Neonatal hemangioma, Vascular mass, Vascular tumor, Newborn
A male newborn with a gestational age of 39 weeks and 2 days, with appropriate weight for gestational age, was born by eutocic delivery. Pregnancy surveillance was unremarkable, with maternal serologies and obstetric ultrasounds considered normal. In the delivery room, an adherent red-violaceous rounded lesion in the left gluteal region, with hard consistency, peripheral pale halo and telangiectasias, measuring approximately 5 cm, was observed (Figure 1). The newborn was clinically well, the physical examination was otherwise normal and there were no other skin lesions. Complete blood count and coagulation factor tests were normal, excluding Kasabach-Merritt phenomenon. Ultrasound revealed a solid, heterogeneous, hyperechoic, bulky mass with imprecise limits and extent in depth, involving the muscular and subcutaneous compartments. Doppler study showed hypervascularity and a few large vessels with high flow. No other masses in the pelvic cavity or signs of anchored marrow were observed. Magnetic resonance angiography revealed a lesion with a pyramidal configuration with 5.3 cm of majoraxis, occupying the subcutaneous region and the internal side of the large and medial gluteus, causing a shift of the median raphe, rectum and anus to the right (Figure 2), suggesting a congenital or infantile hemangioma. Periodic follow-up was scheduled and, at 1 month of age, the infant was clinically well, and the lesion had similar characteristics and size. Thus, ongoing clinical surveillance was continued.
Vascular anomalies are common in newborns and can be a challenging diagnosis as they cover a heterogeneous spectrum of disorders [1]. There are two main categories: Vascular neoplasms and vascular malformations. Vascular malformations are vascular structural anomalies with no neoplastic proliferation of endothelial cells. They are usually present at birth and grow proportionally with the child [2-5]. Vascular tumors represent neoplastic growth of vascular endothelial cells, and only a few are usually present at birth, including infantile and congenital hemangiomas [2]. Infantile hemangiomas are the most common benign tumors of infancy, with a median age of appearance of 2 weeks of life, although some may be noted as a telangiectatic stain or ecchymotic area at birth [2,3]. These lesions have a predictable life cycle, with a proliferative phase of rapid growth over the course of a few months, and an involuting phase that generally begins at 9-12 months and occurs slowly over months to years [2,3]. Most infantile hemangiomas are uncomplicated and do not require treatment [2]. After involution, a residual lesion may be present, such as scarring, redundant skin or anetoderma [3]. In contrast, congenital hemangiomas are benign vascular tumors fully grown at birth, that do not manifest postnatal growth [3]. Congenital hemangiomas present as red-violaceous, bossed plaques or exophytic masses, with coarse telangiectasias, central pallor, and a peripheral pale halo [3]. The head, neck or limbs are the most common locations. They are divided in two major subtypes: Rapidly involuting congenital hemangiomas (RICH) and noninvoluting congenital hemangiomas (NICH), that differ by their natural course. RICH involute completely at around one year of age, while NICH are permanent lesions. A third subtype, partially involuting congenital hemangioma (PICH), is characterized by incomplete regression and posterior stabilization [4-6]. Once involuted, RICH does not leave behind a residual abnormality. In parallel to infantile hemangiomas, most congenital hemangiomas do not require treatment. Imaging appearance of infantile and congenital hemangiomas may overlap, but there are some recognizable differences [2]. On the ultrasound, congenital hemangiomas show greater internal heterogeneity, and less well-circumscribed margins, while infantile hemangiomas present as well-defined ovoid or elongated lesions of the subcutaneous fat with mildly lobulated margins. Color Doppler ultrasound of congenital hemangiomas displays a high vascular density with both arterial and venous flow, and infantile hemangiomas show an abundance of vascular flow within the lesion [2]. On magnetic resonance imaging, congenital hemangiomas are more likely than infantile hemangiomas to demonstrate internal heterogeneity, with intermediate to low T2 signal intensity [2,7].
In some cases, physical examination and history are sufficient to accurately establish a diagnosis. However, although not always necessary, imaging studies are important to rule outmore serious conditions that require immediate intervention. Once these are dismissed, clinical evolution alone may be enough to establish the diagnosis, avoiding unnecessary therapy and other complementary diagnostic tests. Therefore, it is crucial to maintain a close follow-up by an experienced multidisciplinary center to offer the best diagnostic and therapeutic approach.
None.
All authors contributed equally in the writing.

Figure 1: Red-violaceous rounded lesion in the left gluteal region, with peripheral pale halo and telangiectasias.
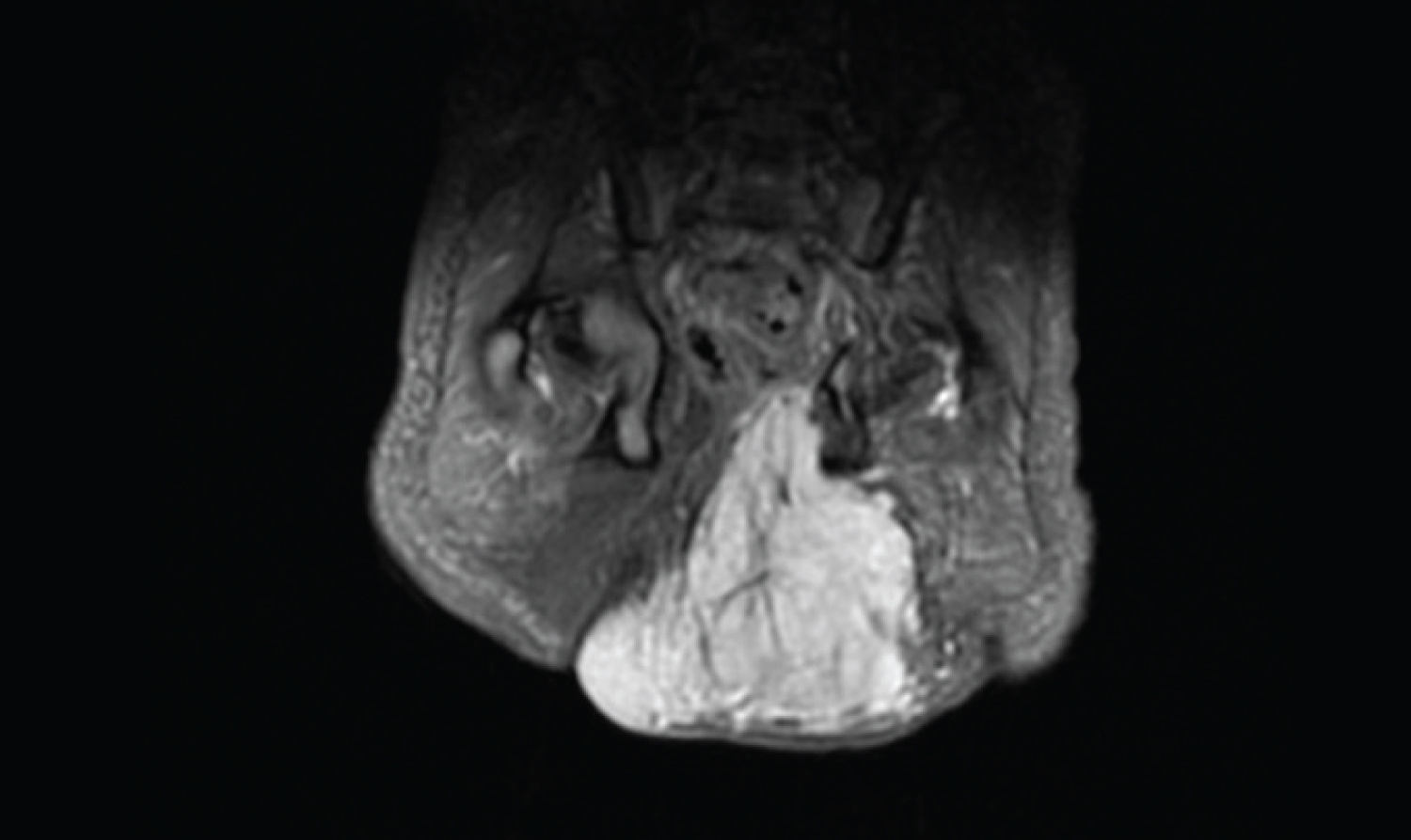
Figure 2: Magnetic Resonance Angiography revealing a lesion with a pyramidal configuration with 5.3 cm of major axis, occupying the subcutaneous region and the internal side of the large and medial gluteus, causing a shift of the median raphe, rectum and anus to the right.