Solitary pulmonary lung nodule is a rare presentation of differentiated thyroid metastatic disease with significantly increased mortality. Current data about diagnosis and treatment are limited, based mostly on case reports.
We present a case of a 56-year-old woman diagnosed with solitary pulmonary metastasis of papillary thyroid carcinoma describing the diagnostic challenge, the chosen treatment and the long-term follow-up results.
The patient initially underwent a total thyroidectomy and received radioactive treatment for locally advanced papillary thyroid carcinoma. During the follow-up scans, a solitary nodule in the left lung was identified, with positive uptake in fluorodeoxyglucose PET-CT but not in an radioactive iodine uptake scan. She underwent a video-assisted thoracoscopic wedge resection. Pathology revealed metastatic papillary thyroid carcinoma. To date, five-years later, she is in a complete remission.
Our case demonstrates the role of surgery, not only for diagnosis but also as a single treatment for solitary lung metastasis of thyroid carcinoma providing long term remission.
Papillary thyroid carcinoma, Solitary pulmonary metastasis, Surgical resection, Follow-up
Differentiated Thyroid Carcinoma (DTC) is one of the most curable cancers and usually carries a good prognosis [1,2]. Distant metastases of DTC are relatively rare, with a wide prevalence range of 4-23% [3]. Nevertheless, it is the most common cause of thyroid cancer-related death, and is associated with a worse prognosis and a median survival of 4.1 years [4]. The most common sites for distant metastasis are in the lungs and/or bones [1,4]. The classical lung involvement is diffuse lesions involving both lungs, in micronodular or miliary patterns. Solitary lung lesion is a rare presentation and is described mostly by case reports [5-7]. Hence, data concerning the diagnosis and treatment of choice is limited.
The main treatment modality for thyroid metastasis is high-dose radioactive iodine (RAI) therapy. Other treatment options include external beam radiation and targeted tyrosine kinase inhibitors for RAI-refractory cases [3,8]. Metastasectomy have been reported mostly with regard to bone metastasis, more as a palliative measure rather than a curative one [2,9]. The role of pulmonary metastasectomy remains unclear, with only scant literature based on case reports and retrospective data only [10]. Only a few reports on pulmonary metastasectomies have described a cure [7,11]. Although the follow-up was relatively short for a cure estimation from papillary thyroid carcinoma (PTC), as recurrences may appear years following the treatment.
Here we present a five-year follow-up of a 56-year-old woman diagnosed with a PTC solitary pulmonary metastasis, successfully treated with surgical resection.
A 56-year-old Caucasian woman was diagnosed with a solitary pulmonary nodule found during a follow-up for PTC. Four years prior, the patient was treated with mercaptizole for Graves' disease, and was followed up in an institutional endocrinology clinic. She underwent a right hemithyroidectomy due to the presence of a suspicious thyroid nodule classified as Bethesda category III) on fine needle aspiration. The pathology examination demonstrated a 15 mm PTC with macroscopic strap muscle invasion. The patient underwent a completion thyroidectomy, with no additional tumor foci. The patient was treated with 150 mCi RAI after withdrawal of thyroid hormone treatment. Post-treatment thyroglobulin levels was 0.2 ng/mL (normal range 0.8-55.00 ng/mL), and her thyroglobulin Ab level was 216 IU/ml (normal range 10.00-40.00 IU/ml). Five months later, a follow-up Thyrogen stimulated radioiodine scan with SPECT/CT was performed, demonstrating an indeterminate finding in the right lung lobe, for which a CT scan was recommended. The patient underwent a chest CT scan which showed a 21 × 16 mm mass in the left lung upper lobe (Figure 1), with no lesion in the right lung. The lesion in the left lung demonstrated a pathological fluorodeoxyglucose (FDG) uptake in a PET-CT scan (Figure 2). Seven month after the surgery, the thyroglobulin and thyroglobulin AB were undetectable. At this point, the differential diagnosis included primary lung cancer or a metastatic lesion of thyroid origin. A video-assisted thoracoscopic excisional biopsy was performed. The pathology examination revealed a 25 mm focus of metastatic papillary thyroid carcinoma, resected with clear margins (Figure 3). Staining was positive for thyroid Transcription Factor-1 (TTF1), thyroglobulin and cytokeratin (CK) 7. The surgery and the postoperative course were uneventful. The postoperative FDG PET-CT scan confirmed resolution. From the ambulatory follow-up to the current date, the patient is in complete remission without any structural or biochemical evidence recurrence for a period of 61 months.
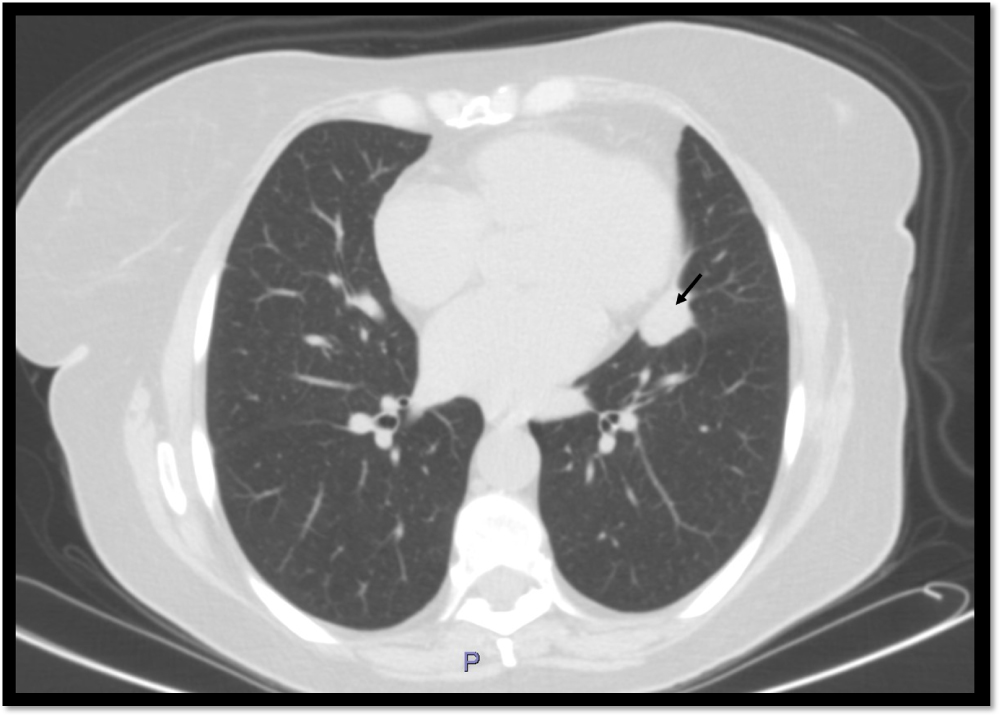 Figure 1: A Computed Tomography (CT) scan of the chest, axial section. A 21 × 16 mm solid lesion in the lingula precardial area of the left upper lobe (arrow) is demonstrated without evidence for lymph nodes enlargement.
View Figure 1
Figure 1: A Computed Tomography (CT) scan of the chest, axial section. A 21 × 16 mm solid lesion in the lingula precardial area of the left upper lobe (arrow) is demonstrated without evidence for lymph nodes enlargement.
View Figure 1
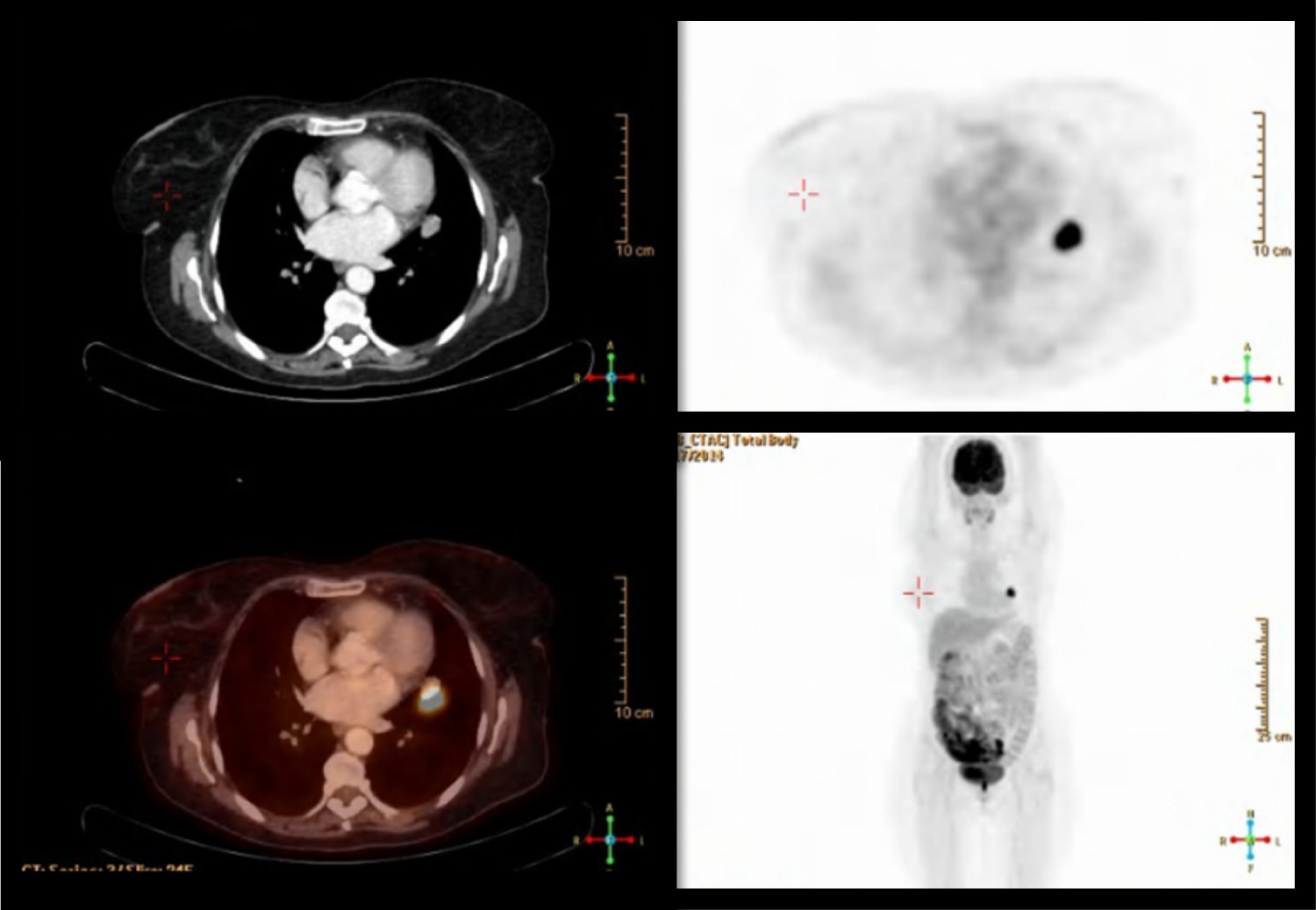 Figure 2: PET/CT scan with FDG. A 22X14 mm lesion with spiky borders is demonstrated in the left upper lobe paramediastinal, in close proximity with the pericard. No pathological uptake of FDG was demonstrated in the neck region.
View Figure 2
Figure 2: PET/CT scan with FDG. A 22X14 mm lesion with spiky borders is demonstrated in the left upper lobe paramediastinal, in close proximity with the pericard. No pathological uptake of FDG was demonstrated in the neck region.
View Figure 2
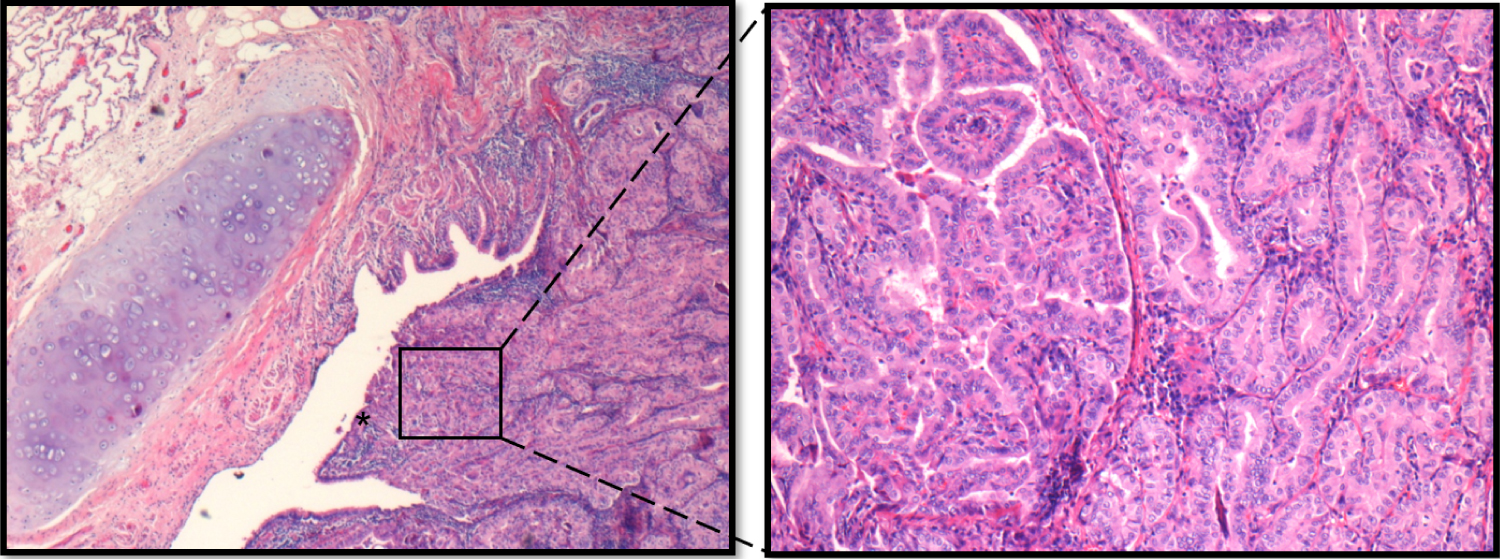 Figure 3: (A) A 25 mm focus of metastatic papillary thyroid carcinoma in the lung, adjacent to a bronchus and involving the bronchial mucosa (asterisk); (B) Magnification of the tumor foci demonstrating papillary structures. Hematoxylin and Eosin stain.
View Figure 3
Figure 3: (A) A 25 mm focus of metastatic papillary thyroid carcinoma in the lung, adjacent to a bronchus and involving the bronchial mucosa (asterisk); (B) Magnification of the tumor foci demonstrating papillary structures. Hematoxylin and Eosin stain.
View Figure 3
About one-third of advanced DTC have metastatic lesions with low avidity for radioiodine treatment at the time of diagnosis or during the progression of the disease, when the ability to concentrate radioiodine is lost. In our patient, the thyroid carcinoma presented as a combination of RAI sensitive neck disease and non-avid iodine solitary lung metastasis. Solitary metastasis is relatively uncommon and was previously reported mostly in the lung, bone and brain [1]. The pre-operative diagnosis of a solitary lung metastasis might be misleading and requires a high index of suspicion. In this case, the lesion was discovered several months following the initial surgery, without evidence of previous regional spread, despite significant thyroid disease with strap muscle involvement.
DTC typically metastasizes through lymphatic spread leading to stepwise progression from primary to regional and then distant metastasis. The presentation here of solitary lung metastasis without regional disease in the neck may suggests that the metastatic spread was hematogenous, thus 'skipping' the regional neck.
RAI is currently the treatment of choice for thyroid cancer metastases. It is considered effective for microscopic metastatic disease but may not be sufficient for macroscopic metastases [12], which require extremely high radiation doses to reach a tumoricidal effect [11,13]. High dose RAI for pulmonary metastasis has been associated with impaired pulmonary functions and pulmonary fibrosis [14]. Furthermore, a pulmonary macronodular lesion was shown to be a predictor for non-131I-avid metastases, as seen in this case report as well. This leads to a lower response rate and reduced survival rates [1,3].
When the metastatic disease is not amenable to RAI therapy, the National Comprehensive Cancer Network (NCCN) guidelines suggests local treatment, such as surgical resection or radiation [2].
Previous retrospective series on the role of metastasectomy for DTC metastatic diseases have showed beneficial effects, with regard to all sites, including the lung [9-11]. Pak, et al. reviewed 47 surgeries for distant metastasis in advanced thyroid cancer, including 12 pulmonary metastasectomies used in conjunction with RAI therapy, and found it beneficial [11]. In Porterfield et al. study, pulmonary resection for thyroid metastasis was safe with low morbidity and mortality and demonstrated improved long-term survival [10]. Here, we report on a five-year disease-free follow-up after metastasectomy as a single modality. Previous studies have suggested criteria for pulmonary metastasectomy (1) Absence of widely disseminated disease; (2) Eradication of the primary tumor; (3) No medical contraindications for surgery; and (4) Adequate pulmonary function that can tolerate resection of all documented disease [11,15]. These terms were verified during the course of this case report, leading to remission by surgery.
In a solitary lung metastasis, surgery appears to be pivotal for the diagnosis and can achieve long-term remission when used as a single modality. Surgery allows the avoidance of RAI large doses and related complications. Thus, surgery as an additional treatment option should be considered in patients with solitary metastases of thyroid carcinoma.
The authors report no conflicts of interest.