 2019. View Table 1
The kaplan-meier estimate of time-to-first ANC visit: The survival time-to-first ANC visit of pregnant women in Ethiopia is visualized using non-parametric survival analysis (K-M) under various variables. Additionally, it offers details on how the survival and hazard functions of the ANC data set are shaped. Figure 1's survival curve showed an initial abrupt reduction followed by a more gradual decline. This suggests that the likelihood of skipping an ANC check increases early in pregnancy and tends to significantly decline as gestational age increases. Additionally, in Ethiopia, the median gestational period for the first ANC visit was the fourth month.
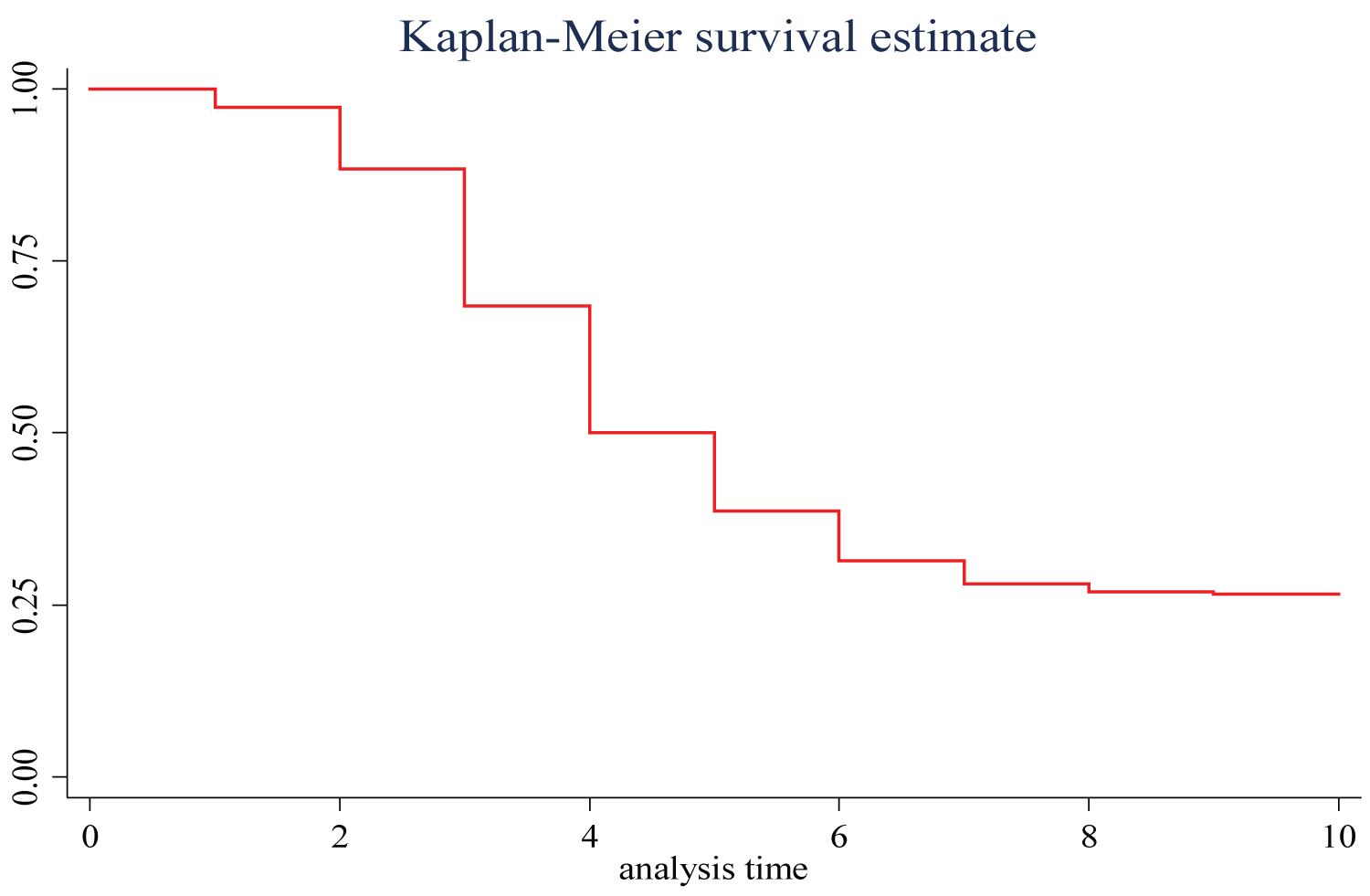 Figure 1: The K-M plots of survival function of time to first ANC visit among pregnant mothers in Ethiopia, 2019.
View Figure 1
Figure 1: The K-M plots of survival function of time to first ANC visit among pregnant mothers in Ethiopia, 2019.
View Figure 1
Comparison of residency based on survival time to first ANC visit: The waiting period before a pregnant woman's first ANC visit is shown using Kaplan Meier graphs for various variables. Figure 2 demonstrates that pregnant women from rural areas started their initial ANC visits later than those from urban areas, or that their chances of not commencing ANC visits were higher across gestational age. Additionally, for inhabitants of urban and rural areas, the median time after the first ANC visit was the third and fifth months, respectively.
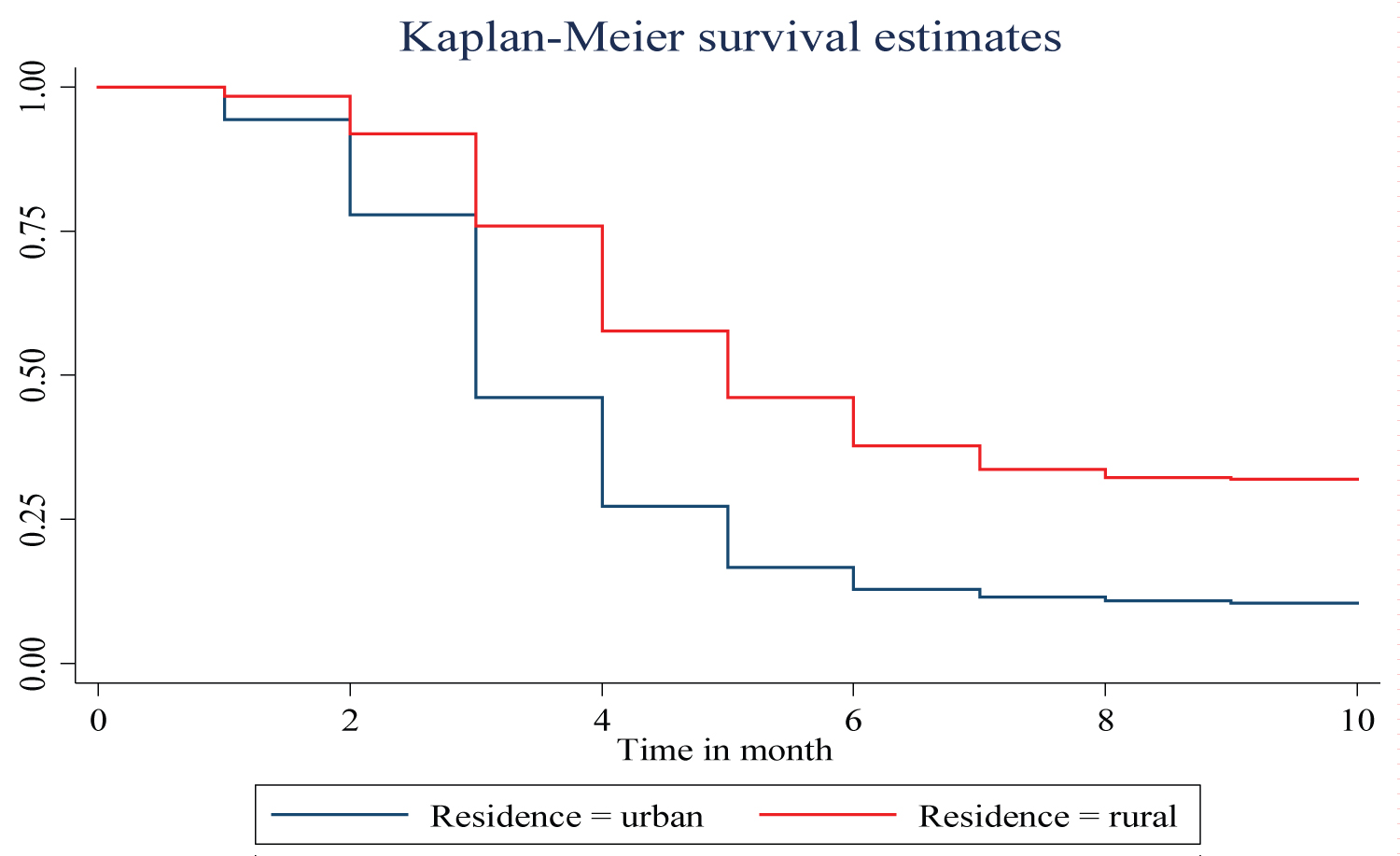 Figure 2: Survival time to first ANC visit among pregnant women by place of residence.
View Figure 2
Figure 2: Survival time to first ANC visit among pregnant women by place of residence.
View Figure 2
Comparison of 'survival' time to first ANC visit by women educational status: Figure 3 illustrates waiting time-to-first ANC visit. The graph shows there are differences in waiting time at first ANC visit for different categories of educational status. Women who attended primary, secondary, higher education started ANC visit earlier than women who did not attend education. The median survival time of women who had no education, attended primary, secondary and higher education were 6, 4, 3 and 3 month respectively. Furthermore, the result of log-rank from Table 2 shows there is a statistically significant difference in survival time of first ANC visit among the educational levels (p-value < 0.001).
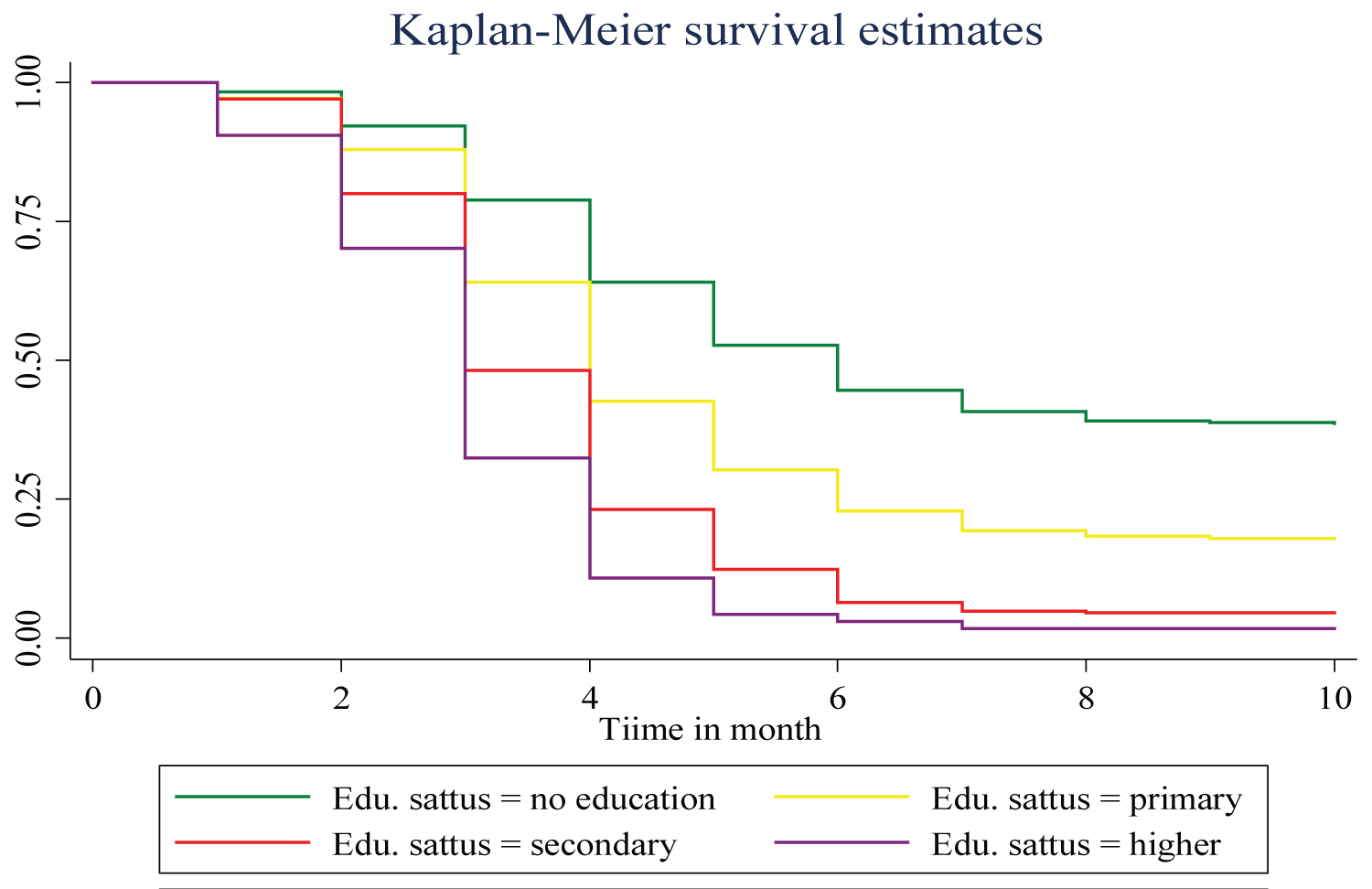 Figure 3: Survival time to first ANC visit among pregnant women by educational status.
View Figure 3
Figure 3: Survival time to first ANC visit among pregnant women by educational status.
View Figure 3
Table 2: Comparison of survival time, for first antenatal care visit (in months) among pregnant women in Ethiopia EDHS, 2019. View Table 2
Comparison of survival time to first ANC visit by wealth index: K-M plot used to compare the survival time to first ANC visit for pregnant women in different wealth index. Thus, it was found women in the poorest wealth index household received first ANC later than poorer, middle, richer and richest wealth categories. Furthermore, the median survival times of first ANC visit for poorest, poorer, middle, richer and richest wealth were 9th, 5th, 4th, 4th and 3rd month respectively (Figure 4).
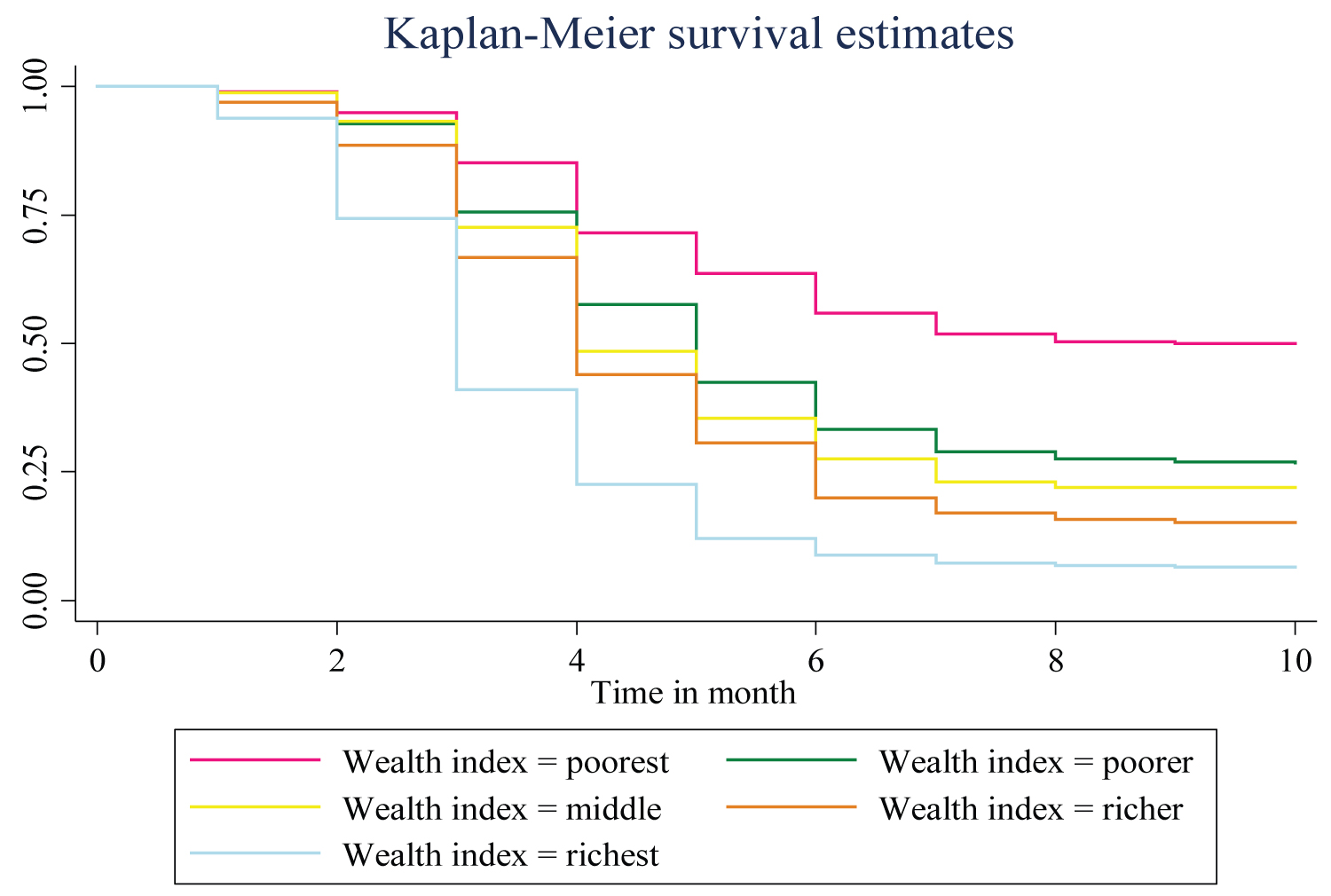 Figure 4: Survival time to first ANC visit among pregnant women by wealth index.
View Figure 4
Figure 4: Survival time to first ANC visit among pregnant women by wealth index.
View Figure 4
Comparison of 'survival' experience by log-rank test: A formal test was carried out using the log-rank to compare the difference between each categorical variable. The general hypothesis states that there is no difference against there are differences among the groups in survival experience time to first ANC visit. The log-rank test result shows that there is no significant difference in the 'survival' experience of different categories for household head (p = 0.744) and marital status. Similarly, the log-rank test performed for different covariates indicate there is statistically significant difference in survival experience among age group (p < 0.001), mother education level (p < 0.001), residence (p < 0.001), wealth index (p < 0.001), parity (p < 0.001), and religion (p < 0.001) (Table 2).
Testing for proportional assumption is vital for interpretation and use of fitted proportional hazard model to look for other models that best fit to the data if the assumption of proportional hazard does not hold. Therefore, a test based on the interaction of the covariates with time and the plot of the scaled Schoenfeld residuals are used to see if the assumption of proportionality is violated or not. The test suggested that the PH assumption is violated for place of religion. Whereas, the global test for Cox proportional hazard has P-Value < 0.05 so do not meet the proportional hazard assumption (Table 3). This departure from proportional hazards occurs when regression coefficients are dependent on time that is when time interacts with covariates. Thus, we doubt the accuracy of the PH assumption and consider the AFT model for this data set.
Table 3: Assumption of proportional hazard model. View Table 3
This study used univariate analysis in order to see the effect of each covariate on time-to-first ANC visit before proceeding to the multivariable analysis. The univariate analysis was fitted for every covariates by AFT models using different baseline distributions i.e. weibull, exponential, log-logistic, and log-normal. In all univariate analysis of AFT models age, marital status, place of residence, woman education, parity, religion, wealth of index and sex of household head associated with waiting time to first ANC visit at 5% level of significance. Hence, based on univariate analysis all explanatory variables are candidates for further analysis. For time-to-first ANC visit data, which is clustered, therefore, a multivariate AFT models of shared frailty (using gamma as well as inverse Gaussian) with weibull, Exponential, lognormal and log-logistic distribution were fitted using gamma as well as inverse Gaussian (Figure 5). To compare the efficiency of different models, AIC and BIC were used, which is most common applicable standard to select the model. A model having the smallest AIC & BIC values is considered the best fitted model. Accordingly, Log logistic AFT model with gamma frailty, which has smallest AIC = 7038.206 and BIC = 7163.764, were selected for the time-to-first ANC visit during gestational age data set (Table 4).
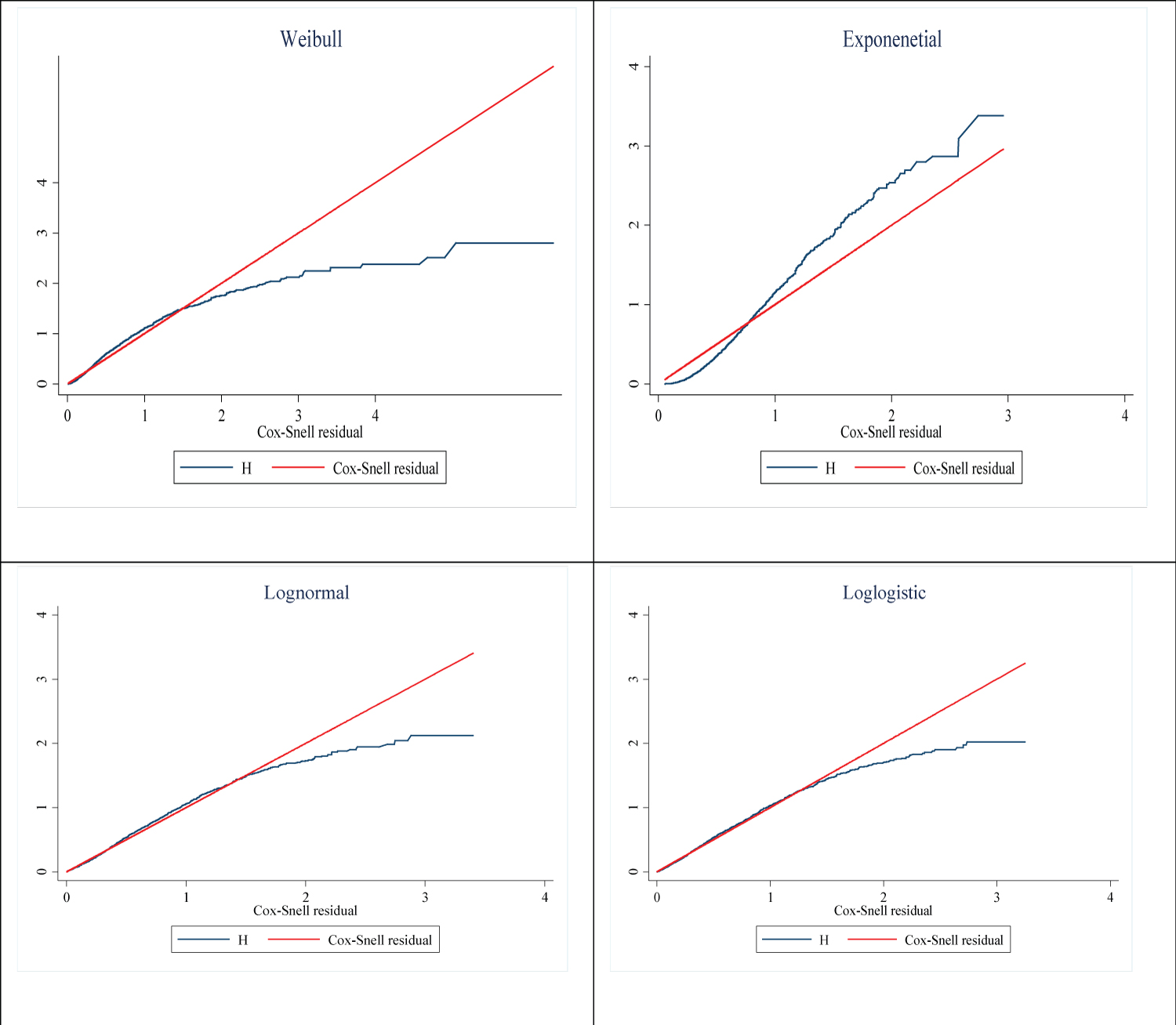 Figure 5: Cox-Snell residual plots for Weibull, exponential, log-normal, and log-logistic AFT models.
View Figure 5
Figure 5: Cox-Snell residual plots for Weibull, exponential, log-normal, and log-logistic AFT models.
View Figure 5
Table 4: Comparison of gamma and Inverse Gaussian shared frailty model with different baseline distributions. View Table 4
The frailty in this model is assumed to follow Gamma distribution with mean 1 and variance equal to theta (θ). There is regional heterogeneity, as seen by the frailty term θ = 0.675. With one degree of freedom and a chi-square value of 692.84, a likelihood ratio test for the hypothesis that θ = 0 yields a very significant p-value of 0.001. This implied that the frailty component had a significant contribution to the model. The result of log logistic multivariable AFT model and covariates such as mother education level, wealth index, sex of house hold head are statistically significant at 5% level of significance. This implies that age, place of residence, marital status and parity has no effect on the survival time-to-first ANC visit among pregnant mothers in Ethiopia. Based on the log logistic AFT regression model, given that the effect of all other factors keep fixed, The acceleration factors for women attending primary, secondary and above education are estimated at 0.918, 0.863 and 0.792 respectively. This implied that women who attended primary, secondary and higher education started their first ANC visit at an early gestational age compared to women who had no education. Regarding religion, women who are followers of Muslim had prolonged time-to-first ANC visit by a factor of 0.907 with a 95% CI (0.857, 0.931) when compared to Orthodox followers women. The acceleration factor and 95% confidence interval for wealth index of pregnant women for a group poorer, middle, richer and richest were 0.917 (0.858, 0.980), 0.890 (0.830, 0.953), 1.136 (0.818, 0.947) and 0.805 (0.735, 0.881) respectively using the poorest as a reference category. This indicates that for poorer, middle, richer and richest groups started ANC earlier than the reference group at a 5% level of significance. The acceleration factor and 95% confidence interval of sex of house hold head for a group of female were 0.944 (0.895, 0.994). This indicates that women who live in female household dead had shortened time to first ANC visit when compared their counterpart (Table 5).
Table 5: Loglogistic Gamma shared frailty model results. View Table 5
According to the WHO and the National Institute for Health and Care Excellence recommendations, the first of such antenatal visits should be conducted in the first trimester (before 14 weeks of gestation) [1].
This study revealed that the median survival time of pregnant women to initiate the first antenatal care visit was at four months of gestation. This finding is lower than studies done in Nigeria median time was six months [23], Ethiopia seven month [24], Malawi five month [25]. This analogous finding might be explained by the country's current adoption of a new focused ANC strategy that mandates the start of first ANC within four months of pregnancy [24]. The findings of this study showed that increasing women's education level significantly shortens the time-to-first ANC visit. The finding is comparable with the report from other studies done in [21,25,26] Illiterate women might have limited understanding of ANC services and their importance to ensure safe delivery [27]. This might be due to higher education leads to better jobs which yield higher income [21]. The other reason might be high chance of exposure for information in case of educated mothers. The justification is that by educating girls, especially those in secondary school or higher, they will be given the tools to make wise decisions about their health care as well as the abilities to become financially independent in the future, raising their standing in the communities where they live [28,29].
The woman's place of residence was one of the variables that affected the time to first antenatal care throughout the gestational age, according to the dataset that was provided. As it was indicated in both log-normal accelerated failure time model and log-logistic gamma shared frailty models the acceleration factor for women who lived in the urban area is much lower than those of rural. This finding is also in agreement with the study done in Vietnam in which rural mothers were attained ANC latter and used fewer visits [17]. This could be due to better presence of ANC providers in urban areas than in rural areas. Also, distances to health facilities are generally shorter in urban centers. There is need to make ANC facilities more accessible to all [20] in addition it might be a result of exposure to health information and awareness on the benefits and advantages of early ANC initiation in favor of urban women [30].
The study also showed that women from richest, rich, middle-class, and poor households started ANC earlier than women from poorest households. This is due to the fact that wealthy women may be more independent, more educated, and more skilled and self-assured when interacting with service providers than impoverished women [31]. A further factor that may prevent women from low-income households from starting ANC on time is hidden costs such those associated with transportation, diagnostics, and lost wages. Due to the workload of their farms or other obligations, impoverished women are also less likely to receive approval from their husbands and other family members to visit a health institution for an ANC checkup. Similarly, poorer women's past interactions with healthcare professionals may have caused them to hesitate to initiate ANC at an early stage [31,32].
Additionally, the expense of the maternity care itself, as well as the transportation to and from the institution, significantly reduced the uptake of the care [33]. Compared to their counterparts, women who live in female households had a shorter time until their first ANC visit.
The factors influencing the time until the first ANC visit were identified using various parametric shared frailty and AFT models using various baseline distributions. The log logistic gamma shared frailty model were well fitted the time-to-first ANC visit dataset than previous parametric shared frailty and AFT models. There was a fragility (clustering) effect on the time to the first ANC visit as a result of variations in the date of the first ANC reception among Ethiopian regions. This suggests that there is heterogeneity and makes the frailty models necessary. This heterogeneity may be a result of the environment, socio-cultural variations in the use of healthcare, and variations in the accessibility of healthcare among Ethiopia's regions. The main variables in this study that were found to be statistically significant included the wealth index, the mother's educational background, the household head's sex, parity, and place of residence. Pregnant women in Ethiopia were more likely to begin their first ANC visit earlier if they came from high income index households, had greater education, and lived in urban regions and female household head. A fourth-month visit to the ANC was the median time of first visit. The study's findings imply that targeted initiatives are required to reach out to women from lower socioeconomic groups, particularly those who are from the poor wealth index, illiterate women, particularly in religious settings.
Ethical clearance for the study was not required since it is a secondary data analysis from EDHS 2019 database. The researchers received the survey data from USAID-DHS program and then the researchers of this study have maintained the confidentiality of the data. The consent was obtained from the study participants during EDHS data collection.
Not applicable.
Data for this study were sourced from Demographic and Health surveys (DHS) and available at: https://www.dhsprogram.com/Data using the detail in the methods section of the document.
The authors declare that they have no competing interests.
No funding available.
DBA, DGB, EAF and SMF conceived the idea for this study; DBA is involved in the data extraction, analysis, interpretation of the finding and writing the original draft. FMA and WDN assisted in the analysis of the study. ESS, RET, TGA, HBE and FMA writing the review and editing the manuscript. All the authors read and approved the final manuscript.
We would like to acknowledge the measure EDHS program which granted as permission to use DHS data.