Background: Localization of mandibular foramen (MF) determines the success of inferior alveolar nerve block (IANB).
Methods: The location of MF was determined in 273 scans using I-CAT machine. Cone beam computed tomography (CBCT) scans were of 104 males (38.10%) and 169 females (61.90%) were assessed. The MF location was analyzed by measuring the following distances: Distance from midpoint of anterior margin of MF to the nearest point on anterior border of ramus of mandible (AB-MF). Distance from midpoint of posterior margin of MF to the nearest point on the posterior border of the ramus of mandible (PB-MF). Distance from the lowest point of mandibular notch to entering point of MF (MF-MN). Distance from entering point of MF to point of the greatest convexity of the inferior ramus border (MF-IB). Distance from entering point of MF to occlusal plane of mandibular right first and second molars (MF-OP). Distance from entering point of MF to apex of retromolar trigone (MF-ARMT). Two ramus anatomic features were analyzed: Ramus width (RW) and ramus height (RH). Mandibular foramen depth (MFD) and mandibular canal width (CW) were also evaluated. Mann-Whitney U test was used to compare between the mean values of males and females.
Result: Males showed significantly higher values in most of the measurements except MFD and ARTM-MF. Conclusions: In the present study, statistically significant differences in the location of the MF were found between males and females. However, there is no need to change needle insertion in IANB because females have overall smaller mandibles. Smaller distances in every direction compensate for each other.
Mandibular foramen, Inferior alveolar nerve block, CBCT
Mandibular foramen (MF) is the channel where the inferior alveolar nerve (IAN) and vessels pass through to supply the mandible, mandibular teeth and the lower lips with nutrition and sensory perception [1]. The exact localization of MF would decrease failure rates of IANB, as IAN should be anesthetized before entering MF to increase the success rate of IANB [2-4]. Moreover, the location of MF is crucial in planning various mandibular surgeries such as bilateral sagittal split osteotomy to avoid injury of the inferior alveolar bundle.
Inferior alveolar nerve block (IANB) is one of the most common anesthetic techniques used in dentistry [2,3]. IANB is used to anaesthetize the mandibular molars in various dental procedures such as endodontic treatment, extraction as well as different mandibular surgical procedures. Despite its extensive usage, IANB has reported failure rates reaching 20% to 25% [3,5]. Failure of IANB may cause a wide range of interoperative as well as postoperative complications. Interoperative complications include pain during dental procedures and hemorrhage due to injury of inferior alveolar vessels. Postoperative complications comprise hematoma, trismus, fracture of mandible and permanent loss of sensation in mandibular area that may reach morbidity due to injury of inferior alveolar nerves and vessels [2-4]. It is reported that the location of MF is affected by age, sex, loss of teeth and ethnicity [2,6,7].
Previous studies suggested a considerable debate about the variation of location of MF regarding sex. Iranian and Turkish previous studies reported significant differences in various measurements in location of MF regarding sex [4,8]. While Canadian and Jordanian had demonstrated no significant difference in the location of MF according to sex [6,9]. Therefore, In the current study, we aimed to locate the position of MF in a sample of Egyptian males and females using CBCT. The ultimate goal is to increase the success rate of IANB.
CBCT was the tool chosen to locate the position of MF in this study. The MF cannot be clinically palpated [6,8,9], therefore previous studies have investigated it's exact location using dried human mandibles [9,10], or conventional panoramic and cephalometric radiographs [9] and computed tomography (CT). Compared to conventional radiography, CBCT is more accurate in localization of various anatomical structures with limited distortion. Moreover, it exhibited more accuracy, higher resolution, lower scan time, and lower radiation doses compared to conventional CT imaging [6]. In the current study, we aimed to locate the position of MF in a sample of Egyptian males and females using CBCT. The ultimate goal is to increase the success rate of IANB.
The study was exempted from review by the research Ethics committee of the university of Ain Shams, exemption number FDASU-Rec EM012202. A total sample of 273 CBCT scans; 104 males (38.10%) and 169 females (61.90%) patients with age ≥ 18 years old were collected from three institutes in two Egyptian governorates (Maxillofacial Radiology department of Ain Shams university and Canadian university in Cairo and 3D dental radiology center in Mansoura). This retrospective study was performed on scans obtained by I-CAT Next Generation machine (Imaging Sciences International, Hatfield, Pennsylvania, USA) with the following scanning parameters; tube voltage of 120 KVp, tube current of 36.12 mA/s and 26.9 seconds scanning time and 16 × 8 FOV) between May 2017 and December 2021. Patients with syndromic craniofacial deformity or with mandibular fracture were excluded. CBCT scans having artifact/s or with limited field of view were also excluded. All the measurements were taken by two radiologists with 10 years of experience.
On I-CAT vision software program the following measurements were executed on the right side of the mandible of each scan:
• AB-MF: Distance from midpoint of anterior margin of mandibular foramen to the nearest point on anterior border of ramus of mandible.
• PB-MF: Distance from the midpoint of posterior margin of mandibular foramen to the nearest point on the posterior border of the ramus of mandible.
• CW: Distance from anterior border to posterior border of mandibular foramen passing through midpoint of mandibular foramen.
• MF-MN: Distance from the lowest point of mandibular notch to the entering point of mandibular foramen.
• MF-IB: Distance from the entering point of mandibular foramen to the point of the greatest convexity of the inferior ramus border.
• MFD: Depth of the mandibular foramen.
• MF-OP: Distance from entering point of mandibular foramen to occlusal plane of mandibular right first and second molars.
• MF-ARMT: Distance from entering point of mandibular foramen to the apex of the retromolar trigone.
• RW: Distance from anterior border of ramus to posterior border of ramus passing by midpoint of mandibular foramen.
• RH: The minimum distance from lowest point of mandibular notch and point of greatest convexity of inferior ramus border passing by entering point of mandibular foramen.
For the purpose of the present study, these are the definitions of the following anatomical terms:
Occlusal plane: A plane that touches the cusps of mandibular right first and second molars and extends to reach the posterior border of the right mandibular ramus below the level of the midpoint of mandibular foramen. Midpoint of mandibular foramen: The most superior point of the mandibular foramen. Entering point of mandibular foramen: The point that divides the mandibular foramen into two equal parts and is found at the lower border of mandibular foramen. It represents the point of needle insertion. Retromolar trigone: Is a triangular area bounded by the temporal crest on the medial side and the anterior border of ramus on the lateral side. The base of the triangle lies posterior to the socket of the third molar.
Multi-planar images (MPR) were used to obtain the linear measurements. Standardization was performed on two MPR views and then the measurements were taken on the third plane. The slice thickness was increased to 8 mm to include all structures needed.
To measure distances AB-MF, PB-MF, RW, CW, MN-MF, MF-IB and RH, standardization was done as follows: In the coronal view, the axial plane was scrolled upwards till reaching the axial slice that shows the beginning of complete separation between mandibular condyle and coronoid processes. In the axial view, the view rotated till the condyle and coronoid became tangent, then the sagittal plane was moved to pass through both the condyle and the coronoid as illustrated in (Figure 1A). In the axial view, the coronal plane was scrolled to attain complete visualization of the mandibular foramen. In the coronal view, the view rotated till MF buccal wall became parallel to sagittal plane, then the sagittal plane was then adjusted to pass through the buccal wall of the mandibular foramen as illustrated in (Figure 1B). Thus, a standardized sagittal view is obtained from which accurate measurements were obtained as illustrated in (Figure 1C).
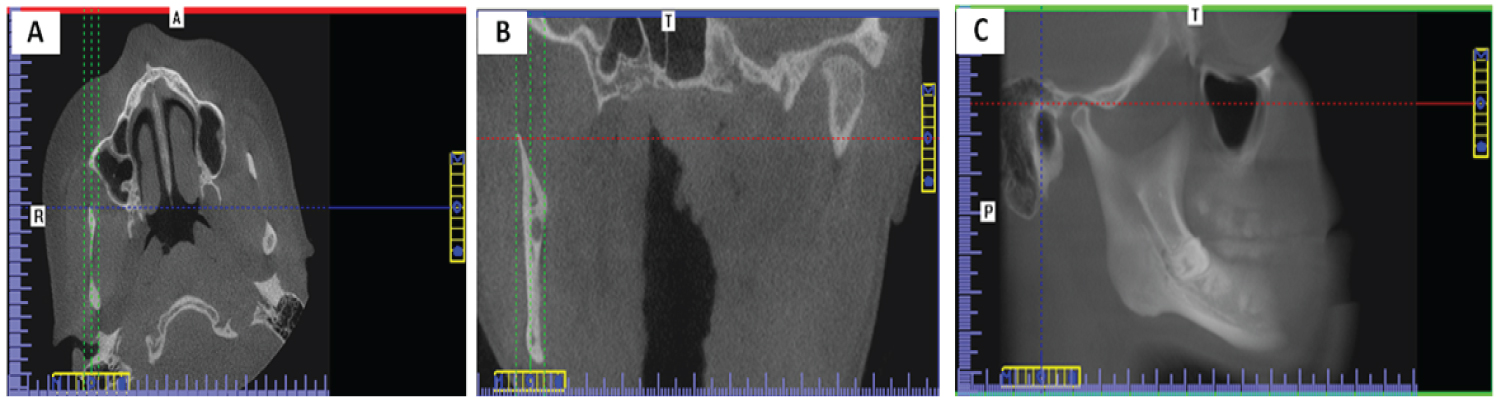 Figure 1: A) Standardization of axial view on I-CAT Vision software that showed the beginning of complete separation between mandibular condyle and coronoid processes. The axial view was rotated till the condyle and coronoid became on the same plane, and the sagittal plane was moved to pass through both the condyle and the coronoid; B) Standardization of coronal view on I-CAT Vision software that showed the start of complete visualization of the mandibular foramen. The coronal view was rotated till the buccal wall of MF was parallel to the sagittal plane. The sagittal plane was then adjusted to pass through the buccal wall of the mandibular foramen; C) Corrected Sagittal view on I-CAT Vision software was obtained from which accurate measurements can be obtained.
View Figure 1
Figure 1: A) Standardization of axial view on I-CAT Vision software that showed the beginning of complete separation between mandibular condyle and coronoid processes. The axial view was rotated till the condyle and coronoid became on the same plane, and the sagittal plane was moved to pass through both the condyle and the coronoid; B) Standardization of coronal view on I-CAT Vision software that showed the start of complete visualization of the mandibular foramen. The coronal view was rotated till the buccal wall of MF was parallel to the sagittal plane. The sagittal plane was then adjusted to pass through the buccal wall of the mandibular foramen; C) Corrected Sagittal view on I-CAT Vision software was obtained from which accurate measurements can be obtained.
View Figure 1
Measurements of AB-MF, PB-MF, RW, CW, MN-MF and MF-IB on the standardized sagittal view are illustrated in (Figure 2A, Figure 2B, Figure 2C, Figure 2D, Figure 2E and Figure 2F) sequentially. The ramus mandibular height (RH) was calculated by adding distances MN-MF and MF-IB from (Figure 2E and Figure 2F).
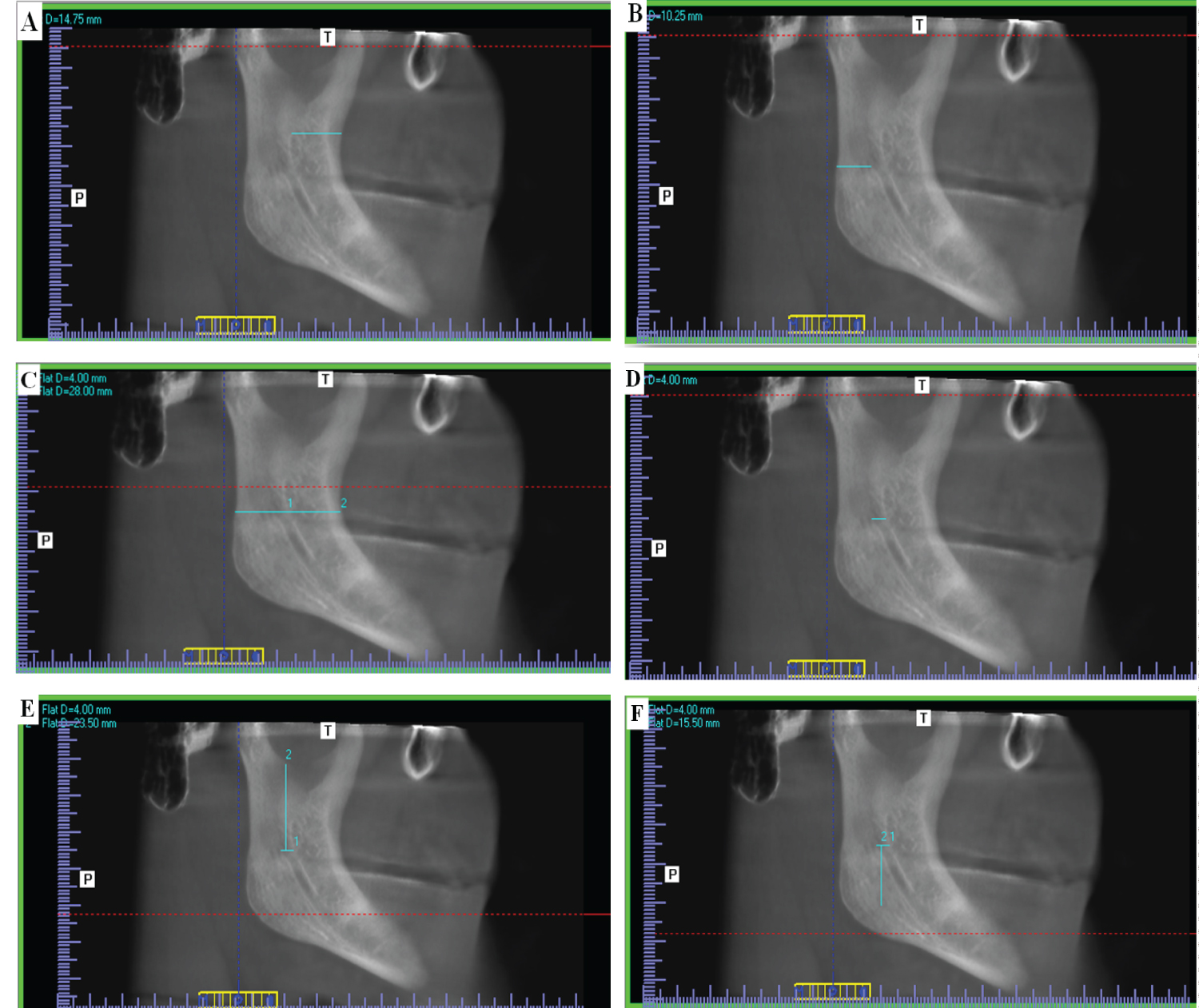 Figure 2: Corrected sagittal view on I-CAT vision software in a forty-three years dentate female showing the following measurements. A) Distance from midpoint of anterior margin of mandibular foramen to the nearest point on anterior border of ramus of mandible AB-MF; B) Distance from the midpoint of posterior margin of mandibular foramen to the nearest point on the posterior border of the ramus of mandible PB-MF; C) RW; D) Distance from anterior border to posterior border of mandibular foramen passing through midpoint of mandibular foramen CW; E) Distance from the lowest point of mandibular notch to the entering point of mandibular foramen MF-MN; F) Distance from the entering point of mandibular foramen to the point of the greatest convexity of the inferior ramus border MF-IB.
View Figure 2
Figure 2: Corrected sagittal view on I-CAT vision software in a forty-three years dentate female showing the following measurements. A) Distance from midpoint of anterior margin of mandibular foramen to the nearest point on anterior border of ramus of mandible AB-MF; B) Distance from the midpoint of posterior margin of mandibular foramen to the nearest point on the posterior border of the ramus of mandible PB-MF; C) RW; D) Distance from anterior border to posterior border of mandibular foramen passing through midpoint of mandibular foramen CW; E) Distance from the lowest point of mandibular notch to the entering point of mandibular foramen MF-MN; F) Distance from the entering point of mandibular foramen to the point of the greatest convexity of the inferior ramus border MF-IB.
View Figure 2
To measure distance MFD, In the coronal view, the axial plane was scrolled till the slice just before which the foramen is completely surrounded by bony cortex. In the axial view, the view was rotated till MF buccal wall became parallel to sagittal plane, then the distance from the lingual to the buccal border of the mandibular foramen was measured as illustrated in (Figure 3A). (Figure 3B) illustrates measurement of MFD from the standardized sagittal view.
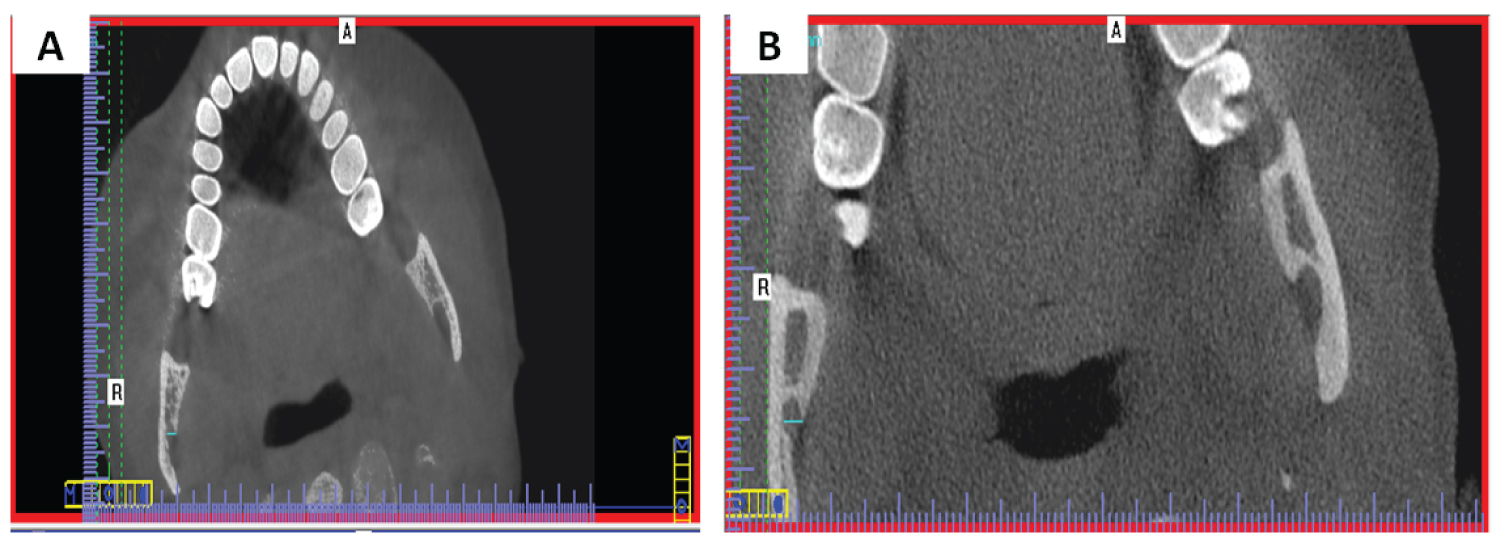 Figure 3: A) Standardization of axial view on I-CAT Vision software to measure MFD. The axial slice just before the mandibular foramen was completely surrounded by a bony cortex was rotated till the buccal wall of the MF became parallel to the sagittal view; B) Measurement of Depth of the mandibular foramen MFD in a forty-three-year-old dentate female on I-CAT vision software.
View Figure 3
Figure 3: A) Standardization of axial view on I-CAT Vision software to measure MFD. The axial slice just before the mandibular foramen was completely surrounded by a bony cortex was rotated till the buccal wall of the MF became parallel to the sagittal view; B) Measurement of Depth of the mandibular foramen MFD in a forty-three-year-old dentate female on I-CAT vision software.
View Figure 3
To measure distances MF-OP and MF-ARMT, In the coronal view, the axial plane was scrolled up to the slice that shows the widest pulp chamber of the mandibular first molar. In the axial view, the view rotated till the buccal wall of mandibular six parallel to sagittal plane, then the sagittal plane was moved to pass through the lingual wall of the mandibular first molar and also bisect the mandibular ramus as illustrated in (Figure 4A). In the axial view, the coronal plane was scrolled up to the first slice that shows the mandibular foramen completely surrounded by cortical bone. In the coronal view, the view was rotated till MF lingual wall parallel sagittal plane, then the sagittal plane was moved to pass through the lingual wall of the mandibular foramen as well as the mandibular condyle as illustrated in (Figure 4B). (Figure 5A and Figure 5B) show measurement of MF-OP and MF-ARTM from the standardized sagittal view.
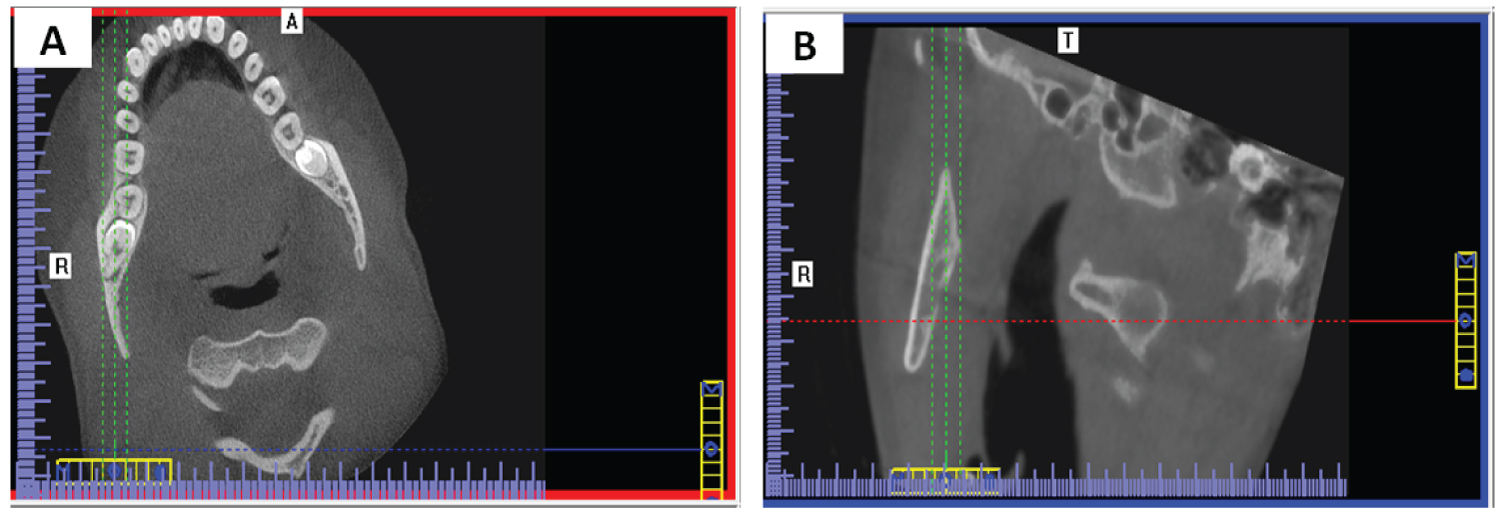 Figure 4: A) Standardization of the axial view on I-CAT Vision software to measure MF-OP and MF-ARMT. The axial view that showed the widest pulp chamber of the mandibular first molar was rotated till the buccal aspect of mandibular first molar became parallel to the sagittal plane. The sagittal plane was then moved to pass through the buccal wall of the mandibular first molar and also bisect the mandibular ramus; B) Standardization of the coronal view that showed the mandibular foramen completely surrounded by cortical bone. The coronal view was rotated till the condyle processes and lingual wall of the MF became on the same plane, and the sagittal plane was moved to pass through the lingual wall of the mandibular foramen as well as the mandibular condyle.
View Figure 4
Figure 4: A) Standardization of the axial view on I-CAT Vision software to measure MF-OP and MF-ARMT. The axial view that showed the widest pulp chamber of the mandibular first molar was rotated till the buccal aspect of mandibular first molar became parallel to the sagittal plane. The sagittal plane was then moved to pass through the buccal wall of the mandibular first molar and also bisect the mandibular ramus; B) Standardization of the coronal view that showed the mandibular foramen completely surrounded by cortical bone. The coronal view was rotated till the condyle processes and lingual wall of the MF became on the same plane, and the sagittal plane was moved to pass through the lingual wall of the mandibular foramen as well as the mandibular condyle.
View Figure 4
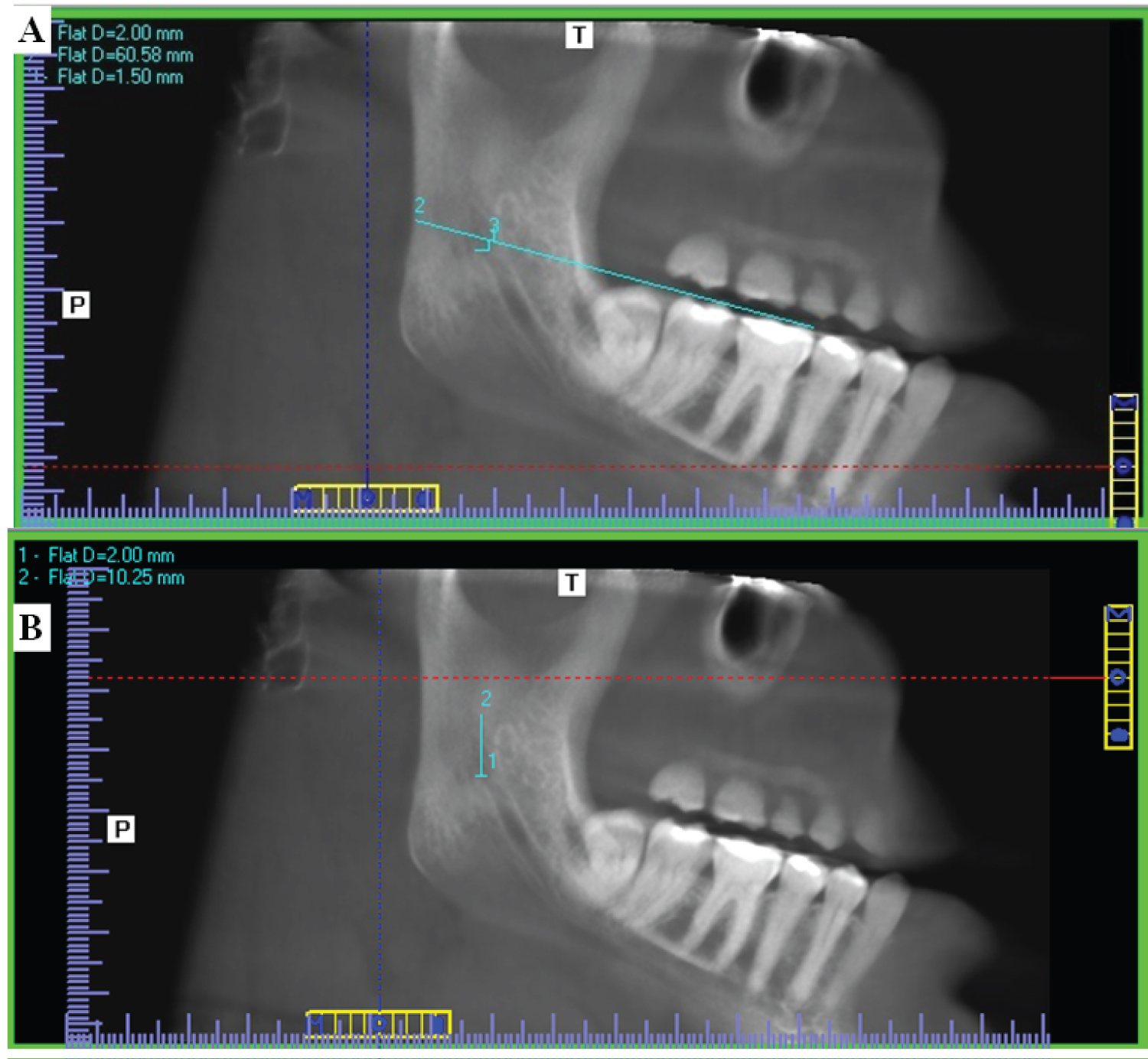 Figure 5: Corrected sagittal view on I-CAT vision software in forty-three years dentate female showing measurements; A) Distance from entering point of mandibular foramen to occlusal plane of mandibular right first and second molars. MF-OP; B) Distance from entering point of mandibular foramen to the apex of the retromolar trigone MF-ARMT.
View Figure 5
Figure 5: Corrected sagittal view on I-CAT vision software in forty-three years dentate female showing measurements; A) Distance from entering point of mandibular foramen to occlusal plane of mandibular right first and second molars. MF-OP; B) Distance from entering point of mandibular foramen to the apex of the retromolar trigone MF-ARMT.
View Figure 5
All data were collected and tabulated. Statistical analysis was performed by IBM SPSS® (version 20), while Microsoft office Excel was used for data handling and graphical presentation. Quantitative variables were described as mean, standard deviation (SD), range, standard error (SE) and 95% confidence interval of the mean. Shapiro-Wilk test was used to test normality hypothesis of all quantitative variables for further choice of appropriate parametric and non-parametric tests. For the present study, the non-parametric Mann and Whitney U test) was applied. Significance level was set at P < 0.05.
Demographic data of the study is presented in Table 1. Significant difference was found between males and females regarding AM-MF, PM-MF, RW, MN-MF, RH, OP-MF, CW and IB-MF, while no significant difference was found regarding MFD and ARMT-MF as presented in Table 2.
Table 1: Shows the demographic data between males and females in the study. View Table 1
Table 2: Comparison of measurements between males and females. View Table 2
Determination of MF location is necessary for the success of various dental procedures. MF is the site of the insertion of the needle during IANB before the nerve hides inside the bone of mandibular canal [6]. IANB is one of the most common techniques used for local anesthetic nerve block of the mandibular molar [2,3]. Despite of the popularity of IANB, it is reported to have high failure rates ranging from 20-25% [3,5]. One of the most popular cause of failure of IANB is lack of awareness of MF location as MF is not palpable intra-orally [2-4]. The location of MF differs according to multiple factors including race, sex, age and loss of teeth [2,6,7]. Therefore, in the present study we analyzed 273 CBCT scans of males and females to localize the location of MF.
In the present study, males and females showed significant differences in the position of MF. Females have smaller values than males in almost all the assessed measurements. Similarly, Enlow, et al. reported that the craniofacial dimensions in the females are 5%-9% less than males. They attributed this to the higher rate and speed of growth in males. Only two measurements showed no significant difference in the location of MF between males and females the mandibular foramen depth (MFD) and the distance between the apex of the retromolar trigone (ARMT) and the mandibular foramen. These two distances are not related to growth rate so are not affected by sex.
In the present study, the distance from midpoint of the anterior margin of MF fossa to the nearest point of the anterior ramus border AB-MF was found to be significantly greater in males than females with means of 17.64 and 16.66 mm. Likewise, Aglarci, et al. reported a significantly higher AB-MF in males than females mean value of 15.5 mm and 14.91 mm respectively [11].
On the other hand, Al-Shayyab, demonstrated that there wasn't a significant difference in AB-MF between male and females with greater value in males (17.71- 17.35 mm respectively) [6]. Trost, et al. also reported no significant difference between sexes regarding AB-MF [12]. They assessed 46 panoramic radiographs of patients ranging in age from 12 to 72 years. The age range in our study was 18 to 68yearsand in females from (18 to 65Y). Afsar, et al. similarly demonstrated that AB-MF is greater in males than females without significant difference. They used oblique cephalometric and panoramic radiographs, a wider age range (10.2-37.5 years) and multiple ethnic origins (Black, Hispanic, Asian and Caucasian) [9]. Lasemi, et al. reported no significant difference between males and females in AB-MF. In that study females even had greater mean values (16.66 mm) than males (16.30 mm) [4]. Their measurements were made on 194 Iranian panoramic radiographs. While we assessed 273 CBCT Egyptian scans. The difference in sample size, type of radiograph and ethnicity of the study participants might explain the disparity of the results.
The distance from midpoint of the posterior margin of MF fossa to the nearest point of the posterior ramus border (PM-MF) was significantly more in males than females with means of 12.56 and 11.85 mm. Likewise, Aglarci, et al. demonstrated that there was a significant difference in PB-MF regarding to sex as male greater than females with mean 13.50-12.60 mm respectively [11].
Afsar, et al. demonstrated that PM-MF was greater in males than females without significant difference [9]. While Trost et al. found no significant difference with sex in the distance (PB-MF) [12]. The discrepancy between our findings might be attributed to their using panoramic radiography, age range 12 to 72 years and a sample size of 46 patients, while we used CBCT to assess 274 patients, ranging in age from 18 to 70 years. Likewise, Al-Shayyab demonstrated that there wasn't significant difference in AB-MF between male and females with greater value in male than females 13.43-12.97 mm respectively [6].
Ramus width defined as the minimum distance between the anterior and posterior borders of the ramus passing by the midpoint of the MF fossa was found to be significantly greater in males than female with a mean of 33.78 and 31.17 mm. To the best of our knowledge, this measurement wasn't previously compared between males and females.
The distance from the lowest point of the mandibular notch to the entering point of MF fossa (MN-MF), was found to be significantly greater in males than females with a mean of 36 and 34.40 mm. Likewise, Aglarci, et al. agreed that there was a significant difference in distance (MF-MN) regarding to sex with mean value greater in males = 17.64 mm and females mean value = 16.62 mm [11]. Opposingly, Afsar, et al. reported no significant difference according to gender with distance (MN-MF) in their study [9]. Also, Al-Shayyab demonstrated that there wasn't significant difference in MN-MF between male and females with greater value in male than females (25.70-25.64 mm respectively).
Ramus height measured as the minimum distance between mandibular notch to the inferior border of the ramus passing by the entering point of MF fossa was found to be significantly longer in males than females with a mean of 49.36 and 43.87 mm successively. To the best of our knowledge, this measurement wasn't previously compared between males and females.
The distance from the midpoint of the mandibular foramen to occlusal plane of mandibular first and second molars (MF-OP) was significantly higher in males than females with a mean of 3.96 and 3.11 mm consecutively. Likewise, Aglarci, et al. demonstrated a significant difference in the distance (MF-OP) among sex with mean value greater in males than females (7.46- 7.19 mm respectively) [11]. Moreover, Lasemi, et al. confirmed the significant difference between male and female regarding MF-OP distance with a mean value greater in males than females (4.75-3.96 mm respectively) [4]. Likewise, Trost, et al. reported a significant difference in MF-OP between genders [12]. Opposingly, Afsar, et al. found no significant difference between males and females regarding MF-OP distance [9]. They used the center of the MF instead of the most superior posterior point as reference point, which explains the difference in values. Likewise, Al-Shayyab demonstrated that there wasn't significant difference in OP-MF between male and females with greater value in male than females (4.65- 4.42 mm respectively) [6].
The canal width described as the distance from the anterior border of MF to the posterior border of MF was found significantly greater in males than females with a mean of 5.22 and 4.49 mm sequentially. To the best of our knowledge, this measurement wasn't previously compared between males and females.
The distance from the entering point of MF fossa to the point of the greatest convexity of the inferior ramus border (IB-MF), was significantly larger in males with a mean of 26.34 and 22.40 mm successively. Likewise, Aglarci, et al. reported a significant difference in the distance (IB-MF) regarding to sex with mean greater in males than females (24.53-23.56 mm respectively) [11]. On other hand Afsar, et al. found no significant difference regarding to sex in (IB-MF) with greater mean value in males than females [9]. Likewise, Al-Shayyab demonstrated that there wasn't significant difference in IB-MF between male and females with greater value in male than females (19.36- 19.10 mm respectively) [6].
The distance from the apex of retromolar trigone to the mandibular foramen (ATRM-MF) showed no significance difference between males and females with a mean of 9.47 and 9.36 mm sequentially.
The depth of the mandibular foramen fossa depression (MFD) also presented no significance difference according to sex in our study with a mean of male = 3.13 and female = 3 mm. Likewise, Aglarci, et al. reported no significant difference in the value of the MFD according to sex with mean value of male = 7.02 mm and mean value of female = 6.92 mm [11].
In the present study, statistically significant differences in the location of the MF were found between Egyptian males and females, like their Turkish and Iranian counterparts. However, there is no need to change needle insertion in IANB because females have overall smaller mandibles. Smaller distances in every direction compensate for each other. Canal width is significantly narrower in females, but this will not affect IANB needle insertion.
The authors deny any conflicts of interest.