A previously well 71-year-old male presented with recurrent stereotyped episodes of right hemisensory disturbance, weakness, and expressive dysphasia lasting 10-20 minutes. Cognitive decline had been noted over the preceding 6-months. He was otherwise in good health with no history of infective symptoms or prior neurosurgical procedures. Interictal neurological examination was unremarkable.
EEG was abnormal with asymmetrical slowing over the left hemisphere and he was commenced on sodium valproate 400 mg B.D. for presumed focal seizures, with initial resolution of the episodes. Magnetic resonance imaging (MRI) demonstrated dural thickening over the left cerebral convexity with post-contrast enhancement. Cerebrospinal fluid (CSF) microscopy revealed a mild mononuclear leucocytosis (WCC 8 × 10^6), with normalprotein and glucose and no growth on culture. Cytology was unremarkable.
Further investigation for malignant and infectious causes, including CT chest/abdomen/pelvis, progress MRI brain and repeat CSF analysis were underway when he re-presented two months laterwith an abrupt recurrence of fluctuating neurological deficit and persistent right sided weakness. A progress MRI revealed progression of the leptomeningeal thickening with contrast enhancement (Figure 1). A left frontal stereotactic craniotomy with resection of dura and subarachnoid membrane was performed, with purulent material visualised in the sulci (Figure 2). Histology of dural and subdural tissue specimens was consistent with a pauci-inflammatory pachymeningitis with no evidence of malignancy. On day four of incubation growth of Cutibacterium acnes was identified from all specimens using VITEK MS MALDI-TOF (database V3.0 KB-clinical, bioMérieux, France).
Minimal right-sided weakness and mild dysphasia remained whilst the patient completed a six-week course of Penicillin G, 15 million units daily by continuous IV infusion at home. Post-treatment MRI demonstrated an extradural collection deep to the craniotomy, measuring 3 × 1.5 cm with mass effect to the underlying brain parenchyma. C. acnes was again cultured from multiple specimens including the overlying bone flap tissue, dural, and subdural tissue collected at re-do craniotomy and washout. On this occasion, the bone flap was removed and a six-week course of intravenous vancomycin therapy was completed with resolution of infection. At two-year follow-up he had no further seizures off anticonvulsant therapy and no focal neurological deficits were present.
C. acnes is a Gram positive anaerobic rod-shaped bacterium that usually forms part of the normal cutaneous flora [1], and can be found in the mouth, nares and genitourinary tract [1]. While C. acnes is a well-recognised cause of neurosurgical infection [2], primary central nervous system (CNS) infection is uncommon, but has been described as a complication of sinus and mastoid infections, and following facial trauma [3]. In one case series of nine patients with de novo C. acnes CNS infection and meningism, an indolent course progressing over weeks to months was common [4].
When introduced into deeper structures C. acnes acts as an opportunistic pathogen and is capable of haematogenous seeding, and forms a biofilm in the presence of a prosthetic device [1]. This has important treatment implications, necessitating the need for surgical debridement of involved structures and removal of prostheses where present. C. acnes remains highly susceptible to beta-lactams and glycopeptides, with increased resistance to clindamycin and tetracyclines reported [5,6]. Antimicrobial susceptibility testing is not routinely performed on C. acnes isolates in our laboratory.
To our knowledge, this is the first reported case of de novo C. acnes CNS infection, where focal neurological deficit in the absence of other signs of meningeal irritation has occurred as the primary manifestation. While his disease relapse remains unexplained, biofilm formation affecting the residual bone flap may be implicated and highlights the importance of thorough surgical debridement despite the seemingly indolent nature of this pathogen.
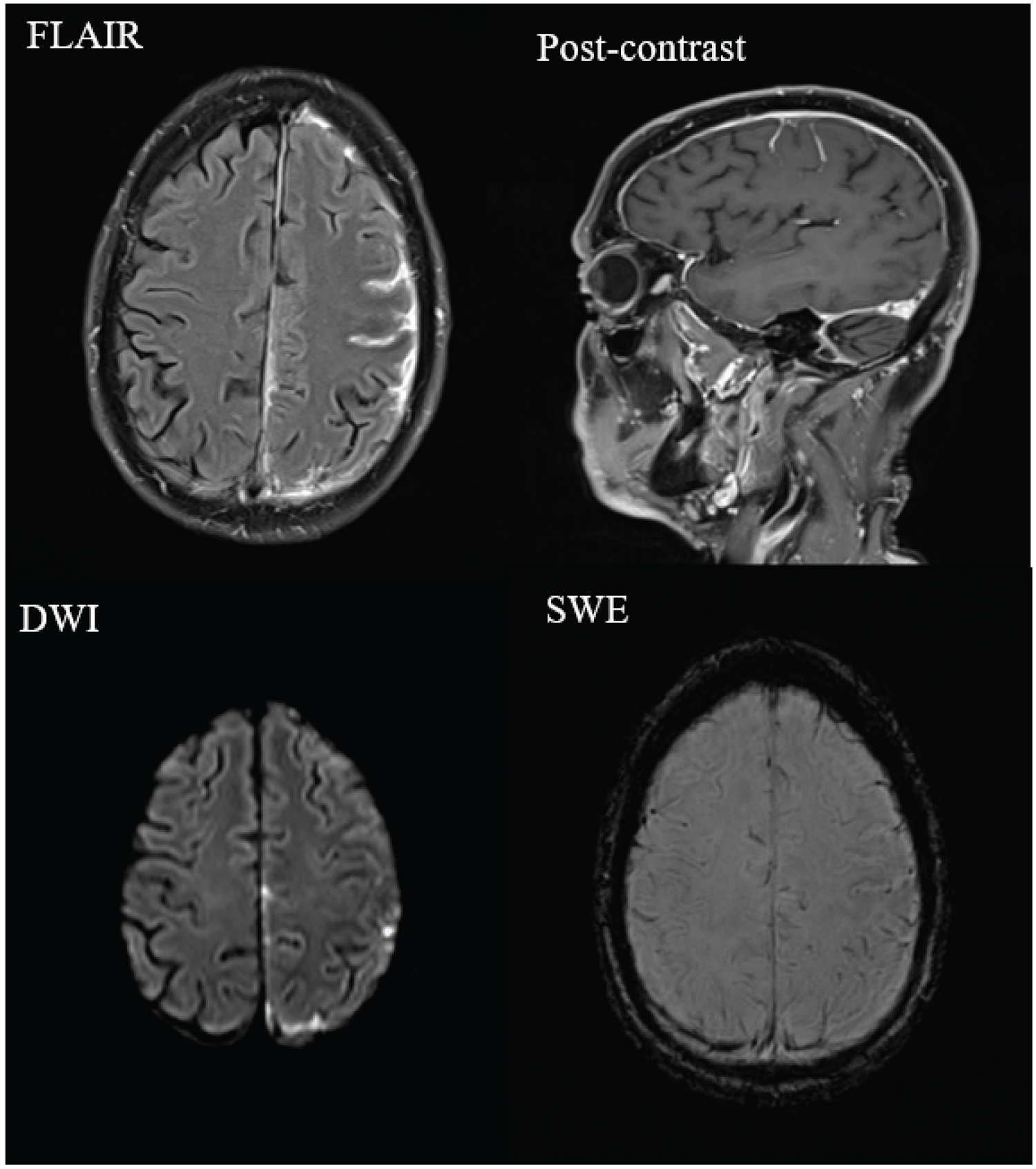
Figure 1: Progress MRI demonstrates left cortical enhancing nodular pachymeningeal and leptomeningeal thickening pre-operatively.
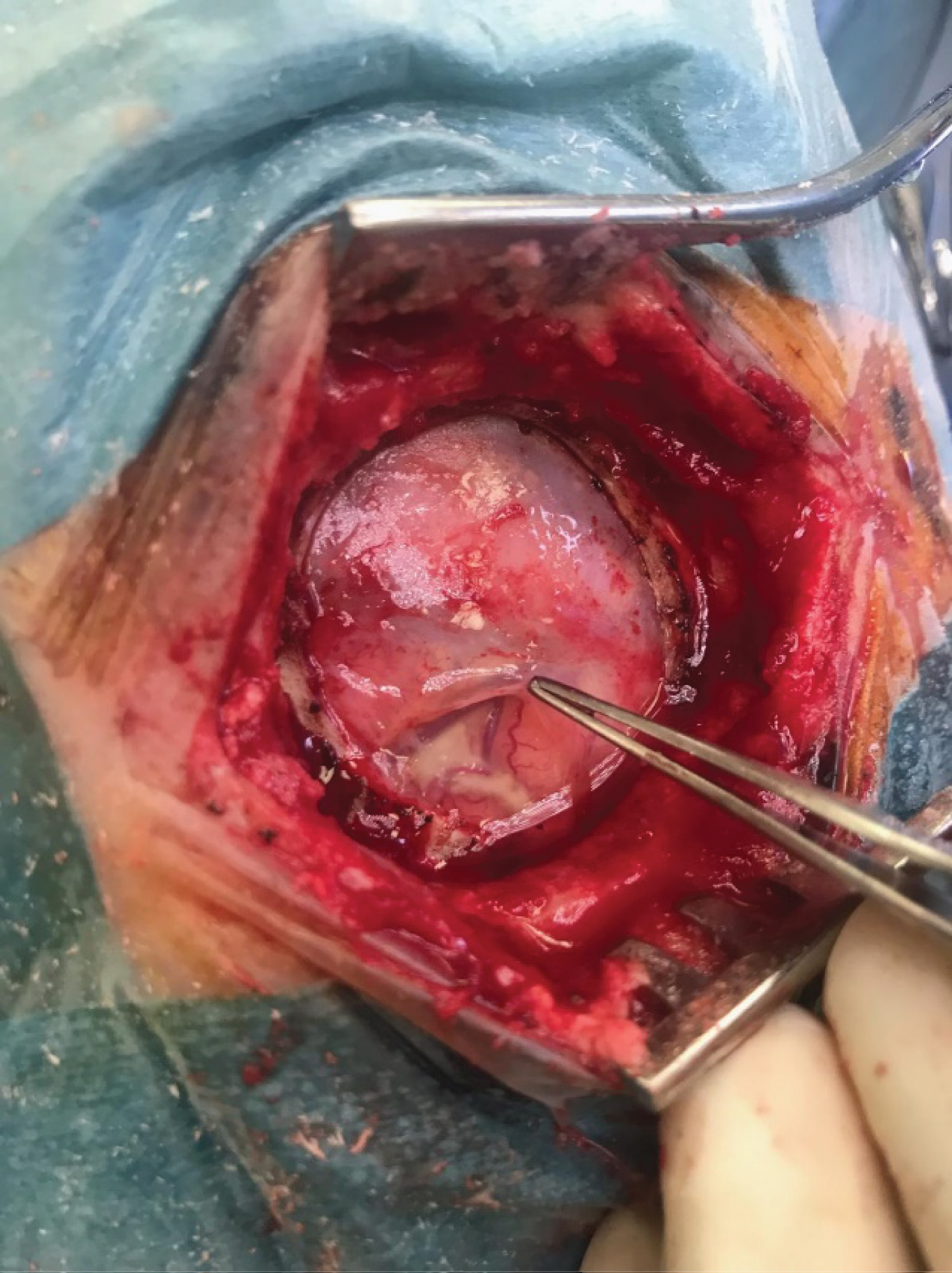
Figure 2: Intra-operative photograph demonstrating normal appearing cortex with purulent material visualised in the sulci.