Cannabis and synthetic cannabinoids have been associated with cardiovascular events including myocardial infarction, arrhythmias, and stroke. The psychoactive cannabinoid delta-9-tetrahydrocannabinol (THC) is a partial agonist for cannabinoid receptors found in the brain, vascular endothelium, liver, and adipose tissue. THC has been implicated in cases of cannabis arteritis and vasculopathy. We describe a case of acute renal artery infarction following synthetic cannabinoid ingestion, with successful thrombolysis and revascularization.
Marijuana, or cannabis, is one of the most widely used psychoactive substances in the world. Its use continues to increase with its legalization in several states. Cannabis and synthetic cannabinoids have been associated with cardiovascular events including myocardial infarction, arrhythmias, and stroke. The psychoactive cannabinoid delta-9-tetrahydrocannabinol (THC) is a partial agonist for cannabinoid receptors found in the brain, vascular endothelium, liver, and adipose tissue. THC has been implicated in cases of cannabis arteritis and vasculopathy. Clinicians must be aware of potential cannabis-related complications to inform patients about risks of cannabis and synthetic cannabinoid use.
A 22-year-old African American male college student presented with acute abdominal pain radiating to the right flank with associated fever, dark urine, and non bilious non bloody vomiting. There was no dysuria or change in bowel habits. Medical history was notable for nephrotic syndrome due to biopsy-proven minimal change disease diagnosed at age 17, which was in remission with the use of tacrolimus and prednisone. He had ingested synthetic cannabinoids the night before, and experienced a brief episode of diaphoresis, palpitations, and anxiety. Exam was notable for right CVA tenderness. Labs were remarkable for leukocytosis of 17,400/microliter and microscopic hematuria. Urine protein to creatinine ratio suggested proteinuria of 1.2 g/day. Cardiolipin antibodies and homocysteine levels were not elevated. Factor V Leiden and prothrombin gene G20210A mutation was negative. Abdominal CT with contrast showed an acute right kidney infarction, and the patient was placed on heparin gtt (Figure 1). Angiography showed an 18 mm thrombus in the distal aspect of the right main renal artery, with impaired perfusion to the superior two-thirds of the kidney but sparing of the inferior pole due to an accessory renal artery (Figure 2) [1-6].
The patient underwent catheter-directed thrombolysis. Follow-up angiography 24 hours after thrombolysis demonstrated thrombus resolution and revascularization of two additional segmental renal arteries. The patient was discharged on enoxaparin and warfarin after 6 days of hospitalization (Figure 3).
Renal artery thrombosis with acute renal infarction is extremely rare, and is typically associated with atrial fibrillation or hypercoagulable states. Management involves intravenous heparin and blood pressure control with angiotensin-converting-enzyme inhibitors or angiotensin II receptor blockers. Thrombolysis and thrombectomy is supported primarily by case reports, but there are no clear guidelines on its use in the treatment of renal artery thrombosis. The duration of anticoagulation is not well defined.
While nephrotic syndrome is a hypercoagulable state, venous thrombosis is more common than arterial events, 1 and this patient's minimal change disease was in remission. The psychoactive cannabinoid delta-9-tetrahydrocannabinol (THC) is a partial agonist for cannabinoid receptors found in the brain, vascular endothelium, liver, and adipose tissue, and has been implicated in cases of cannabis arteritis and vasculopathy. The underlying mechanisms may include autonomic dysfunction, platelet activation, and endothelial damage. Cannabis and synthetic cannabinoids have been associated with cardiovascular events including myocardial infarction, arrhythmias, and stroke. Clinicians must be aware of potential cannabis-related complications to inform patients about risks of cannabis and synthetic cannabinoid use.
This project was not funded by any entity. The authors have no financial conflicts to disclose.
Joyce Ho and Remus Popa contributed to writing, editing, and image review. Youhanna Gad contributed with image acquisition and review.
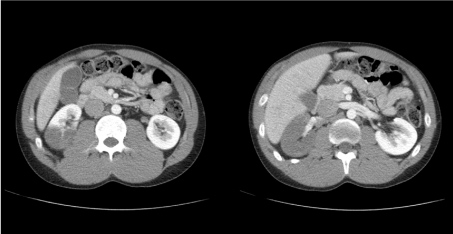
Figure 1: Contrast CT of abdomen and pelvis. Axial view demonstrating showing acute right kidney infarction, with sparing of the inferior pole.

Figure 2: Contrast CT of abdomen and pelvis. Coronal view demonstrating showing acute right kidney infarction, with sparing of the inferior pole.
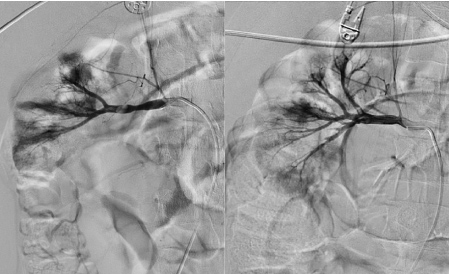
Figure 3: Renal angiography. Angiography before (left) and 24 hours after catheter-directed TPA (right) showing revascularization of segmental renal arteries.