Extraocular sebaceous carcinoma is an uncommon malignant tumor that usually affects the head and neck. Despite being rich in sebaceous glands, vulvar sebaceous carcinoma is extremely rare. We report a case of vulvar sebaceous carcinoma in a 64-year-old woman that presented as an asymptomatic nodule and was successfully treated by wide local excision. The number of reported cases of vulvar sebaceous carcinoma is very small, more cases need to be collected in order to identify prognostic factors and appropriate management modalities.
Sebaceous carcinoma, Vulva, Local excision
Sebaceous carcinoma (SC) is a well described type of malignant adenocarcinoma with sebaceous differentiation. However, this type of neoplasm is very rarely seen in the vulvar area. The most common malignant neoplasms of vulva are squamous carcinomas (87%) and malignant melanomas (6%) [1]. Today, there are only a few reported cases of sebaceous carcinoma of the vulva and they have varying clinical courses. Here, we report a case of vulvar sebaceous carcinoma that presented as a slow growing lump without any associated vulvar skin lesions or metastases that was successfully treated with local excision.
A 64-year-old woman was referred to our Vulvar clinic by her primary care physician for a vulvar lump that developed over 12 months. The lump was relatively asymptomatic; there was no associated pain, pruritus, bleeding, or discharge. She had other comorbidities of diabetes, chronic renal impairment, and osteoporosis with a BMI of 18 kg/m2. Her other personal and family medical was unremarkable. Physical examination revealed a 2 × 1.5 cm erythematous nodule on the right labium minus (Figure 1). The surrounding area was clear. No enlarged inguinal nodes were detected. Examination of vagina and cervix were within age-appropriate normal limits. A Keyes punch biopsy was performed and was suggestive of adnexal neoplasm. Computed tomography did not reveal any abnormality in pelvis and groin nodes. In view of the patient's comorbidities, the lump was excised under local anesthesia. Histologically, the specimen showed skin with a dermal tumor composed of nests and lobules of basaloid cells accompanied by a dense lymphoplasmacytic infiltrate (Figure 2). The tumor cells showed a high nuclear to cytoplasmic ratio with pleomorphic, irregular nuclear membranes, vesicular nuclei and prominent nucleoli. The cytoplasm had a foamy and micro vesicular appearance, which was more prominent towards the center of the lobules (Figure 3). Occasional large intracytoplasmic vacuoles were present. There was brisk mitotic activity. Some areas showed comedo necrosis. The surface epithelium was focally ulcerated. Pagetoid spread of tumor cells to the overlying epidermis was noted, but no definite lymphovascular invasion was seen. These tumor cells were strongly and diffusely immunoreactive to p53. Combined with clinical presentation, these findings lead to the diagnosis of vulvar sebaceous carcinoma. All resection margins were uninvolved. At the time of reporting, the patient has now been recurrence-free for 22 months.
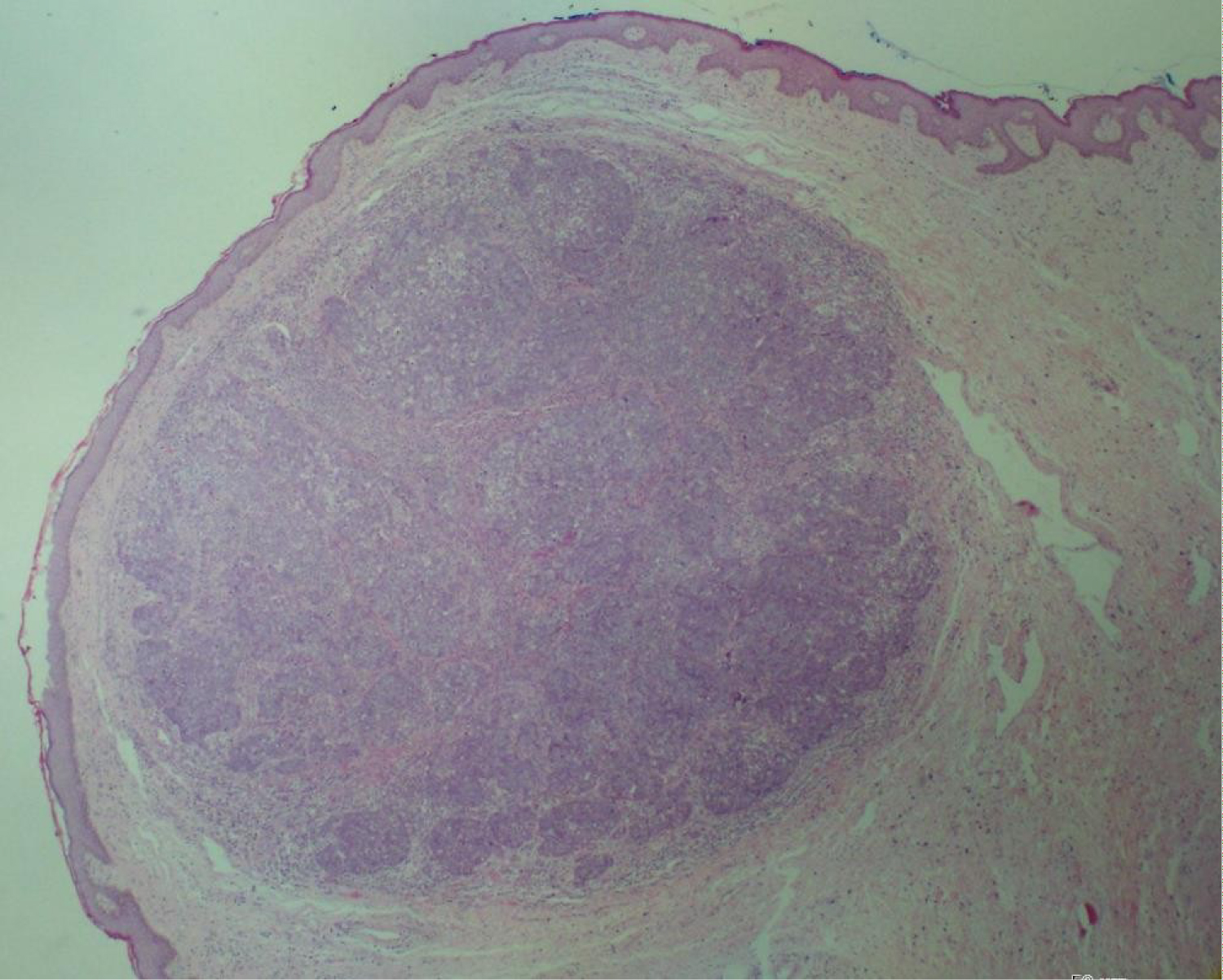 Figure 1: CT - angiography, CT - perfusion and cerebral angiography before endovascular treatment. A) CT - angiogram showing AVM and aneurism localization; B) CT - prefusion showing hyperperfusion zone in AVM and high-flow drainage vein; C) Cerebral angiography showing AVM of the right fronto-parietal region and the proximal flow - related aneurysm on the right terminal ACA afferent.
View Figure 1
Figure 1: CT - angiography, CT - perfusion and cerebral angiography before endovascular treatment. A) CT - angiogram showing AVM and aneurism localization; B) CT - prefusion showing hyperperfusion zone in AVM and high-flow drainage vein; C) Cerebral angiography showing AVM of the right fronto-parietal region and the proximal flow - related aneurysm on the right terminal ACA afferent.
View Figure 1
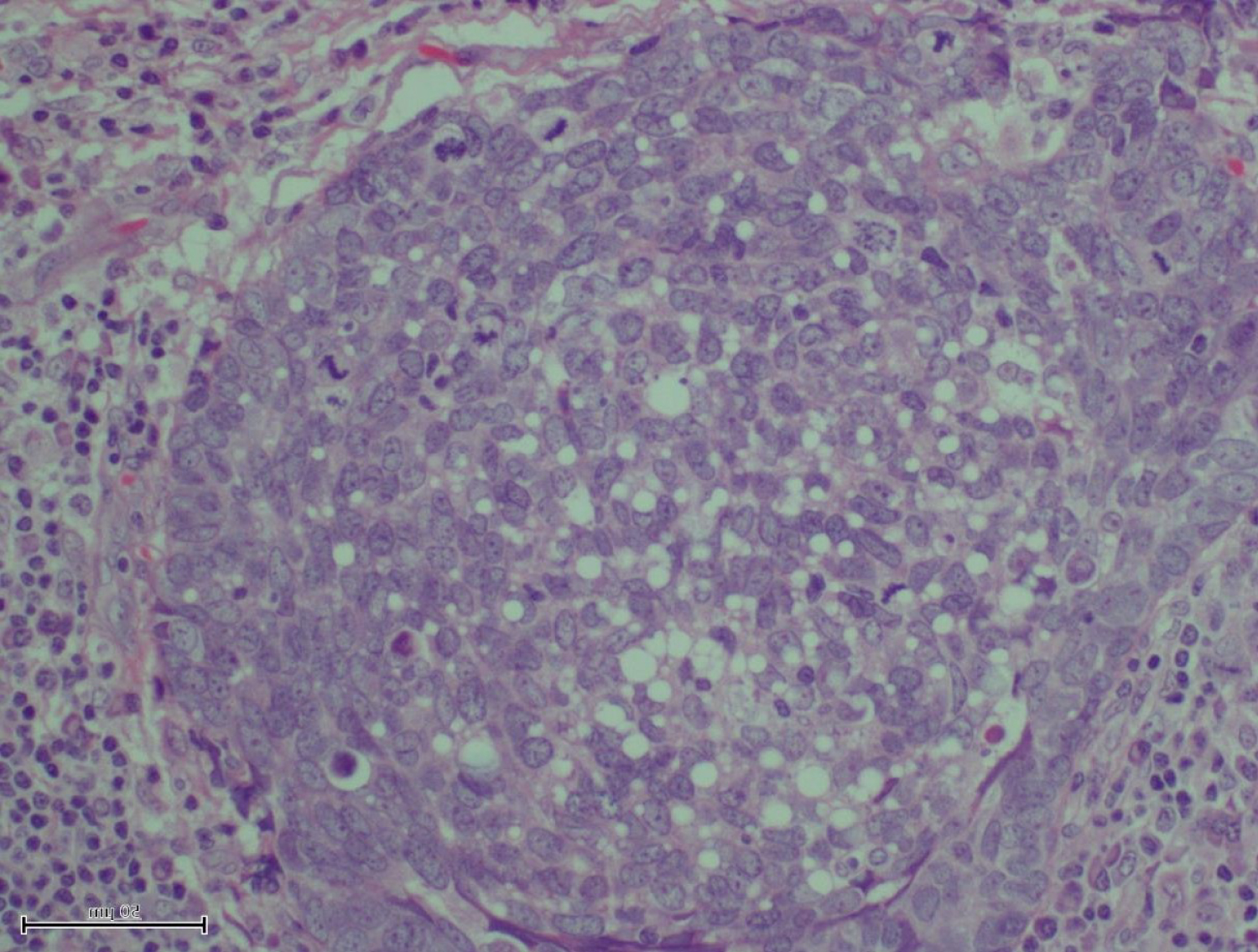 Figure 2: Superselective angiography: Determined by the right recurrent artery of Heubner and normal perforating arteries extending from the aneurism neck.
View Figure 2
Figure 2: Superselective angiography: Determined by the right recurrent artery of Heubner and normal perforating arteries extending from the aneurism neck.
View Figure 2
 Figure 3: Supreselective angiography showing AVM node and embolized fistulous part of the AVM.
View Figure 3
Figure 3: Supreselective angiography showing AVM node and embolized fistulous part of the AVM.
View Figure 3
Extraocular sebaceous carcinoma most often occurs on the head and neck region. Although sebaceous glands are abundant and may be prominent on the vulva, only 10 cases of vulvar sebaceous carcinoma have been reported in the literature, to our knowledge. The presentation is often nonspecific with ulcer, plaque, nodules or exophytic tumors. The duration of symptoms ranges from 4 months to 2 years and the age at presentation from 31 to 89 years. Due to their nonspecific presentation, they are often recognized late. Vulvar sebaceous carcinoma was reported to be associated with Bowen's disease [2,3] and colonic adenocarcinoma, likely in the setting of Muir-Torre syndrome [4], although most cases were isolated [5].
Very little is known about the aggressiveness and natural history of vulvar SC. The rarity of the condition limits the possibility of reliably estimating remission, recurrence, and survival rates. It is, hence, difficult to formulate treatment recommendations. The few cases in the literature have very differing clinical courses (Table 1). Khan, et al. reported a SC in a 49 years old woman with disease spread to the inguinal lymph nodes who underwent local excision and bilateral groin node dissection but recurred within 7 months [6]. In contrast to this, Kawamoto, et al. described a case that also had inguinal metastases at presentation; she was offered surgery with adjuvant radiotherapy and was recurrence free for the rest of the follow-up period [2]. Similarly to ours, a number of reported cases had not spread at presentation and did not recur after initial treatment [7-10]. To date, only one case was documented to have distant metastasis [11]. Commonly used treatment modalities include surgical excision (wide local excision or hemi vulvectomy with or without inguinal lymphadenectomy), chemotherapy and/or radiotherapy as adjuvant treatment or for recurrence.
Table 1: Literature with differing clinical courses. View Table 1
It is difficult to identify clear prognostic factors due to the extremely small number of cases. Nonetheless, we note that only the case with local recurrence had local-regional lymphatic spread at presentation and was only treated surgically. The other case with lymphatic spread was successfully treated with surgery and adjuvant radiotherapy; no recurrence was noted by the end of follow up. This indicates a possibility of lymphatic spread being a predictor of recurrence and adjuvant radiotherapy an adequate treatment modality in such cases. Even though, extraocular SC is thought to be more aggressive than its periocular counterpart, these reports suggest that with appropriate management most case can be successfully cured.
I have no conflict of interest. This project was conducted at the KK Women's and Children's Hospital, 100 Bukit Timah Rd, Singapore. This project received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.