Glandular cystitis is a differential diagnosis of malignant bladder tumors. Only the Pathological examination can be used to make a diagnosis. Glandular cystitis has no specific clinical manifestation. The clinical signs are not very specific and suggest bladder carcinoma. Principles of treatment for Glandular cystitis were used to treat these causative factors. Trans-urethral resection of the bladder pseudotumoral forms. The course of glandular cystitis is controversial and primarily focuses on the risk of lesion degeneration and requires regular monitoring of both radiological (CT) and, and biological (renal) function, urinary cytology), and control cystoscopy with multiple biopsies. Lack of consensus surveillance and the lack of perspective makes it difficult to understand the evolution of this pathology.
We report in our work, a case of Florid glandular cystitis with 15 years of follow-up while highlighting the therapeutic and the prognostic difficulties encountered during follow-up. This risk is primarily associated with malignant degeneration.
Glandular cystitis, Recurrences, 15 Years follow up
TURB: Transurethral Resection of the Bladder; uro-CT Scan: uro-Computed Tomography Scan
Described for the first time in 1761 by Morgani [1], Glandular cystitis is a benign metaplasia, developed from Von Brunn's islets (epithelial clusters included in the mucous chorion). Rare, usually asymptomatic; it is favored by chronic irritation, and is sometimes associated with pelvic lipomatosis.
Its transformation into adenocarcinoma is exceptional and occurs in the case of persistence of the favoring factor. However, annual monitoring using cystoscopy with bladder biopsy is necessary. The florid form is considerably rarer and more disabling. It usually requires wide excision of the lesions. Here, we report a case of florid glandular cystitis with 15 years of follow-up, whose data are compared with those of the literature.
In our work, we report the case of a 54-year-old weaned patient with a history of chronic smoking weaned 1 year ago. The patient has been followed up since 2003 for florid glandular cystitis with multiple transurethral resections of the bladder "TURB" (9 TURB in total), and the last TURB dates back to 02/2021. In 2003, the patient had his first TURB for a bladder tumor, the pathological examination of which revealed glandular cystitis. Th patient underwent annual follow-up cystoscopies; recurrences were marked by de novo onset of irritation. Bladder syndrome, pollakiuria, and repetitive episodes of urinary tractinfection. Diagnosis of recurrence was confirmed by follow-up cystoscopy, in which recurrence was always in the trigonal region (Figure 1). Pathological examination results in all TURBs in favor of glandular cystitis (Figure 2).
Glandular cystitis is a benign tumor of the bladder, predominantly Male, Cases reported in women are rare, and cases with recurrences are rarer. Its incidence varies between 0.1% and 1.9%, it is a differential diagnosis of malignant bladder tumor [2]. The mechanisms of occurrence of glandular metaplasia of the bladder are still poorly understood. It generally develops in a context of chronic inflammation whose causesare variable: Urinary stasis, bladder lithiasis, chronic catheterization, urinary tract infection, bladder tumor, and neurogenic bladder. More rarely, other factors are noted such as allergy, exposure to toxicants, hormonal imbalances, and bladder diverticula [3]. Likewise, pelvic lipomatosis is associated in 75% to 80% of cases with glandular cystitis [4]. The uro-CT scan rules out or confirms the presence of pelvic lipomatosis, it can help to act on the obstruction earlier, and therefore avoid complications of chronic obstruction of the upperurinary tract. In general, the search for the causal factor does not, in all cases, lead to its identification, this is the case with our patient where no cause was highlighted. Glandular cystitis has no specific clinical translation. The Clinical signs are not very specific and suggest a bladder carcinoma. Several modes of revelation are described either by macroscopic hematuria, by chronic irritative voiding disorders of the bladder, rarely obstructive signs linked to the invasion of the two meatus by a florid form associated or not with the envelopment of the pelvic ureters by associated pelvic lipomatosis [5]. Our patient presented with symptoms of bladder irritation without obstructive signs. The various explorations confirm the positive diagnosis, which is that of urothelial carcinoma. Only the anatomopathological examination, makes it possible to highlight the cylindrical glandular tissue at the level of the mucosa and the submucosa, and provides diagnostic certainty. There are two histological types of glandular cystitis: The first called typical form and the second: Intestinal metaplasia of the bladder [6]. The exact proportions of these two subtypes are not known; in contrast, studies agree that intestinal bladder metaplasia is much less common than the typical form. These two histological types of glandular cystitis are distinguished by different or even opposite immunohistochemical profiles. The principles of treatment for glandular cystitis are to treat the causative factor if it is shown. Trans-urethral resection of the bladder for pseudotumoral forms: Which should be complete and deep if possible; Over a period of 15 years our patient had 9 TURBs the last date back to 02/2021. And finally, non-conservative surgery is for complicated forms. The course of glandular cystitis is very controversial and is primarily focused on the risk of lesion degeneration, and requires regular monitoring both radiological (CT), biological (renal function, urinary cytology) and control cystoscopies with multiple biopsies. The lack of consensus around surveillance and the lack of perspective are a difficulty in knowing the evolution of this pathology.
Glandular cystitis is rare, has no specific clinical translation, poses a problem of differential diagnosis with malignant bladder tumors, only the pathological examination allows a positive diagnosis to be made. The treatment is based on the treatment of the causative factor if identified, otherwise a complete and deep resection of the lesion. Close follow-up is essential given the risk of recurrence and degeneration.
Consent was obtained or waived by all participants in this study. Ethics committee in the Military hospital of Meknes issued approval not applicable. Disclosure statement: No potential conflict of interest was reported by the author(s). Informed consent: Informed consent was obtained. Ethical approval was obtained from the local ethics committee in the Military hospital of Meknes- Morocco and the patient consented to participate in the case report and his information was handled as anonymous according to the ethical standards.
The authors declare no conflict of interest.
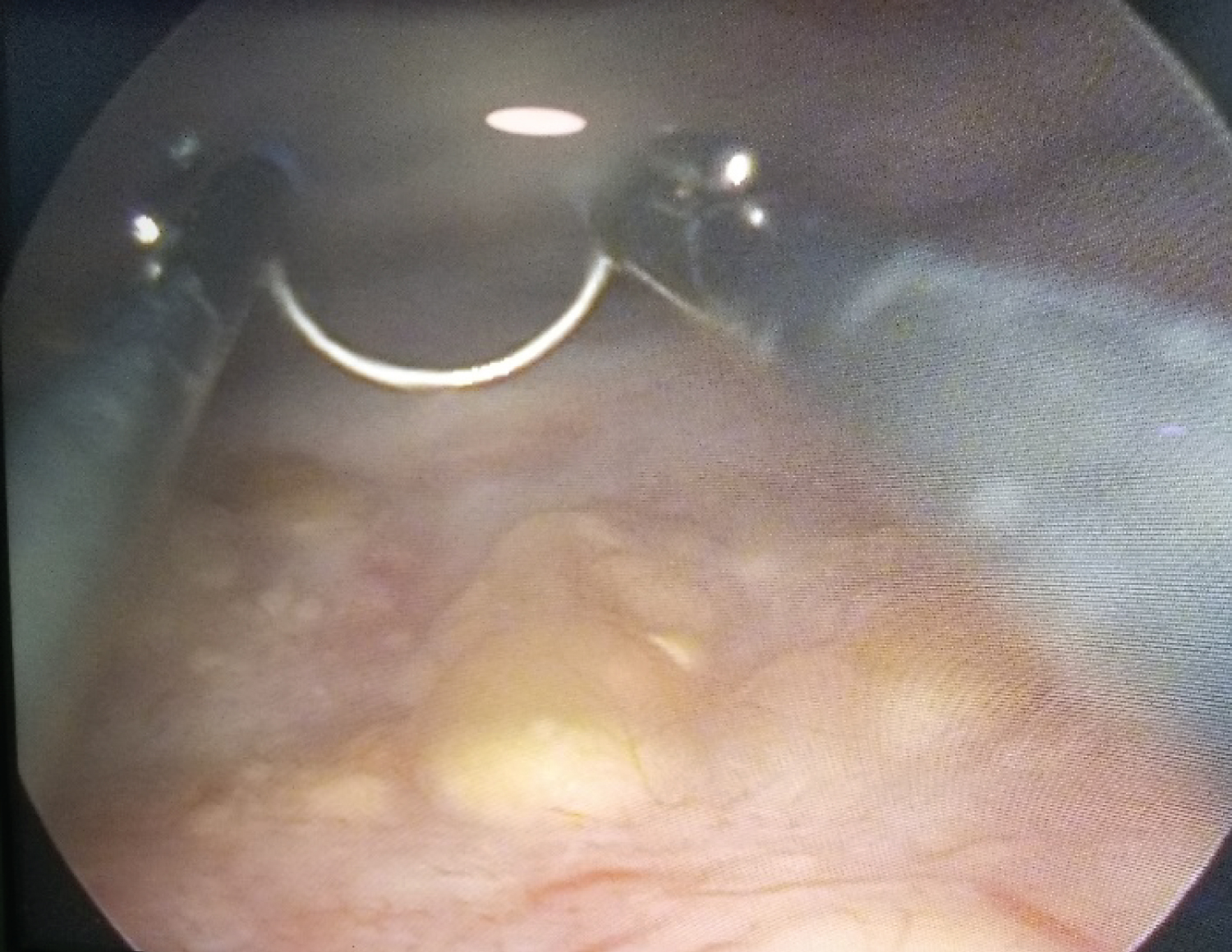
Figure 1: Endoscopic aspect of the bladder tumor: Localization in the trigonal region.
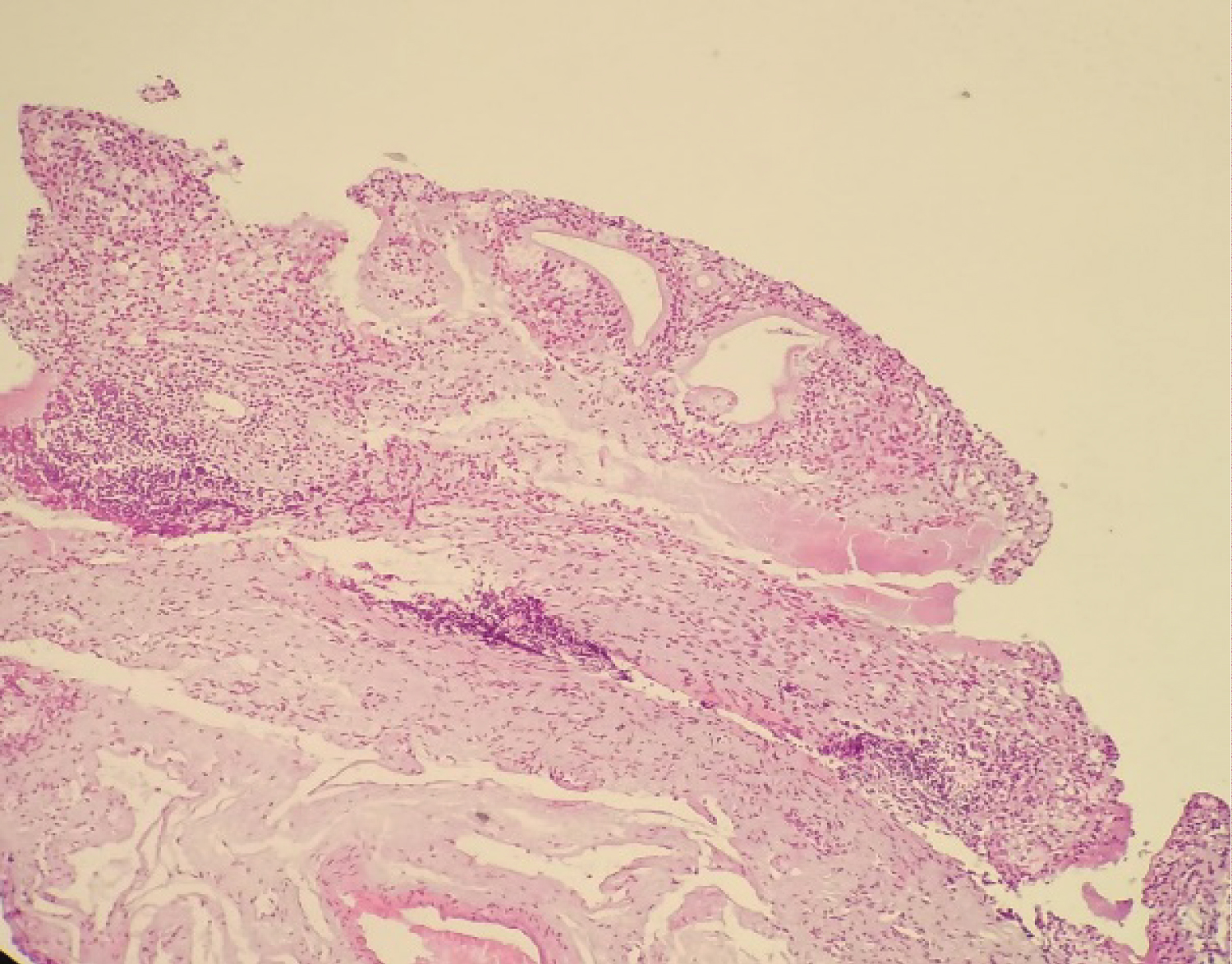
Figure 2: Von Brunn's glands take on a cystic appearance with glandular metaplasia.