A previously healthy 9-year-old girl presented with a 3-day history of high fever (> 40 °C) and acute pain in the right shoulder. A blood chemical profile showed a C-reactive protein level of 9.7 mg per liter and a white cell count of 12,500 per cubic millimeter. Shoulder radiographs were normal, but magnetic resonance imaging showed acute osteomyelitis around proximal humeral epiphyseal plate and a subperiosteal abscess around the humeral neck (Figure 1). Vancomycin was empirically started after blood cultures taken. The blood cultures grew Methicillin-Susceptible Staphylococcus aureus (MSSA) and the antibiotherapy was de-escalated to cefazolin. After 1 week of parenteral antibiotics [1], she still had high fever and C-reactive protein level and white cell count were getting worse. Therefore, this therapy was considered ineffective and surgical management was required to control the infection [2]. A deltopectoral approach was used to drain the subperiosteal abscess, and resection was performed (Figure 2). The abscess cultures also revealed MSSA growth. Her shoulder pain and fever rapidly improved 2 days after surgery. At 2 weeks of surgery, blood chemical profiles were normal and blood cultures were negative. She recovered well and there has been no recurrence since a year.
MSSA is definitely the most frequent pathogen responsible for pediatric acute osteomyelitis; the gold standard of antibiotic therapy is usually effective. Surgical treatment should be considered for the patients who do not respond to antibiotic therapy such as those with a subperiosteal abscess [2]. Since the shoulder joint is tightly encapsulated, quick arthrotomy to decrease intraarticular pressure and prevent avascular necrosis is recommended [1]. Early surgical treatment effectively resolved subperiosteal abscess with pediatric acute osteomyelitis to prevent spillover into the joint and subsequent growth cartilage damage.
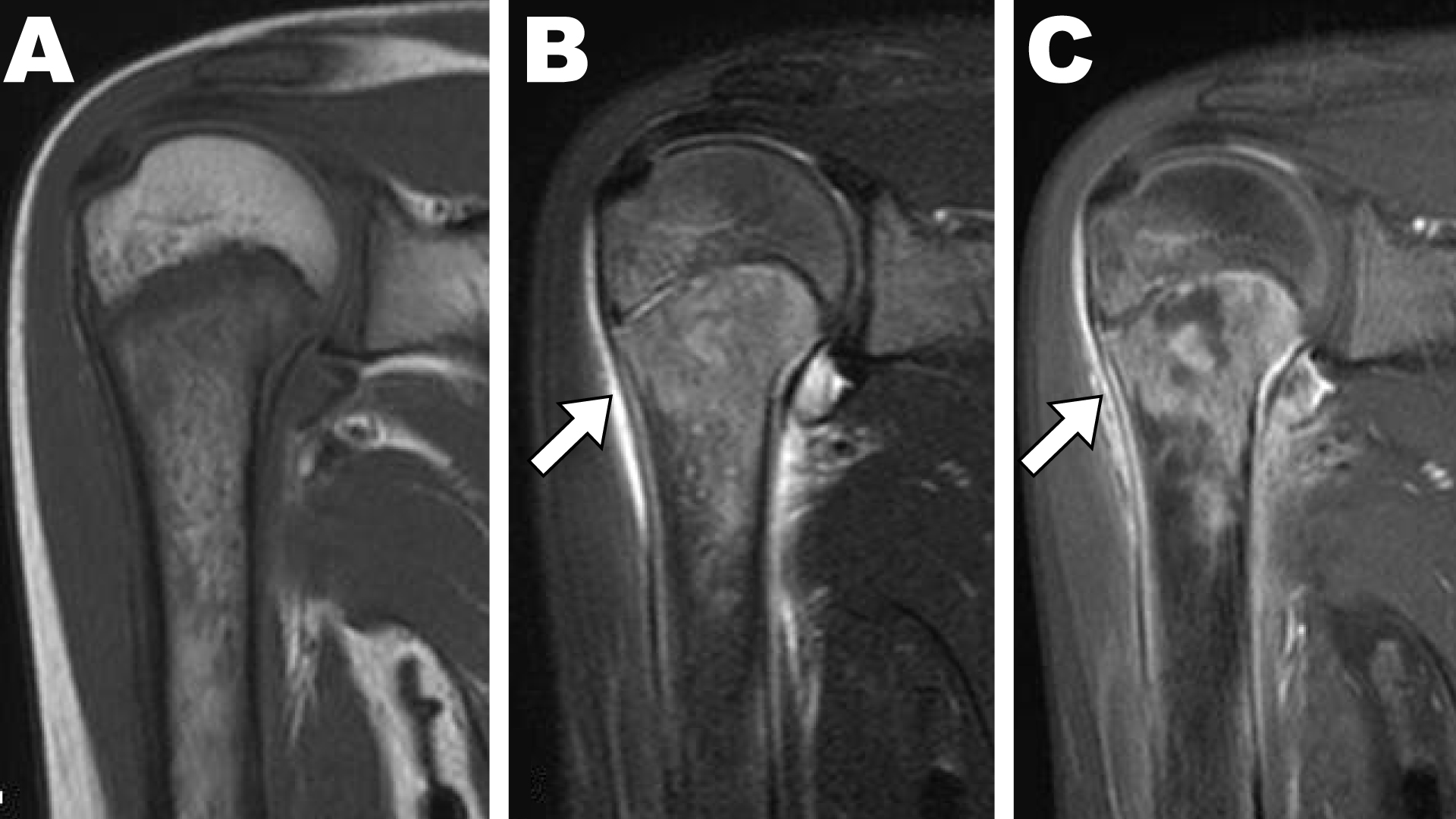
Figure 1: Contrast-enhanced T1-weighted magnetic resonance imaging showed high signal intensity in the proximal humerus and a subperiosteal abscess (white arrow) around the medial humeral neck. T1-weighted (T1w) Turbo Spinecho Imaging (TSE) showed low signal intensity; (A) T2-weighted (T2w) TSE showed high signal intensity; (B) around proximal humeral epiphyseal plate. Contrast-enhanced T1w magnetic resonance imaging (C) T2w TSE showed high signal intensity around humeral neck (arrow).
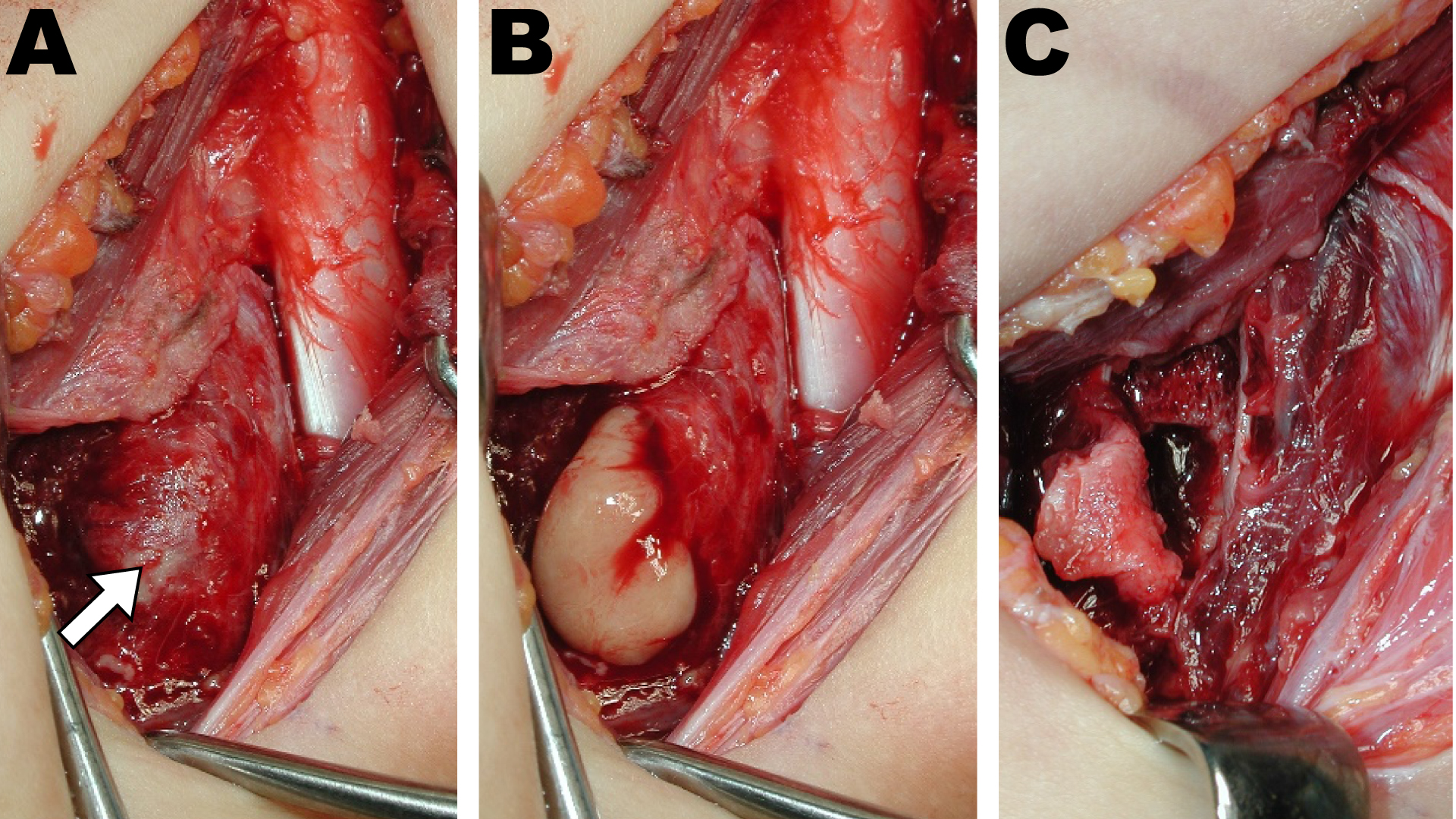
Figure 2: The subperiosteal abscess was identified intraoperatively (A, arrow) and resection was performed (B: during resection, C: after resection).