Spontaneous psoas hematoma, Hemophilia, Conservative management
Spontaneous hematoma of the psoas muscle is a rare entity whose incidence varies between 0.6% and 6.6% [1] and is potentially fatal. Although hematomas of traumatic origin are reported, spontaneous hemorrhages are relatively more frequent.
Spontaneous iliopsoas hematomas usually occur in patients with coagulopathy due to hemophilia or anticoagulants/antithrombotics. Clinically, patients present with pain in the right iliac fossa, groin or back, with a flexed hip and tenderness in passive extension, or even signs of hypovolemia.
Femoral compression neuropathy may be present, leading to sensory numbness or paresthesia of the ipsilateral lower limb, and quadriceps muscle weakness [2].
We present the case of a 50-year-old patient, characterized by the onset at a late age of a spontaneous hematoma of the psoas secondary to hemophilia A, hitherto unrecognized.
We present a case of a 50-year-old patient, with no notable pathological history, who had presented excruciating left lumbar pain (VAS: 9) for 10 days with sudden onset and progressive worsening associated with motor deficit of the ipsilateral lower limb.
The clinical examination found an isolated motor deficit of the quadriceps and the left hamstrings rated 1/5, associated with impaired sensitivity at the level of the antero-internal face of the thigh with ecchymotic spots at the level of the left lumbar fossa.
A complete biological assessment was carried out, which objectified a TCA elongated to 69.6, a hemoglobin 5.1.
With these biological abnormalities, an injected abdominal CT scan was performed which showed (Figure 1 and Figure 2).
Our initial management was to transfuse the patient with red blood cells and fresh frozen plasma, to undergo and analgesic treatment with bi-antibiotic therapy based on third-generation cephalosporins and aminoglycosides to avoid super infection of the hematoma.
We then completed our biological assessment with a dosage of factors XI, XII, and Willebrand factor. This objectified a collapsed factor VIII level (< 1%) so the diagnosis of acquired hemophilia A was retained in our patient.
After consultation with the systemic disease specialist, the decision was to put the patient on oral corticosteroid therapy.
Faced with these major coagulation disorders, our attitude was conservative given the major risk to the vital prognosis of the patient, even if the functional prognosis is compromised.
Treatment of iliopsoas hematoma mainly includes conservative treatment, ultrasound- or CT-guided percutaneous drainage, embolization, incision, and surgical or laparoscopic retroperitoneal drainage. The therapeutic modality is chosen based on the clinical manifestations and the severity of the hematoma [3-5]. Conservative treatment is recommended for patients with mild bleeding and no apparent symptoms of nerve compression, which includes discontinuation anticoagulant drugs as in the present case, bed rest, and blood transfusion [4]. For patients with significant pain, percutaneous drainage and decompression guided by ultrasound or CT may be indicated. Angiography may be considered for acute life-threatening massive hemorrhage, if the bleeding point of a pulsating artery can be identified, arterial embolization is the treatment of choice [5]. For patients with complete paralysis of the femoral nerve by compression by iliopsoas hematoma following trauma, decompression by surgical incision and drainage is indicated, retroperitoneal laparoscopic treatment may also be considered [5,6].
Spontaneous psoas hematomas are usually linked to acquired or congenital coagulation disorders: anticoagulant accident, anti-factor VIII autoantibodies, hemophilia, Von Willebrand disease, various coagulation factor deficiencies.
It seems reasonable to opt for medical management with bed rest and correction of bleeding abnormalities, in patients who have little or no neurological complications. However, when a patient presents with significant and especially profound neurological deficits, surgical exploration and decompression may be the treatment of choice.
None.
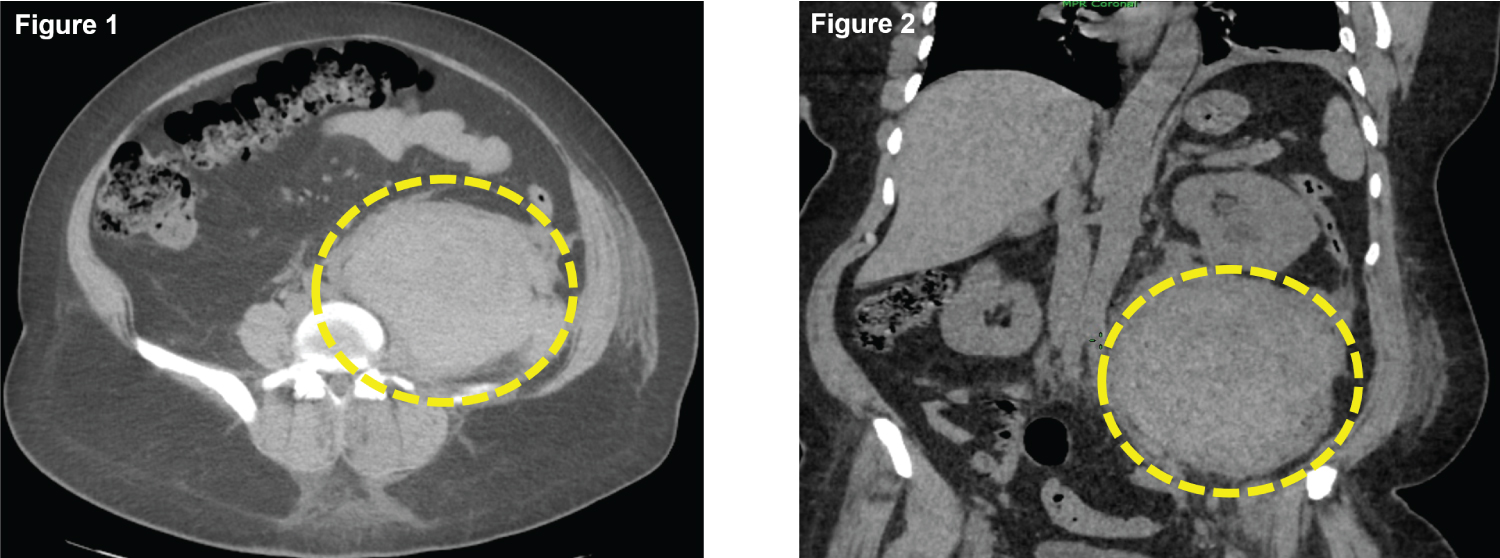
Figure 1: An abdominal CT scan showing the presence of a large hematoma of the left psoas muscle measuring 18 cm*12 cm compressing the ipsilateral ureter with uterohydronephrosis.