Chronic Kidney Disease (CKD) is an increasing global public health problem and usually occurs as a silent disease, often diagnosed in advanced stages of renal dysfunction. An estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m2 and/or markers of kidney damage for > 3 months are the criteria that define CKD. Among the markers of kidney damage, urine sediment abnormalities are a simple means to facilitate the diagnosis of CKD.
Urine sediment images were obtained with SediMAX® conTRUST PRO. The images provided were both in phase contrast and bright field.
SediMAX® conTrust PRO, a new automated sediment analyzer, with concomitant bright field and phase contrast microscopy enables the best interpretation of the CKD urine sediment abnormalities in terms of quality, detail, and definition of the urine elements.
Automated urinalysis, Phase contrast urine microcopy, sediMAX conTRUST PRO, Urine sediment, CKD
Chronic Kidney Disease (CKD) is an increasing global public health problem with a worldwide prevalence of 13.4%, associated with increased risks of cardiovascular morbidity, increased mortality, and/or decreased quality of life [1]. CKD is a silent disease, and kidney function may be greatly reduced before any recognition of the disease occurs. Medical management then must be addressed towards identification, treatment, monitoring, slowing progression, and reducing complications. CKD is defined by the presence of an estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m2 and/or markers of kidney damage for > 3 months. The markers of kidney damage are: albuminuria, urine sediment abnormalities, electrolyte and other abnormalities due to tubular disorders, abnormalities detected by histology, structural abnormalities detected by imaging, and a history of kidney transplantation [2].
In the patients with eGFR below 60 mL/min/1.73 m2 the urine sediment, defined as a non-invasive "liquid biopsy", is a very simple means of obtaining CKD diagnosis [3]. Indeed, according to the 2012 KDIGO guideline2, the observation of any of the following urinary sediment alterations: isolated non-visible (microscopic) hematuria with abnormal red blood cell (RBC) morphology in glomerular basement membrane disorders; RBC casts in proliferative glomerulonephritis; white blood cell (WBC) casts in pyelonephritis or interstitial nephritis; oval fat bodies or fatty casts in diseases with proteinuria; granular casts and renal tubular epithelial cells in many kidney parenchymal diseases, further defines the presence of CKD. Manual microscopy represents the working tool for urine sediment analysis. Bright field microscopy is widely performed in central laboratories to screen for kidney disease. However, visualization and identification of low-refractile particles (hyaline casts, ghost cells), and of morphologic cell details such as, dysmorphic erythrocytes, renal tubular epithelial cells, atypical/malignant urothelial cells, are not clear with bright field microscopy (Figure 1 and Figure 2) [4,5]. Phase contrast microscopy greatly improves the visualization of the afore mentioned details and allows for higher level testing. Nonetheless, bright field microscopy provides a better resolution of the tridimensional morphology of crystals [4] and lipid droplet contours compared to phase contrast microscopy (Figure 3 and Figure 4).
Recently, automated systems have become extensively applied to urine particle analysis. This has determined standardization of the testing process by eliminating the steps (centrifugation, supernatant elimination, etc.,) of manual microscopy that introduce variability. Furthermore, automation has various other advantages: it allows for electronic transmission, storage, and interpretation of data. Among the automated systems, a new analyzer, sediMAX® conTRUST PRO (77 Elektronica, Budapest, Hungary; distributed in Italy by A. Menarini Diagnostics, Florence, Italy), is now available providing simultaneous automated phase contrast and bright field microscopy. SediMAX® conTrust PRO is a cuvette-based urine sediment analayzer of the sediMAX® series. An advanced built-in digital camera provides both a bright field and a phase contrast microscopic image from the same viewfield. By default 15 high resolution digital gray scale images are taken from different locations on a disposable cuvette bearing urine. These correspond to a total of 2.2 μL of native urine for each sample. In parallel with the analysis of the sample, a special neural based evaluation module of the sediMAX® conTRUST PRO controls the process, recognizes, and classifies the urine particles [6].
In conclusion, the integration of bright field and phase contrast microscopy by sediMAX® conTrust PRO, enables the best interpretation in terms of quality, detail, and definition of the urine particles of a specific sediment during on screen revision of the images. This consents a rapid identification of the urine sediment abnormalities that are present in CKD.
No.
No.
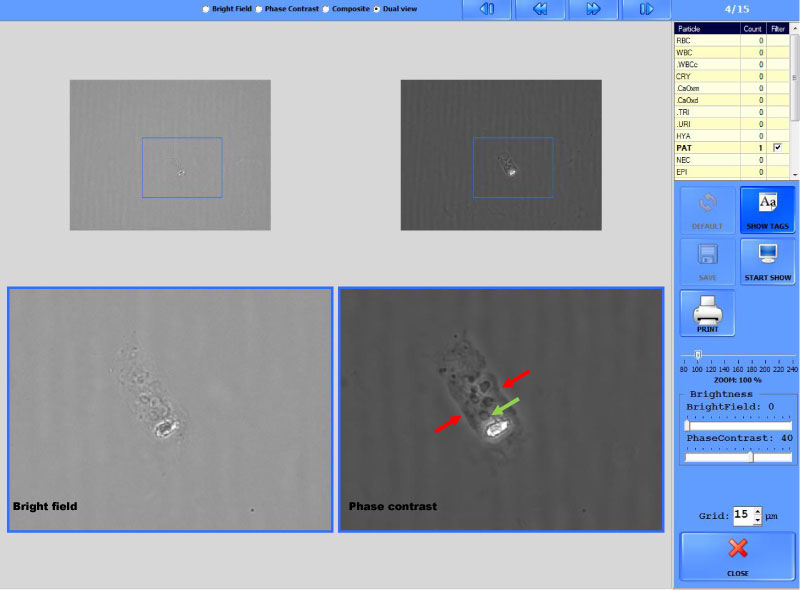
Figure 1: RBC cast: the phase contrast image enhances the cast margins and the RBCs inside the cast.
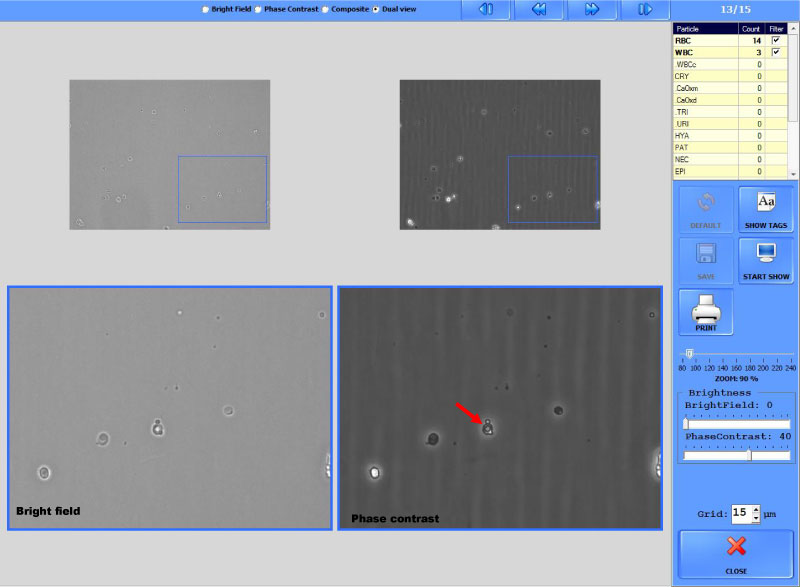
Figure 2: Acanthocytes: the phase contrast image accentuates the ring structure of the acanthocyte.
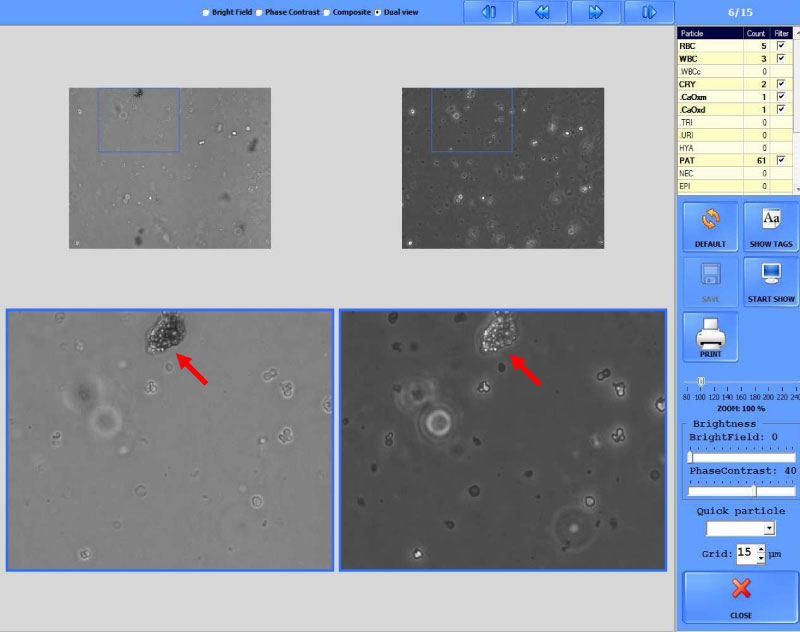
Figure 3: Oval fat body: The bright field image in the Dual View option provides a sharper definition of the fat droplet contour than the phase contrast image.
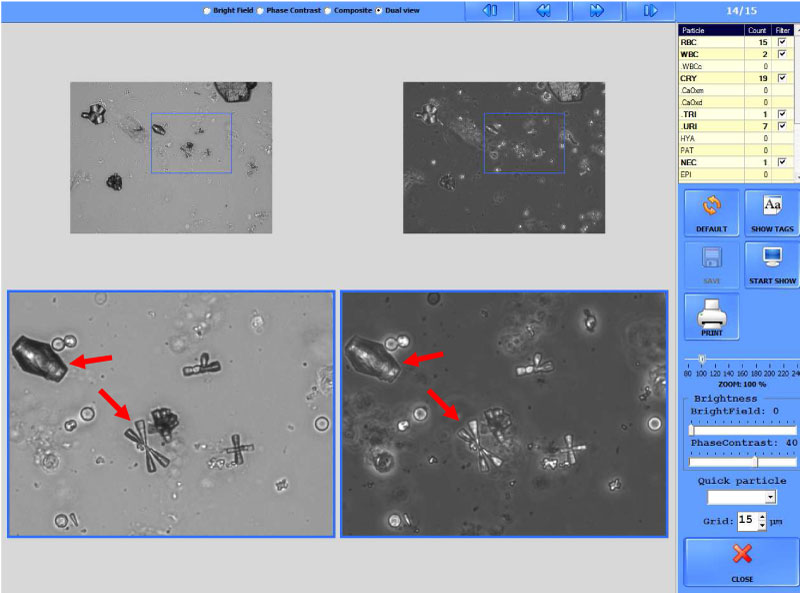
Figure 4: Uric acid crystals: The bright field image accentuates the tridimensional morphology of the crystals.